Intracapsular Cataract Extraction (ICCE): Indications, Complications, and Management
Cataract surgery is one of the most common and essential procedures for restoring vision. Among the various techniques, Intracapsular Cataract Extraction (ICCE) stands out for its unique approach of removing the entire lens and its capsule. Despite being largely replaced by more modern methods, ICCE remains a vital option in specific cases, particularly for patients with dense cataracts or insufficient zonules.
What is Intracapsular Cataract Extraction?
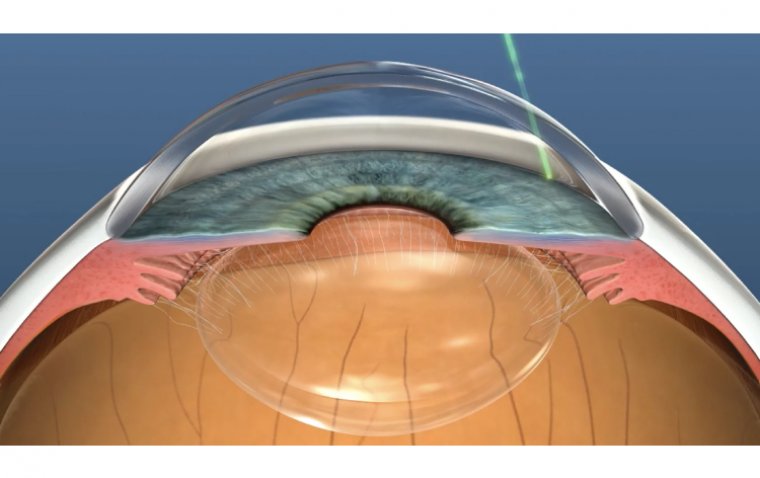
Intracapsular Cataract Extraction (ICCE) is a surgical technique where the entire lens and the surrounding capsule are removed from the eye. This method was more prevalent before the advent of modern techniques like phacoemulsification but still holds significance in certain scenarios. Historically, ICCE was the go-to procedure, providing a clear path for light to enter the eye, thereby improving visual acuity.
Surgical Procedure for Intracapsular Cataract Extraction
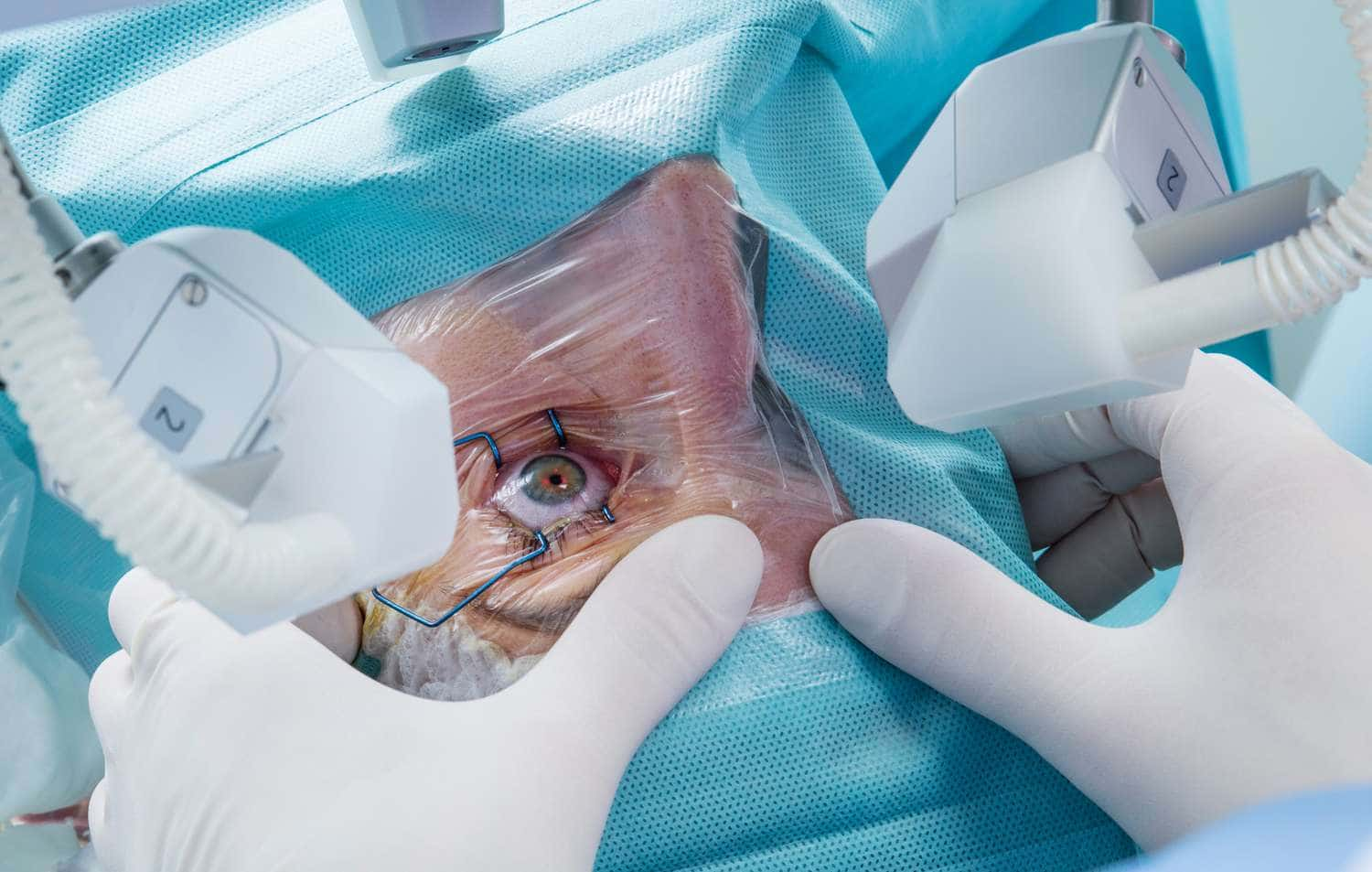
Intracapsular cataract extraction (ICCE) is a meticulous surgical procedure where the entire lens and its surrounding capsule are removed. This procedure, though less common today, is vital for certain eye conditions. Here's a detailed look at the steps involved in ICCE:
1. Preoperative Preparation
Before the surgery, the patient undergoes a thorough eye examination and medical evaluation. Specific instructions are provided regarding medications, fasting, and hygiene. Patients are typically advised to avoid eating or drinking for a few hours before the procedure to reduce the risk of complications.
2. Anesthesia
The procedure begins with the administration of anesthesia to ensure the patient experiences no pain. This can be local anesthesia, numbing only the eye, or general anesthesia, making the patient unconscious. The choice depends on the patient's condition and the surgeon's recommendation.
3. Eye Preparation
The eye is thoroughly cleaned and sterilized to prevent infection. An eyelid speculum is used to keep the eye open and steady during the surgery. The surrounding area is draped to maintain a sterile field.
