The Role Of Endoscopy In Ophthalmology
Current technology for ophthalmic endoscopy delivers undoubted advantages in certain surgical situations.
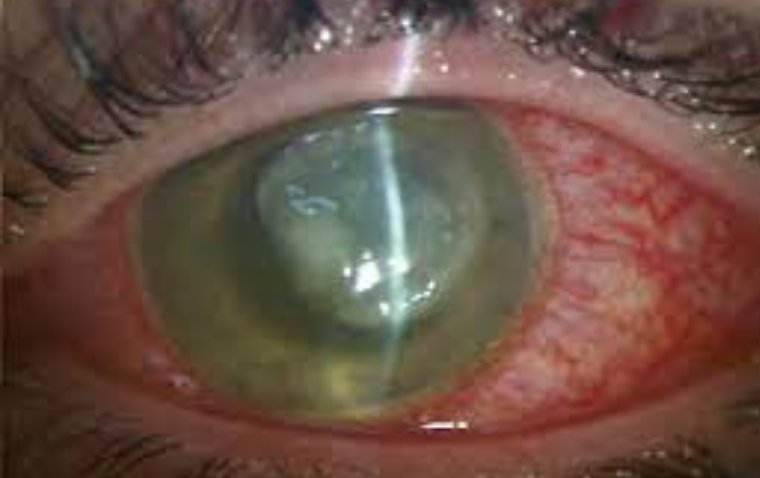
It provides excellent visualization in eyes with compromised view through the cornea, anterior segment, or lens.
It facilitates excellent peripheral PRP in the patients with peripheral ischemic retinopathies. It allows ECP in patients with glaucoma, either at the time of cataract surgery or as a standalone procedure.
Generations of ophthalmologists have recognized the intrinsic value of endoscopy.
Since 1934, when Thorpe combined a Galilean telescope, light source and eyepiece and then made an 8-mm scleral incision to extract nonmagnetic intraocular foreign bodies, inventor-surgeons have tinkered with it, allowing for intraocular and orbital surgery; remote visualization of real-time images; and, after Martin Uram, MD, added a laser in 1992, endoscopic cyclophotocoagulation (ECP).
Improvements to the unit’s size, maneuverability and clarity followed. And then, a few years later, ECP and phacoemulsification were combined.
But the ophthalmic industry is chock-a-block with rolling stones, and new techniques arose to confront the challenges of managing glaucoma concurrent with cataract surgery. So once again, ECP slid under the radar.
The slide has apparently stopped.
“Everything is cyclical,” says Robert Noecker, MD, MBA, of Ophthalmic Consultants of Connecticut. “Surgeons get distracted by new things, then return to what consistently works.”
And, he adds, “The technology has improved from the original version.”
Renaissance Tech
Over the past few years, endoscopy has had a renaissance of sorts, with uses that include other glaucoma procedures, retinal surgeries, anterior segment procedures and ocular traumas.
“It gives you a view into the eye that you cannot get any other way,” says Brian Francis, MD, director of glaucoma services and the Rupert and Gertrude Steiger chair in Vision Research at the UCLA Doheny Eye Institute.
“It allows you to not only treat areas that you didn’t have access to before but allows you to diagnostically make decisions during surgery based on what you can see through the endoscope that you cannot see through the operating microscope.”
Because you can see the anatomy, says David A. Goldman, MD, cases that would normally be obscured because of a cloudy or scarred cornea now can be viewed, and areas like the sulcus that usually aren’t easily visible are now visible.
Although most people associate ECP with the whole unit, the endoscope now has reusable parts, assisting not only diagnostic but also therapy making decisions, says Dr. Goldman, an ophthalmologist in Palm Beach Gardens, Fla.
“Even if you’re not using the laser, the endoscope provides a lot of advantages,” like performing a host of different surgeries.
Endoscopy Overview
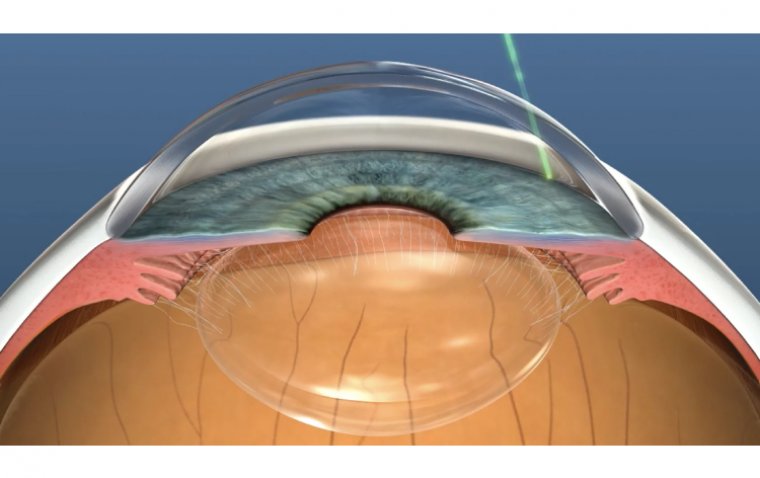
The beauty of using endoscopy for glaucoma and ECP-related surgeries, says Dr. Francis, is that it decreases aqueous production; other procedures work on outflow — but that doesn’t preclude the two types of procedures from being used together (more on this in a minute).
