Corneal Collagen Cross-Linking as a Game-Changer for Eye Health
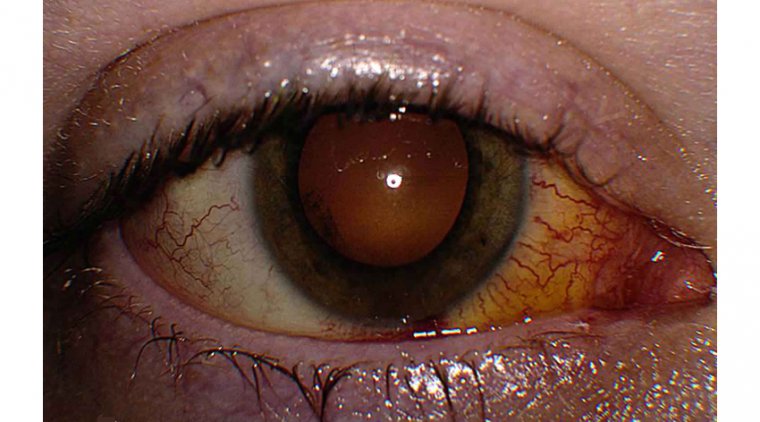
The world of ophthalmology is constantly evolving, with innovative treatments and procedures emerging to address a wide range of eye conditions. One such cutting-edge treatment, corneal collagen cross-linking (CXL), has gained significant attention for its role in managing keratoconus, a progressive eye disorder that affects the shape of the cornea. This article delves into the world of corneal collagen cross-linking, providing an in-depth look at this revolutionary procedure and its effectiveness in treating keratoconus.
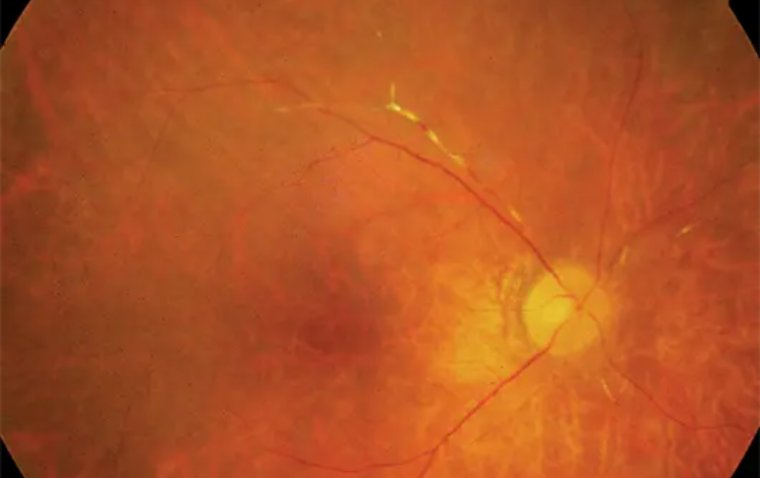
Corneal collagen cross-linking is a minimally invasive procedure that strengthens the corneal structure by promoting the formation of new collagen bonds within the cornea. This treatment is particularly beneficial for individuals suffering from keratoconus, a condition characterized by the thinning and bulging of the cornea into a cone-like shape. Left untreated, keratoconus can lead to significant vision impairment and even corneal transplant in severe cases. With the advent of corneal collagen cross-linking, patients now have a viable option to halt the progression of keratoconus and preserve their vision.
What Is Corneal Collagen Cross-Linking?