4. Incision
A small incision is made in the cornea, the clear front part of the eye, to access the lens. The incision is carefully planned to allow for the removal of the lens and to minimize healing time. Sometimes, a larger incision is needed for this procedure compared to other cataract surgeries.
5. Lens and Capsule Removal
Using specialized instruments, the surgeon carefully separates the lens from its attachments and removes it along with the capsule. This is the critical step of ICCE, requiring precision to avoid damage to surrounding tissues. The entire lens-capsule complex is extracted as one piece.
6. Insertion of Intraocular Lens (IOL)
After removing the natural lens, an artificial intraocular lens (IOL) is implanted to restore vision. The type and positioning of the IOL are predetermined based on the patient's eye measurements. The IOL can be placed in the anterior chamber or sutured in place if needed.
7. Closing the Incision
The incision is closed using fine sutures or by applying a self-sealing technique, depending on the type and size of the incision. Proper closure is essential to prevent infection and ensure quick healing. The eye is then covered with a protective shield.
Postoperative Care and Follow-up
Postoperative care is crucial for a successful recovery. Regular follow-up appointments are scheduled to monitor the healing process and ensure the IOL is functioning correctly. The first follow-up is typically within 24 hours of the surgery, followed by additional visits over the next few weeks. Adjustments to medications or activities may be made based on recovery progress.
Comparison with Other Cataract Extraction Methods
Comparing ICCE with other techniques like extracapsular cataract extraction (ECCE) and phacoemulsification reveals significant differences. While ECCE involves removing the lens and leaving the capsule intact, phacoemulsification uses ultrasound to break the lens into smaller pieces. ICCE, however, involves a larger incision and is more invasive but eliminates the risk of posterior capsule opacification (PCO).
What Are the Benefits of Intracapsular Cataract Extraction?