ECP also shrinks the ciliary processes, and that action opens the angle in cases of severe plateau iris.
Dr. Francis, first introduced to the technology during his fellowship 20 years ago, says standard ECP is an anterior approach through a clear corneal incision; it can be a standalone procedure in a pseudophakic or aphakic patient with or without other glaucoma surgeries, or combined with phacoemulsification cataract surgery.
The combined procedure — best for patients with mild to moderate glaucoma who have cataracts and the desire to reduce IOP or glaucoma medications — is more effective at lowering IOP and reduces the need for glaucoma medications over a longer period of time than just a cataract procedure.
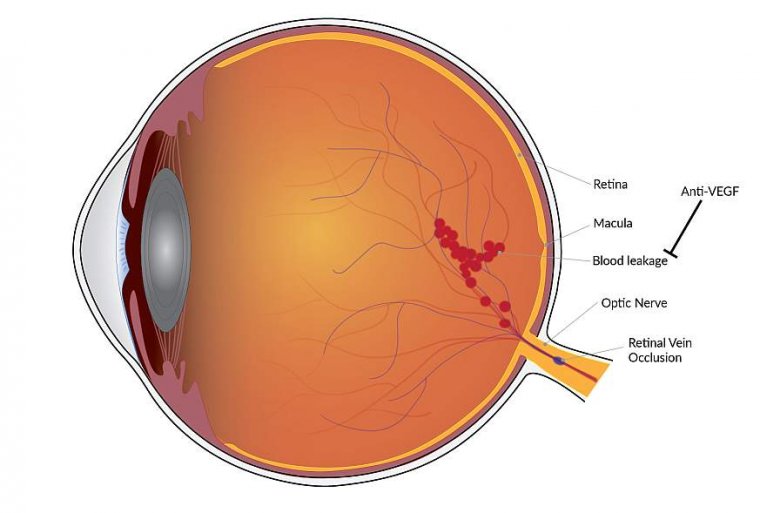
For patients whose eyes failed a prior glaucoma surgery or whose IOP did not sufficiently reduce, ECP can be added to minimally invasive glaucoma surgery (MIGS), such as trabeculotomy by internal approach (Trabectome, Neomedix) or with placement of a trabecular bypass stent (iStent, Glaukos) or suprachoroidal stent (CyPass, Alcon) to enhance pressure lowering in surgery, Dr. Francis says.
The point, he says, is to combine different MIGS procedures that use different pathways.
“Let’s say you have an outflow procedure such as an iStent. You can combine that with ECP, which is an aqueous inflow procedure, to try to lower IOP more than can be accomplished with the outflow procedure alone.”
“Usually, you put a gonioscopy lens on the eye to visualize the angle,” says Dr. Noecker, “but with the endoscope we can directly visualize where we want to put the device and also evaluate it after it’s in.” Dr. Noecker has used endoscopy since 1999 and co-teaches an endoscopy course with Dr. Francis at the AAO annual meetings.
The Hardcore Cases
For patients with more severe glaucoma who have failed trabeculectomy or tube shunt, ECP can augment regular glaucoma filtration surgery.
In those whose advanced glaucoma is recalcitrant to multiple glaucoma filtration surgery and other procedures, Dr. Francis recommends using ECP-plus, which uses a pars plana approach and allows laser ablation of the pars plana.
“By entering the pars plana, you’re able to view the ciliary processes … completely, and therefore you’re able to treat the ciliary processes in a more aggressive and complete manner, achieving better pressure-lowering,” he says.
“You’re also treating about one or two rows of the pars plana, so that gives you even more profound pressure-lowering.”
In a study published earlier this year, patients treated with ECP-plus had their mean IOP lowered by at least 61%, which was sustained for a follow-up period of more than one year.
Also, patients needed fewer glaucoma medications.
Other Applications
ECP can be useful in other types of glaucoma, Dr. Francis adds. For example, patients with plateau iris syndrome are refractory to iridotomy and iridoplasty and in some cases, lens removal. These patients can benefit from endoscopic cycloplasty (ECPL) and lens extraction.
“We take out the lens but use the laser to treat and shrink the ciliary processes in the eye,” Dr. Francis says. “The pathogenesis of plateau iris is very large; anteriorly rotated ciliary processes push the iris forward and close the angle.
By directly viewing and shrinking those processes, you’re pulling them away posteriorly from the iris, thereby opening up the angle. We have found that to be more effective in these severe patients than just taking out the lens.”
