Bitemporal Hemianopia: Causes, Symptoms, and Management
What Is Bitemporal Hemianopia?
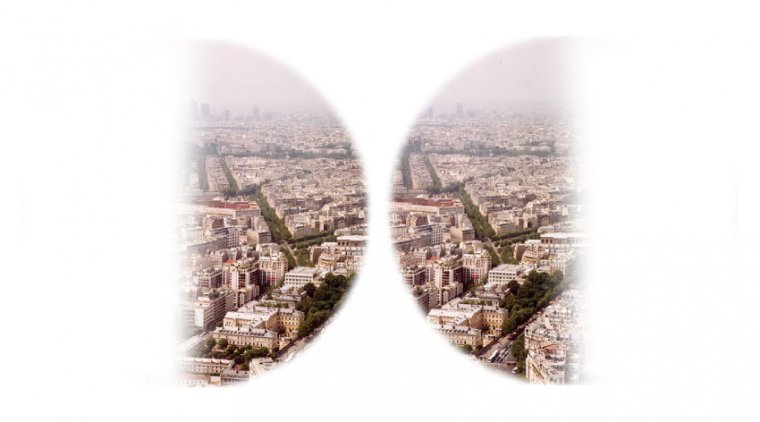
Bitemporal hemianopia, also known as bitemporal heteronymous hemianopia, is a visual field defect that affects both eyes, resulting in the loss of vision in the outer (temporal) halves of the visual field. In simpler terms, individuals with bitemporal hemianopia experience a "blind spot" on the outer sides of their visual field in both eyes, while the central and inner (nasal) fields of vision remain unaffected.
This unique visual impairment typically arises due to damage or compression of the optic chiasm, the point where the optic nerves from each eye cross and partially merge before transmitting visual information to the brain. The optic chiasm is responsible for relaying visual input from the retina to the brain's visual cortex, where it is processed and interpreted. When the optic chiasm is affected, it disrupts the normal flow of visual information, leading to the characteristic loss of vision in bitemporal hemianopia.
In this article, we will explore the causes, symptoms, and management options for bitemporal hemianopia, raising awareness about this uncommon yet impactful visual disorder and guiding those affected towards a clearer path forward.
The Science of Bitemporal Hemianopia: How It Affects Vision
To better understand bitemporal hemianopia, it's crucial to delve into the science behind how it affects vision. The human visual system is a complex network that relies on the seamless integration of the eyes, optic nerves, and brain to process and interpret the visual information we receive from our surroundings.
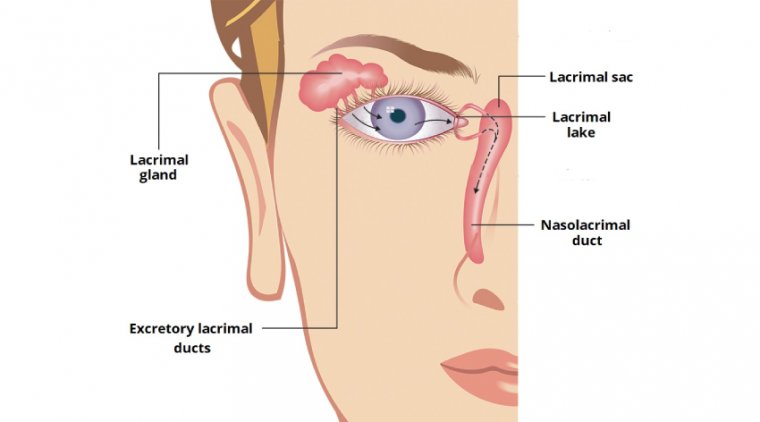
In a healthy visual system, light enters the eye and is focused on the retina, a light-sensitive tissue lining the back of the eye. The retina contains specialized photoreceptor cells called rods and cones that convert light into electrical signals. These signals are then transmitted through the optic nerve to the optic chiasm, where the nerve fibers from the nasal halves of each retina cross to the opposite side, while the fibers from the temporal halves continue on the same side. This arrangement ensures that the right visual field of both eyes is processed in the left hemisphere of the brain and the left visual field in the right hemisphere.
Bitemporal hemianopia occurs when there is damage or compression at the level of the optic chiasm, disrupting the transmission of visual information from the temporal halves of both retinas. Since the nasal fibers cross at the chiasm, they are more susceptible to injury or compression, leading to the characteristic vision loss in the outer (temporal) visual fields of both eyes.
.jpg)
An Overview of Bitemporal Hemianopia Credit: Science Direct
Causes of Bitemporal Hemianopia
Bitemporal hemianopia is typically caused by an underlying condition that affects the optic chiasm. A range of factors can lead to the damage or compression of this crucial structure, disrupting the normal transmission of visual information and resulting in the characteristic visual field loss. Some common causes of bitemporal hemianopia include:
1. Brain tumors: A brain tumor, particularly one located near or within the sella turcica (a depression in the sphenoid bone that houses the pituitary gland), can compress the optic chiasm. Pituitary adenomas are the most common type of tumor associated with bitemporal hemianopia, although other types of tumors such as craniopharyngiomas, meningiomas, and gliomas can also be responsible.
