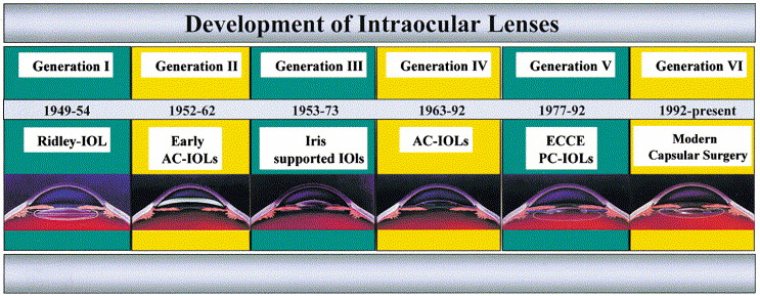
The Evolution of IOLs
Cataract is the most prevalent ophthalmic disease. Treatment of cataracts has been practiced for centuries using various surgical and nonsurgical procedures.
However, avoidance of complications and attainment of high-quality postoperative visual rehabilitation were difficult in the years before the introduction of modern IOLs. Because significant dioptric power resides in the crystalline lens, its removal results in marked visual disability.
In order to fully understand the technological evolution of cataract surgery over the past 50 years, we need to compare current surgical procedures and visual recovery times with those reported half a century ago.
A look at the history of cataract surgery clearly shows that its evolution is an outcome of the vision of a few inspired pioneers who had great passion for their profession. When phacoemulsification was first developed, it faced strong opposition and hence took time in being accepted by the majority of eye surgeons.
It was only with the introduction of intraocular lenses (IOLs), and to a greater degree with the advent of foldable IOLs, that the technique was accepted and used on a much larger scale. In the same way, the evolution of the IOL itself was influenced by ongoing technological progress with phacoemulsification devices and phacoemulsification techniques.
This progress led to the development of lenses that could be inserted through increasingly smaller incisions. Today we are able to perform cataract surgery in a few minutes, with visual rehabilitation, and we owe it exclusively to a small number of surgeons who firmly believed in these technological innovations.
Even though cataract surgery has been practiced for over 2000 years, modern cataract surgery started just some 50 years ago with the first IOL implantation by Sir Harold Ridley. The development of intraocular lenses was accompanied by great successes and disasters.
With the fast development of cataract surgical techniques over the past 20 years, a successful marriage between IOL-developments and surgery was established. Indication profiles for cataract surgery and IOL implantation extended to more and more patient groups.
At this time classical cataract surgery is further developing into refractive intraocular lens surgery to correct higher ametropia in clear lens or phakic eyes. This development was only possible because of the improvements of surgical techniques and implants in classical cataract surgery.
Intraocular lenses (IOLs) have come a long way from the first rigid polymethyl methacrylate, or PMMA, lenses implanted in the 1950s. Cataract surgery is now precise and predictable enough to allow surgeons to optimize refractive outcomes by offering a range of IOL technologies to satisfy patient needs.
Monofocal IOLs
Monofocal IOLs provide spherical correction for a single distance. These lenses do not address astigmatism or presbyopia – in other words, patients will require glasses for optimal vision after surgery.
Patients can choose distance, intermediate, or near with these lenses but cannot have multiple distance in focus at once (unless they choose monovision). Monofocal IOLs provide excellent image clarity and contrast with minimal aberrations, such as glare and halos.
These lenses are ideal for patients with ocular comorbidities, such as VF and contrast loss due to age-related macular degeneration (AMD) or glaucoma. Many lenses are variations of the common monofocal IOL platforms offered by the major IOL manufacturers.
Most current monofocal IOLs implanted, such as the Johnson & Johnson Vision (J&J) Tecnis (ZCB00), Alcon Acrysof (SA60WF), Vsy Biotech GmBH Enova™, and Bausch + Lomb enVista (MX60E), are one-piece lenses made of hydrophobic acrylic.
These lenses are foldable and are designed for placement in the capsular bag. J&J’s recently approved monofocal, Eyhance (ICB00), with a modified anterior surface sphericity to increase depth of focus and provide some range of vision, is an added benefit to current monofocal options.