It’s also helpful for angle trauma like cyclodialysis clefts, iridodialysis, even angle surgery such as excimer laser trabeculostomy (ELT, TUI-Laser – currently in FDA trials), which you can do via the endoscopic view as well as sulcus procedures, Dr. Francis adds.
Few Left Out in the Cold
The vast majority, 90%, of patients are appropriate candidates for ECP, say Drs. Noecker and Goldman.
However, Dr. Goldman does not recommend it for patients with uveitic glaucoma because the procedure itself is pro-inflammatory. Adds Dr. Noecker: “You have to be able to visualize behind the iris, so if someone has a lot of adhesions it can be difficult.”
Again, emphasizes Dr. Goldman, ECP’s advantage is it allows direct visualization of your treatment. “Right now some other devices are transscleral cyclodestructive procedures, and you’re basically going until you hear an audible pop sound.”
“ That’s a more aggressive treatment even though it’s technically approved for mild to moderate disease. When you’re talking about blindly treating versus visualizing your treatment, there’s a big advantage to being able to do it via endoscopy.”
Not For Glaucoma Specialists Only
Beyond glaucoma, ophthalmologists are finding additional uses for endoscopy, such as in posterior segment procedures. Some eye surgeons are treating retinal detachments or proliferative vitreoretinopathy.
When looking through the endoscope, the light source shines straight into the vitreous and reflects back, which makes it easily identifiable, appearing like a fog or mist. In a microscope, however, it looks clear, Dr. Francis says.
Endoscopy can also be used for ocular traumas. Dr. Goldman recently saw a patient with a ruptured globe. Even after he repaired the cornea — it was in multiple pieces — it was very cloudy.
“We knew there was an intraoperative foreign body and we had some idea where it was based on preoperative CT scans but didn’t know [the exact location].” Using the endoscope, he located the foreign body and extracted it.
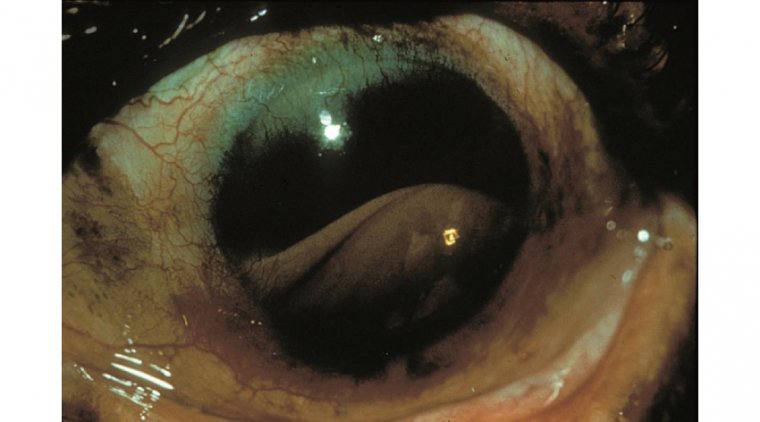
Dr. Francis has used the endoscope when managing patients referred for lingering problems. In one case, a patient presented with uveitis-glaucoma-hyphema syndrome after cataract surgery and a follow-up procedure to cut off a haptic in the sulcus.
Using the endoscope, he saw that the capsule had fibrosed underneath the cut-off haptic, and the optic next to it tilted the IOL at an angle where the sharp edge pointed up toward the iris. He reopened the capsular bag in that area, tucked in the optic and straightened out the lens implant.
What You’ll Need to Know
Yes, there is a learning curve. First, remember it’s heads up, not down. “Instead of looking through the microscope, with endoscopy you actually sit up and look at a TV screen to monitor what you’re doing,” Dr. Goldman says.
“That’s something … other specialists have been doing for decades, but it’s relatively new in ophthalmology.”
Because the view is more two-dimensional, adds Dr. Francis, concentrate on anatomy to get a feel for depth perception and the 3D clues.
Also, he adds, a surgeon will know how close she is to something by its size on the screen — the larger, the closer.
Dr. Goldman advises first-time ECP users to insert the scope at the end of cataract surgery to get a feel for the ECP probe. “What you’ll find is that if the sulcus is well-inflated with viscoelastic, the chamber should really stay stable and you should get really good visualization of the anatomy.”
Don’t get too aggressive with ECP, he adds; make sure to direct therapy just at the ciliary processes and stop when you see the whitening. Finally, make sure a good technician assists you, one who can provide optimal view and proper orientation.
No End in Sight
Dr. Goldman thinks more companies will develop endoscopes. His logic: More technologies are requiring smaller incisions, more procedures are being developed on the angle of the eye, so the endoscope could be the likely candidate “ to confirm good surgical technique.”
Adds Dr. Noecker: It’s been around for two decades so, “you might say, …‘It’s old and boring.’ But it keeps reinventing itself as the technology gets better and better.”
(1).jpg)