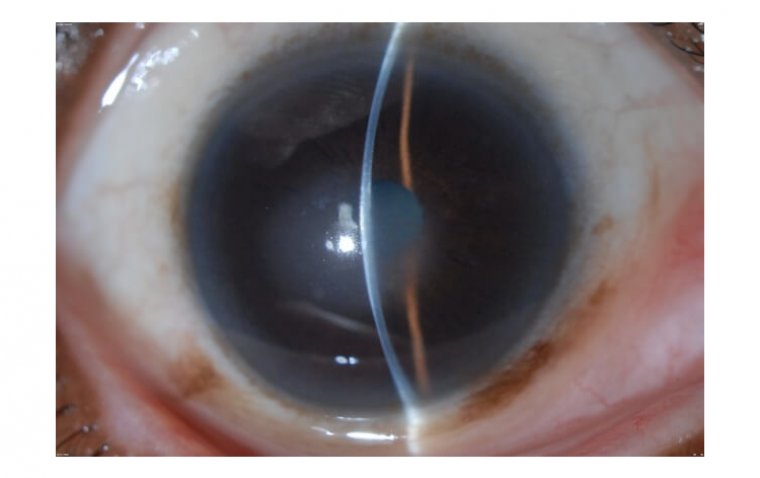
Corneal collagen cross-linking (CXL) is a minimally invasive, FDA-approved treatment designed to strengthen the cornea and halt the progression of keratoconus and other corneal ectatic disorders. The procedure works by increasing the collagen cross-links within the corneal stroma, the middle layer of the cornea composed primarily of collagen fibers. These cross-links act as supportive structures, providing stability and maintaining the cornea's shape and curvature.
During the CXL procedure, riboflavin (vitamin B2) eye drops are applied to the cornea, which is then exposed to ultraviolet-A (UVA) light. The combination of riboflavin and UVA light triggers a photochemical reaction that forms new covalent bonds between the collagen fibers. As a result, the cornea becomes stiffer and more resistant to deformation, effectively slowing or stopping the progression of keratoconus.
There are two primary techniques used for corneal collagen cross-linking: epithelium-off (also known as the Dresden protocol) and epithelium-on (also referred to as transepithelial or epi-on). The epithelium-off method involves removing the outer layer of the cornea (epithelium) before applying riboflavin eye drops, while the epithelium-on technique leaves the epithelium intact during the procedure. Each method has its advantages and potential risks, and the choice of technique is typically determined by the ophthalmologist based on the patient's specific needs and corneal condition.
How Does Corneal Collagen Cross-Linking Work?
Corneal collagen cross-linking (CXL) works by promoting the formation of new covalent bonds between collagen fibers within the corneal stroma, the middle layer of the cornea. This process strengthens the cornea's structure and increases its biomechanical stability, which can slow or stop the progression of keratoconus and other corneal ectatic disorders. Here's a step-by-step breakdown of how CXL works:
1. Pre-treatment: Before the CXL procedure, the ophthalmologist will conduct a thorough eye examination and assess the patient's corneal thickness. If the cornea is too thin, the procedure may not be suitable. In some cases, the ophthalmologist may recommend using a technique called hypotonic riboflavin to increase corneal thickness temporarily.
2. Riboflavin application: Depending on the chosen technique (epithelium-off or epithelium-on), the outer layer of the cornea (epithelium) may be removed to facilitate the absorption of riboflavin eye drops. The riboflavin solution is then applied to the cornea for a specific duration, typically around 30 minutes.
3. Ultraviolet-A (UVA) light exposure: After the cornea has been sufficiently saturated with riboflavin, the patient's eye is exposed to a controlled dose of UVA light for a predetermined period, usually between 10 to 30 minutes. The UVA light activates the riboflavin, which, in turn, generates reactive oxygen species (ROS). These ROS molecules initiate the formation of new covalent bonds between collagen fibers, increasing the cornea's rigidity and stability.
4. Post-treatment: Once the UVA exposure is complete, the eye is rinsed, and a soft contact lens or a bandage may be placed on the eye to protect it and promote healing. The patient is typically prescribed antibiotic and anti-inflammatory eye drops to prevent infection and reduce inflammation.
What Are the Benefits of Corneal Collagen Cross-Linking?
Corneal collagen cross-linking (CXL) offers several benefits for patients with keratoconus and other corneal ectatic disorders. These benefits include:
1. Halting disease progression: CXL is designed to slow or stop the progression of keratoconus and other corneal ectatic disorders by strengthening the cornea's structure. This can help prevent further vision deterioration and reduce the need for more invasive treatments, such as corneal transplants, in the future.
2. Potential improvement in vision: While the primary goal of CXL is to halt disease progression, some patients may experience an improvement in their vision following the procedure. This can occur due to a slight flattening of the cornea, which can reduce irregular astigmatism and enhance visual acuity.