● Improved Vision Clarity
One of the most significant benefits of ICCE is the potential for dramatically improved vision. By removing the entire cloudy lens, patients can experience a substantial increase in visual clarity, especially if they were previously experiencing severe cataract-related vision impairment.
● Suitability for Complex Cases
ICCE is particularly beneficial in complex cases where other cataract surgery methods might not be effective. For example, in instances of lens dislocation, severe trauma, or hyper-mature cataracts, ICCE allows the surgeon to manage the situation more comprehensively by removing the entire lens and capsule.
● Effective for Weak Zonules
Patients with conditions like Marfan syndrome, pseudoexfoliation syndrome, or other issues leading to weak zonules benefit significantly from ICCE. These conditions can make the lens unstable, and removing it entirely prevents further complications and ensures the stability of the intraocular lens implant.
● Lower Risk of Capsule-Related Complications
Since ICCE involves the removal of the entire lens capsule, it eliminates the risk of posterior capsule opacification (PCO). PCO is a common complication in other cataract surgeries where the capsule is left intact and can cause secondary vision impairment, often requiring additional laser treatment.
Risks and Complications of Intracapsular Cataract Extraction
While ICCE is generally safe, it carries risks like any surgical procedure. Some of these are:
Post-surgical infections can occur if bacteria enter the eye during or after the procedure. Proper sterilization and post-operative care, including the use of antibiotic eye drops, can minimize this risk.
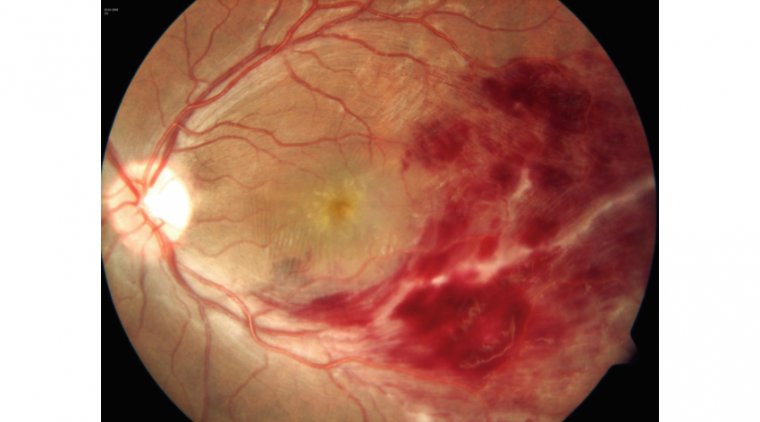
● Retinal Detachment
This serious complication involves the separation of the retina from the underlying tissue, potentially leading to vision loss. Immediate medical attention is required if symptoms like sudden floaters or flashes of light appear.
● Bleeding
Intraoperative or postoperative bleeding can occur, particularly if the patient has underlying health conditions or is on blood-thinning medications. Surgeons take precautions to minimize this risk.
● Prolonged Inflammation
Some patients may experience extended periods of inflammation post-surgery, requiring ongoing medication and monitoring to ensure it does not lead to further complications.
● Dislocation of Intraocular Lens (IOL)
Post-surgery, the artificial lens implanted during ICCE can become dislocated, necessitating additional surgical intervention to reposition or replace the IOL.

Intracapsular Cataract Extraction Recovery
Recovery from ICCE varies among patients but generally spans several weeks. Patients may experience mild discomfort and increased sensitivity to light. Following the surgeon's advice and avoiding strenuous activities can facilitate a smooth recovery and long-term visual improvement.
Conclusion
In conclusion, cataract surgery remains a fundamental procedure for restoring vision, with Intracapsular Cataract Extraction (ICCE) offering a unique approach by removing the entire lens and its capsule. Despite its decline in popularity due to advancements in surgical techniques, ICCE remains indispensable for specific cases, particularly those involving dense cataracts or compromised zonules.
Through meticulous preoperative preparation, precise surgical steps, and vigilant postoperative care, ICCE continues to provide substantial benefits, including improved vision clarity, suitability for complex cases, and a lower risk of capsule-related complications like posterior capsule opacification. However, as with any surgical procedure, ICCE carries certain risks and potential complications, underscoring the importance of informed patient consent, thorough preoperative evaluation, and attentive postoperative management to ensure optimal outcomes and long-term visual health.
Reference:
https://eyesurgeryguide.org/intracapsular-cataract-extraction/
(1).jpg)