2. Head trauma: Severe head injuries can result in damage to the optic chiasm or surrounding structures, leading to bitemporal hemianopia. Such injuries may involve direct trauma, hemorrhage, or swelling that compresses the chiasm.
3. Inflammatory conditions: Certain inflammatory diseases, such as sarcoidosis or multiple sclerosis, can cause inflammation and damage to the optic chiasm, resulting in bitemporal hemianopia.
4. Vascular conditions: Stroke or other vascular problems that affect the blood supply to the optic chiasm can cause ischemic injury, leading to visual field defects like bitemporal hemianopia.
5. Congenital anomalies: Rarely, developmental anomalies or congenital malformations of the optic chiasm can lead to bitemporal hemianopia.
6. Infections: In some cases, infections that spread to the central nervous system, such as meningitis or encephalitis, can cause inflammation or damage to the optic chiasm, resulting in bitemporal hemianopia.
Signs and Symptoms of Bitemporal Hemianopia
Bitemporal hemianopia presents with a unique pattern of vision loss that can impact an individual's daily life and activities. The signs and symptoms of this visual field defect may vary depending on the severity and extent of the damage to the optic chiasm. Some common signs and symptoms of bitemporal hemianopia include:
● Vision loss: The most characteristic symptom of bitemporal hemianopia is the loss of vision in the outer (temporal) halves of the visual field in both eyes. This can result in difficulties with peripheral vision and may cause individuals to bump into objects or miss visual cues on their left and right sides.
● Blurred vision: Some individuals may experience blurred vision in the affected areas of their visual field.
● Difficulty with night vision: The loss of peripheral vision can make it challenging to navigate in low-light conditions, as the outer visual field is crucial for detecting objects and obstacles in dimly lit environments.
● Difficulty with depth perception: Bitemporal hemianopia can make it harder to judge distances and perceive depth accurately, potentially leading to difficulties with activities such as driving, playing sports, or navigating uneven terrain.
● Eye strain or discomfort: Individuals with bitemporal hemianopia may experience eye strain or discomfort as they try to compensate for their vision loss by constantly scanning their environment or squinting to focus on objects.
Visual Field Defects and Impairments
Visual field defects are characterized by a loss or impairment of vision in specific areas of the visual field. These defects can arise due to damage or dysfunction at various points along the visual pathway, from the retina to the optic nerve, optic chiasm, and the visual cortex in the brain. Bitemporal hemianopia is one such visual field defect; however, there are several other types of visual field defects that can occur due to different underlying causes. Some common visual field defects include:
1. Homonymous hemianopia: Homonymous hemianopia is a visual field defect that affects the same side of the visual field in both eyes (either the left or right side). This condition typically results from damage to the optic tract or the visual cortex in the brain, often due to a stroke, brain tumor, or head trauma.
2. Quadrantanopia: Quadrantanopia is a visual field defect that affects a quarter of the visual field in both eyes. It can be classified as superior (upper) or inferior (lower) and homonymous (affecting the same side in both eyes) or heteronymous (affecting opposite sides in each eye). Quadrantanopia usually results from damage to specific areas of the visual pathway or cortex, often due to a stroke or brain injury.
3. Central scotoma: A central scotoma is a visual field defect characterized by a blind spot or area of reduced vision in the central visual field. This condition often arises due to damage to the macula, the central region of the retina responsible for detailed central vision. Common causes of central scotoma include age-related macular degeneration, optic neuritis, and glaucoma.
4. Peripheral scotoma: A peripheral scotoma is a visual field defect that affects the peripheral or outer regions of the visual field. It can be caused by a variety of factors, including glaucoma, retinitis pigmentosa, or damage to the peripheral retina due to injury or disease.
5. Tunnel vision: Tunnel vision refers to a significant loss of peripheral vision, resulting in a narrowed visual field that resembles looking through a tunnel. This condition can be caused by various factors, including advanced glaucoma, retinitis pigmentosa, or damage to the peripheral visual pathways.
Impacts on Daily Life
Visual field defects, such as bitemporal hemianopia, can have significant consequences on an individual's daily life, affecting their ability to carry out routine tasks and participate in social activities. The impact of these vision impairments may vary depending on the severity and extent of the visual field loss, as well as the individual's lifestyle and personal circumstances. Some common ways in which visual field defects can impact daily life include:
Difficulty with mobility: The loss of peripheral vision can make it challenging to navigate unfamiliar environments, avoid obstacles, and maintain balance, increasing the risk of falls and accidents.
Impaired driving ability: Visual field defects can compromise driving safety by limiting the ability to detect vehicles, pedestrians, or obstacles on the side of the road. In some cases, individuals with significant visual field loss may not meet the legal requirements for driving and may need to relinquish their driving privileges.
Challenges in social settings: Limited peripheral vision can make it difficult to engage in group conversations, as individuals may struggle to see all participants or perceive non-verbal cues from those outside their visual field.