3. Minimally invasive procedure: CXL is a minimally invasive outpatient procedure, which means it can be performed with minimal disruption to the patient's daily life. The recovery time is relatively short, especially for the epithelium-on (epi-on) technique, which does not involve removing the outer layer of the cornea.
4. Long-lasting results: Studies have shown that the effects of CXL can be long-lasting, with many patients experiencing stable corneal conditions for several years following the procedure. However, it is important to note that the results can vary depending on the individual and the severity of their condition.
5. Improved quality of life: By stabilizing the cornea and potentially improving vision, CXL can help patients maintain their independence and participate in activities they enjoy without the fear of their vision worsening due to keratoconus progression.
6. Customizable treatment: The two main techniques of CXL, epithelium-off (Dresden protocol) and epithelium-on (transepithelial or epi-on), allow ophthalmologists to customize the treatment based on the patient's specific needs and corneal condition.
How Is the Procedure Done?
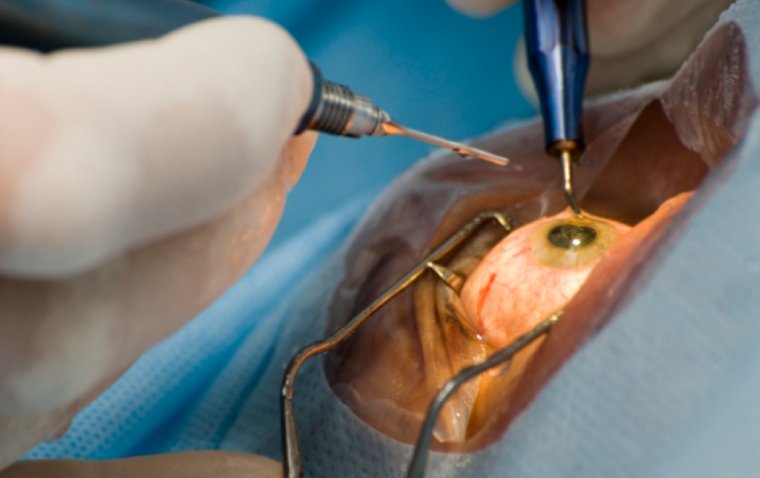
Corneal collagen cross-linking (CXL) is a minimally invasive outpatient procedure that can help slow or halt the progression of keratoconus and other corneal ectatic disorders. The following steps outline the general process of the CXL procedure:
Step 1: Pre-assessment Before the CXL procedure, the ophthalmologist will conduct a thorough eye examination, including measuring the corneal thickness and assessing the overall health of the eye. This helps determine if the patient is a suitable candidate for the procedure.
Step 2: Anesthesia The patient is administered topical anesthetic eye drops to numb the eye and minimize discomfort during the procedure.
Step 3: Epithelial removal (epithelium-off technique only) For the epithelium-off CXL technique, the outermost layer of the cornea (the epithelium) is gently removed to allow better absorption of the riboflavin solution. This step is not performed in the epithelium-on (epi-on) technique.
Step 4: Riboflavin application The patient's eye is treated with riboflavin (vitamin B2) eye drops for about 30 minutes. This allows the riboflavin to penetrate and saturate the corneal tissue.
Step 5: Ultraviolet-A (UVA) light exposure Once the cornea has absorbed sufficient riboflavin, the patient's eye is exposed to controlled UVA light for 10 to 30 minutes. The UVA light activates the riboflavin, which generates reactive oxygen species (ROS) and promotes the formation of new covalent bonds between collagen fibers, ultimately strengthening the cornea's structure.
Step 6: Post-treatment care After the UVA exposure, the eye is rinsed, and a soft contact lens or bandage is placed on the eye to protect it and promote healing. The patient is prescribed antibiotic and anti-inflammatory eye drops to prevent infection and reduce inflammation.
Step 7: Follow-up appointments The patient will attend follow-up appointments with their ophthalmologist to monitor the healing process and assess the effectiveness of the treatment. These appointments may be scheduled within the first few days, weeks, or months following the procedure, depending on the patient's individual needs.
.jpg)
What Happens During the Corneal Collagen Cross-Linking Procedure?
