Myasthenia Gravis Ptosis: A Closer Look at the Eye Symptom
What Is Myasthenia Gravis?
Myasthenia gravis (MG) is an autoimmune neuromuscular disorder characterized by fluctuating muscle weakness and fatigue. In individuals with MG, the immune system produces antibodies that target acetylcholine receptors, vital for nerve-to-muscle communication. This disrupts the normal functioning of these receptors, making it difficult for the muscles to contract effectively and leading to muscle weakness.
Role of Acetylcholine Receptors and Muscle Weakness
Acetylcholine receptors are essential for transmitting signals between nerve endings and muscle fibers. When these receptors are blocked or destroyed due to the autoimmune response in MG, the muscle's ability to contract weakens. This can lead to a variety of symptoms but often manifests as ptosis (drooping of the eyelids), difficulty in speaking, swallowing, and even challenges with breathing and general mobility. The degree of muscle weakness can vary from person to person and may even fluctuate throughout the day.
Exploring Ptosis in Myasthenia Gravis
Link Between MG and Ptosis
In Myasthenia Gravis, the levator palpebrae superioris, the muscle responsible for lifting the upper eyelid, is frequently affected. The muscle's weakness leads to ptosis, or the drooping of the eyelid, making it difficult for patients to keep their eyes fully open. Because the levator muscle is one of the muscles often first impacted by the disease, ptosis can serve as an early symptom and a telltale sign that something may be amiss neuromuscularly.
Ptosis as a Common and Early Symptom
Ptosis is often one of the first symptoms to appear in MG and can be easily identified, even by the layperson, as a drooping eyelid. It may initially occur only after physical exertion or late in the day when muscles are fatigued but can become more constant as the disease progresses. Given its early onset in the course of MG, the presence of ptosis can be instrumental in prompting individuals to seek medical advice, leading to earlier diagnosis and treatment.
What Causes Myasthenia Gravis Ptosis?
Autoimmune Dysfunction
The primary cause of ptosis in Myasthenia Gravis is rooted in autoimmune dysfunction. In MG, the body's immune system mistakenly targets and attacks acetylcholine receptors at the neuromuscular junction. This leads to a decrease in the number of functional receptors, which are essential for muscle contraction.
Role of Acetylcholine Receptors
Acetylcholine is a neurotransmitter that bridges the gap between nerve cells and muscle cells, enabling muscle contraction. When acetylcholine receptors are compromised, the muscle cells receive fewer signals, resulting in muscle weakness. In the case of ptosis, the levator palpebrae superioris muscle is directly affected, making it difficult for the patient to lift the upper eyelid effectively.
Progressive Muscle Fatigue
One characteristic feature of Myasthenia Gravis is the fluctuating and often progressive nature of muscle weakness. Initially, ptosis may only be evident after prolonged periods of eye use or towards the end of the day. However, as the condition worsens, ptosis can become more constant and may affect one or both eyes.
Symptoms of Myasthenia Gravis Ptosis
Onset and Progression
The onset of ptosis in Myasthenia Gravis patients is often gradual, with muscle weakness fluctuating throughout the day. In some cases, the ptosis may be worse in the morning, while for others, it may intensify with fatigue as the day progresses. Over time, as the disease progresses, the ptosis may become more constant and potentially affect both eyes.
Accompanying Symptoms
While ptosis is a prominent symptom in MG, it is often accompanied by other signs of muscle weakness. These can include:
● Double Vision (Diplopia): Patients may experience temporary or chronic episodes of double vision, which may worsen with fatigue.
● Difficulty Swallowing (Dysphagia): Muscle weakness may extend to the throat, leading to difficulties in swallowing food or liquids.
● Muscle Fatigue: Generalized muscle weakness is common in MG, affecting various parts of the body including the arms, legs, and respiratory muscles.

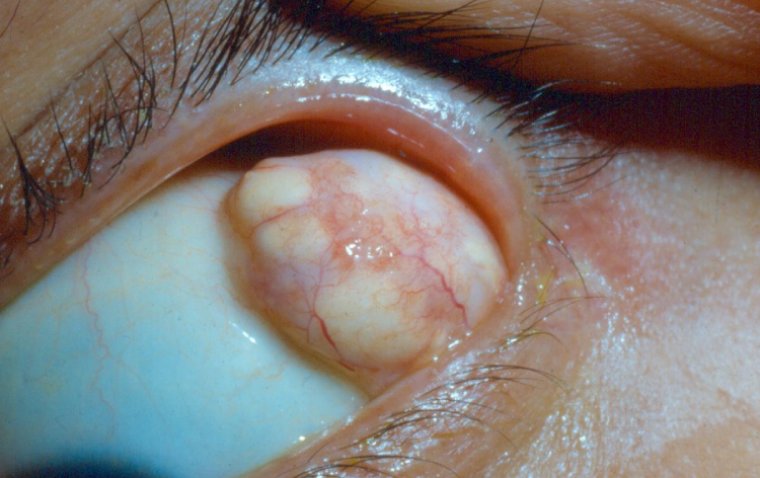
Credit: Moran CORE
How to Diagnose Myasthenia Gravis Ptosis
Diagnostic Methods
1. Tensilon (Edrophonium) Test: One of the most specific tests for Myasthenia Gravis, the Tensilon test involves administering edrophonium chloride to temporarily relieve muscle weakness. An immediate and significant improvement in muscle strength, including lifting of the ptotic eyelid, is a positive indication of MG.