Many monofocal three-piece IOLs are available, including the J&J Tecnis (ZA9003), Zeiss CT-Lucia, and the Alcon MA60AC. These lenses consist of a central optic with separate haptics attached to opposite sides.
Advantages of three-piece lenses include the versatility to safely place them in the capsular bag, sulcus, or sclera via fixation. Monofocal IOLs are covered by health insurance in the United States, but all other lenses discussed are typically an extra cost to the patient.
Toric IOLs
Monofocal toric IOLs are very similar to standard monofocal IOLs but also correct corneal astigmatism. These lenses must be positioned precisely during surgery based on preoperative measurements.
They are available in a range of sphere and cylinder powers to address most patients’ needs. All current monofocal, multifocal, and extended depth of focus (EDOF) platforms also are available in toric version for use in astigmatism treatment.
Multifocal & Trifocal IOLs
Multifocal IOLs, as the name suggests, create multiple focal points at different distances to treat presbyopia. These lenses have a pattern of rings formed in the central optic.
The rings focus light to provide clear distance, near, and/or intermediate vision, depending on the lens. The most common multifocal IOLs are the J&J Tecnis and the Alcon ReStor.
These are effectively bifocal lenses, providing good distance and near vision with limited intermediate vision. They are generally available in different add powers as well as sphere and cylinder powers.
The newest multifocal IOL available in the United States is the Alcon PanOptix. This trifocal lens provides good distance, intermediate, and near vision. Other IOLs in this category are in the pipeline for FDA approval with enhanced options to optimize range and minimize halos and glare.
Multifocal IOLs have increased aberrations (halos and glare) due to the rings of the optic and are not advisable for patients who have retinal disease, glaucoma, or irregular corneas.
EDOF IOLs
EDOF IOLs treat presbyopia by extending the range of focus rather than splitting light into discrete focal points. The advantages of EDOF lenses are reduced aberrations compared to multifocal/trifocal IOLS and improved intermediate vision compared to multifocal IOLs.
Near vision with EDOF IOLs is typically not as high quality as with multifocal or trifocal IOLs. These lenses should also be considered only for patients with otherwise relatively healthy eyes. EDOF IOLs available in the United States are the J&J Tecnis Symfony and the recently approved Alcon Vivity.
Vivity is similar to a monofocal IOL with a slight central change in curvature, providing good intermediate and distance vision with low aberrations similar to a monofocal IOL.
Light Adjustable IOL
The Light Adjustable Lens (RxSight) is different from prior IOLs, as the power of the lens can be changed after implantation.
The lens optic contains monomers that can be activated by a UV light treatment to alter the shape and power of the lens. This lens is implanted similarly to the other lenses discussed.
In the postoperative period, the refraction is obtained and treatments are applied to the lens in-office, eventually locking in the final power around one month after surgery. This lens is ideal for patients whose preoperative calculations are challenging, such as those who have corneal irregularities or have had previous laser vision correction.
Light adjustable lenses do not address presbyopia and have high image quality with minimal aberrations comparable to monofocal IOLs.
Accommodating IOLs
Accommodating IOLs are designed to address presbyopia by changing position, shape, or configuration when the eye accommodates.
This recreates the natural change in lens power with accommodation, reducing or eliminating presbyopia; patients with these lenses can see well at distance, intermediate, and near. Unlike multifocal and EDOF lenses, which have aberrations due to the rings etched in the optics, accommodating IOLs have minimal aberrations as their optics are smooth.
These lenses can therefore be used in patients with ocular conditions such as glaucoma or AMD. The only currently available accommodating IOL in the U.S. is the Bausch + Lomb Crystalens, which features flexible haptics that allow some movement of the optic during accommodation to effectively change power.
This IOL depends on capsular flexibility to accomplish range of vision, and the degree of IOL flexibility varies from case to case. Other accommodating IOLs that change shape include the Alcon FluidVision, the Atia Vision, and the Juvene IOLs, which are in the pipeline for approval.
Most of these IOLs can also treat astigmatism with a toric version, and the modular lenses can also be designed for drug delivery.
Finding The Right Lens
With the advances in technology and health care, patients are better informed and have higher expectations of cataract surgery than ever before.
Patients should be introduced to all IOL options so that they, along with their surgeon, can select the best lenses to fit their individual needs and lifestyles.
(1).jpg)