During the corneal collagen cross-linking (CXL) procedure, the ophthalmologist first conducts a pre-assessment to evaluate the patient's suitability for CXL. After applying topical anesthetic eye drops, the outermost layer of the cornea (the epithelium) may be removed, depending on the CXL technique used. The cornea is then treated with riboflavin eye drops for approximately 30 minutes, followed by controlled UVA light exposure for 10 to 30 minutes. This process strengthens the corneal structure and helps halt the progression of keratoconus or other ectatic disorders. Post-treatment care involves rinsing the eye, applying a soft contact lens or bandage, and prescribing antibiotic and anti-inflammatory eye drops. Finally, the patient will attend follow-up appointments to monitor the healing process and assess the effectiveness of the treatment.
How Long Does the Procedure Take?
The corneal collagen cross-linking (CXL) procedure typically takes about 1-2 hours from start to finish. The actual duration can vary depending on the specific technique used (epithelium-off or epithelium-on) and the patient's individual circumstances.
Here is a rough breakdown of the time spent on each step of the procedure:
● Pre-assessment: This can vary depending on the tests conducted and the patient's specific needs.
● Anesthesia: A few minutes for the topical anesthetic eye drops to take effect.
● Epithelial removal (if applicable): This step, if performed, takes approximately 5 to 10 minutes.
● Riboflavin application: About 30 minutes for the riboflavin eye drops to penetrate and saturate the corneal tissue.
● Ultraviolet-A (UVA) light exposure: This step generally takes 10 to 30 minutes, depending on the specific CXL protocol used.
● Post-treatment care: A few minutes to rinse the eye, apply a contact lens or bandage, and provide post-treatment instructions.
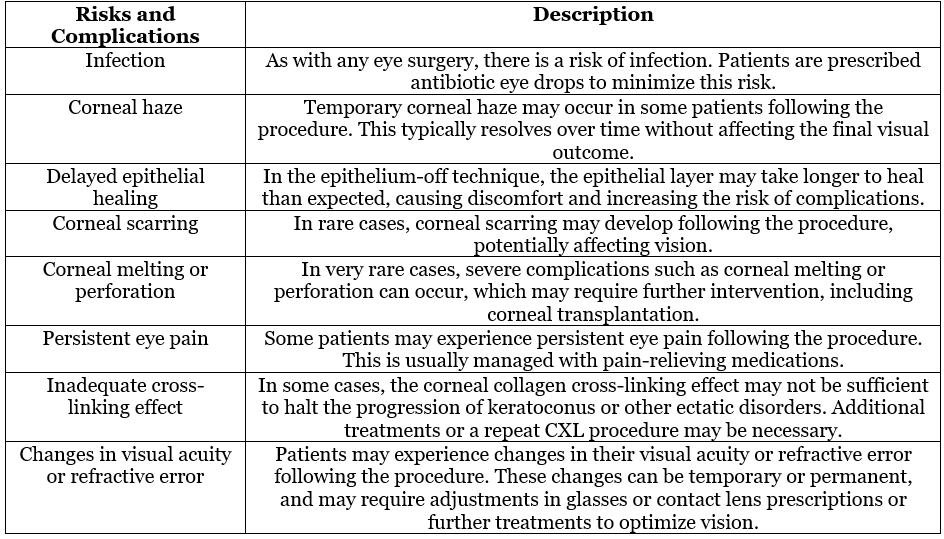
Risks and Complications
Who Is a Good Candidate for Corneal Collagen Cross-Linking?
A good candidate for corneal collagen cross-linking (CXL) typically exhibits the following characteristics:
1. Progressive keratoconus or other ectatic corneal disorders: CXL is primarily indicated for patients with progressive keratoconus, pellucid marginal degeneration, or post-refractive surgery ectasia. These conditions lead to the thinning and bulging of the cornea, which can cause vision impairment. CXL aims to strengthen the corneal tissue and halt the progression of these disorders.
2. Adequate corneal thickness: A minimum corneal thickness is required for the CXL procedure to be effective and safe. Generally, the cornea should be at least 400 micrometers thick after the removal of the epithelium (if applicable). This requirement may vary based on the specific CXL technique used.