Difficulty with sports and recreational activities: Visual field defects can impact the ability to participate in sports and other recreational activities, particularly those that require good peripheral vision and depth perception, such as basketball, soccer, or skiing.
Struggles with reading and screen use: Depending on the extent and location of the visual field loss, individuals may experience difficulties with reading, watching TV, or using a computer or smartphone, as they may struggle to see the entire screen or page at once.
Increased anxiety and depression: The challenges and limitations imposed by visual field defects can lead to feelings of frustration, isolation, and depression, as individuals may feel limited in their independence and ability to participate in daily activities.
Diagnosis and Management of Bitemporal Hemianopia
Diagnosing and managing bitemporal hemianopia requires a comprehensive approach involving several steps, from identifying the visual field defect to addressing its underlying cause and providing appropriate support and rehabilitation services.
1. Diagnosis: Bitemporal hemianopia is typically diagnosed through a combination of a patient's medical history, a thorough eye examination, and visual field testing. A common test used to identify visual field defects is perimetry, which assesses the patient's peripheral vision by presenting light stimuli at various locations in their visual field. Imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may also be ordered to identify any structural abnormalities or lesions that could be causing the bitemporal hemianopia.
Identifying the underlying cause: Once bitemporal hemianopia is diagnosed, it is crucial to determine its underlying cause. As previously mentioned, bitemporal hemianopia is often caused by conditions that affect the optic chiasm, such as brain tumors, head trauma, or vascular issues. Identifying the cause is essential for determining the most appropriate treatment and management plan.
Treatment of the underlying cause: The treatment for bitemporal hemianopia will depend on the cause of the visual field defect. For example, if a brain tumor is responsible, treatment options may include surgery, radiation therapy, or chemotherapy. In cases of vascular issues, managing risk factors like high blood pressure or diabetes may help improve the condition. It is crucial to work closely with healthcare professionals to develop a tailored treatment plan based on the specific cause and individual needs.
Vision rehabilitation and support: Managing bitemporal hemianopia also involves providing support and rehabilitation services to help individuals adapt to their visual field loss and maintain their independence and quality of life. Occupational therapists and low vision rehabilitation specialists can offer guidance on adaptive techniques, visual aids, and home modifications that can make daily activities more manageable. Counseling and support groups may also be beneficial for individuals experiencing emotional challenges related to their vision loss.
Nonsurgical and Surgical Management Options
Looking Ahead: Advances in Bitemporal Hemianopia Management and Treatment
As researchers and clinicians continue to study and better understand bitemporal hemianopia, there is hope for future advancements in the management and treatment of this visual field defect. Some areas of potential progress include:
1. Improved diagnostic techniques: The development of more advanced imaging technologies and visual field testing methods could help healthcare professionals diagnose bitemporal hemianopia more accurately and quickly, allowing for earlier intervention and potentially better outcomes.
2. Gene therapy: As our understanding of the genetic factors contributing to bitemporal hemianopia and its underlying causes grows, there may be opportunities for gene therapy or other targeted treatments that address these genetic components, potentially offering new ways to prevent or treat this condition.
3. Neuroprotective agents: Researchers are investigating neuroprotective agents that may help protect the optic chiasm and other neural structures from damage caused by various factors, such as inflammation, ischemia, or trauma. These agents could potentially be used as a preventative measure or as part of the treatment plan for bitemporal hemianopia.
4. Brain-computer interfaces: Advances in brain-computer interfaces and neuroprosthetics may offer potential solutions for restoring vision in individuals with visual field defects like bitemporal hemianopia. While still in the early stages of research, these technologies hold promise for helping people regain some degree of visual function.
5. Personalized medicine: As the field of personalized medicine continues to evolve, there may be opportunities to develop more targeted and individualized treatment plans for bitemporal hemianopia based on factors such as genetics, lifestyle, and the specific cause of the visual field defect.
6. Enhanced rehabilitation and support services: Advances in low vision rehabilitation and assistive technologies can help improve the quality of life for individuals with bitemporal hemianopia. Continued research and innovation in these areas can lead to more effective tools and strategies for adapting to visual field loss and maintaining independence.
To Conclude...
Bitemporal hemianopia is a complex visual field defect that can significantly impact an individual's daily life and overall well-being. Throughout this article, we have explored the science behind bitemporal hemianopia, its causes, symptoms, diagnosis, management, and potential advancements in treatment. Early detection and intervention are crucial to minimize the impact of this condition on a person's quality of life.
By understanding the various aspects of bitemporal hemianopia, we can better support individuals affected by this condition and provide them with the necessary tools and resources to navigate their daily lives. As research and technology continue to advance, there is hope for improved diagnostic techniques, more effective treatment options, and enhanced support services that can help individuals with bitemporal hemianopia maintain their independence and enjoy a better quality of life.
In conclusion, by raising awareness and fostering a greater understanding of bitemporal hemianopia, we can work together to ensure that individuals affected by this condition receive the care and support they need to face the challenges ahead with resilience and hope.
(1).jpg)
.PNG)