3. Age: CXL is typically recommended for patients over the age of 14, as this is when the progression of keratoconus is most likely to occur. However, the procedure can be considered for younger patients if their keratoconus is rapidly progressing or severely impacting their vision.
4. Clear central cornea: Patients should have a relatively clear central cornea, as significant scarring or opacities in this area may limit the effectiveness of the CXL procedure and negatively affect visual outcomes.
5. No active eye infections or inflammation: Patients should not have any active eye infections or inflammation at the time of the procedure, as these conditions may increase the risk of complications.
6. No history of poor corneal wound healing: Patients with a history of poor corneal wound healing or other corneal disorders that may increase the risk of complications are generally not considered good candidates for CXL.
Alternative Treatments
While corneal collagen cross-linking (CXL) is an effective treatment for keratoconus and other ectatic corneal disorders, there are alternative treatments available, depending on the severity and progression of the condition. Some of these alternatives include:
● Glasses and contact lenses: In the early stages of keratoconus, prescription glasses or soft contact lenses may be sufficient to correct vision. As the condition progresses, specialized contact lenses, such as rigid gas permeable (RGP) lenses, hybrid lenses, or scleral lenses, may be required to achieve optimal vision correction.
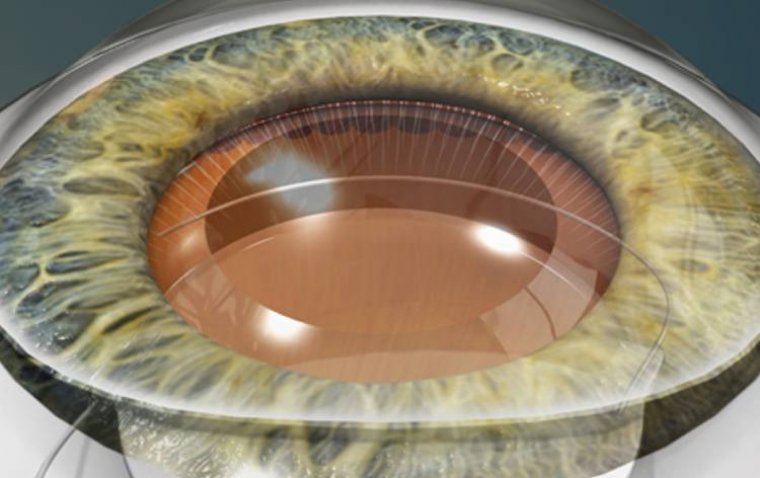
● Corneal inserts (Intacs): Intacs are semi-circular plastic segments that are surgically implanted into the cornea to help reshape and flatten it, improving vision. They are typically used for patients with moderate keratoconus who cannot tolerate contact lenses.
● Topography-guided photorefractive keratectomy (PRK): In some cases, topography-guided PRK, a type of laser eye surgery, may be used to reshape the cornea and improve vision in patients with keratoconus. This procedure is often combined with CXL to provide additional corneal strengthening and stability.
● Corneal transplantation: In advanced cases of keratoconus or other ectatic corneal disorders, when other treatments are no longer effective, a corneal transplantation may be necessary. This involves replacing the damaged cornea with healthy donor tissue. There are different types of corneal transplants, including deep anterior lamellar keratoplasty (DALK) and penetrating keratoplasty (PK).
Conclusion
In the blink of an eye, corneal collagen cross-linking (CXL) has emerged as a sight-saving treatment for those struggling with keratoconus and other ectatic corneal disorders. By shedding light—literally—on the affected cornea, CXL strengthens the tissue, halting the progression of these conditions and preserving vision. While CXL may not be the perfect fit for everyone, it has undoubtedly become a cornerstone in the management of these disorders.
But don't get too cornea-whelmed! Alternative treatments, such as glasses, contact lenses, Intacs, and even corneal transplantation, can help patients see the world in a whole new light. As with any medical condition, early detection and intervention are key to maintaining optimal vision and eye health. So, don't turn a blind eye to the importance of regular eye examinations and consultations with a corneal specialist—seeing is believing, after all!
(1).jpg)