2. Repetitive Nerve Stimulation: This electromyography test involves sending small electrical impulses to the muscles to measure their response. A decline in the muscle's ability to respond to the electrical stimuli may indicate MG.
3. Blood Tests for Acetylcholine Receptor Antibodies: Presence of antibodies against acetylcholine receptors in the blood is a strong indicator of MG. These antibodies interfere with the communication between the nerve and muscle, leading to symptoms like ptosis.
4. Additional Imaging and Tests: MRI or CT scans may also be performed to rule out thymoma or other conditions that may mimic the symptoms of MG.
Importance of Specialized Medical Evaluation
Given that Myasthenia Gravis and its symptoms like ptosis can fluctuate and be confounded with other neuromuscular diseases, it is crucial to consult specialists in neuromuscular disorders or ophthalmologists familiar with MG for an accurate diagnosis.
Treatment Approaches for Myasthenia Gravis Ptosis
Cholinesterase Inhibitors
● Pyridostigmine (Mestinon): One of the most commonly used cholinesterase inhibitors, pyridostigmine helps improve muscle strength by inhibiting the enzyme that breaks down acetylcholine, a neurotransmitter vital for muscle contraction. This can offer symptomatic relief for ptosis and other muscle weaknesses related to MG.
Immunosuppressive Therapies
● Azathioprine (Imuran) and Mycophenolate Mofetil (CellCept): These immunosuppressants can be effective in the long-term management of MG. They work by dampening the immune response, thus reducing the production of antibodies against acetylcholine receptors.
Corticosteroids
● Prednisone: This medication has anti-inflammatory properties and can help suppress the immune system. It is often used in higher doses initially to gain control over the symptoms and then tapered down to reduce side effects.
Biologic Treatments
● Eculizumab (Soliris) and Rituximab (Rituxan): These newer treatments are designed to target specific parts of the immune system. Eculizumab blocks the activation of the complement system, reducing muscle weakness, while Rituximab targets B cells that produce harmful antibodies.
Surgical Interventions
● Thymectomy: Removal of the thymus gland is an option for some MG patients, as the gland is believed to contribute to the production of harmful antibodies. This option is particularly considered if a tumor (thymoma) is present.
Symptomatic Management
● Eyelid Crutches or Scleral Shell: For patients with severe ptosis, devices such as eyelid crutches fitted onto glasses or a scleral shell can mechanically support the eyelid, improving vision and appearance.
Surgical Interventions
Ptosis Repair
For some patients with Myasthenia Gravis, ptosis can be severe enough to significantly impede vision or impact the quality of life. In such cases, surgical correction, known as ptosis repair, may be considered. The surgery involves tightening the levator muscle, which is responsible for lifting the eyelid. This helps to elevate the eyelid to a more normal position, improving both vision and appearance.
However, surgical intervention for ptosis in the context of MG poses some unique challenges:
● Fluctuating Symptoms: The symptoms of MG, including ptosis, can vary in severity from day to day. This fluctuating nature makes it challenging to determine the appropriate level of surgical correction needed.
● Potential for Exacerbation: Any surgical procedure carries a risk of exacerbating MG symptoms. Therefore, the decision to proceed with surgery should be made carefully, with the full involvement of a team of specialists, including neurologists and ophthalmologists.
● Medication Management: Prior to surgery, medication regimens may be optimized to ensure that the MG symptoms are as controlled as possible. This can include the use of cholinesterase inhibitors or even intravenous immunoglobulin (IVIG) treatments to improve muscle strength temporarily.
● Postoperative Care: Post-surgical care is vital and will often involve close monitoring to ensure that MG symptoms do not worsen. Adjustments to medication may be required, and additional supportive therapies may be initiated.
Long-Term Outlook
Fluctuating Symptoms
One of the most challenging aspects of living with Myasthenia Gravis (MG) is the fluctuating nature of its symptoms, including ptosis. Patients may experience periods of symptom stability, but can also have exacerbations or "flare-ups," where symptoms like ptosis can worsen temporarily. This can be triggered by various factors such as infections, stress, or even changes in medication. The unpredictability of symptom fluctuation necessitates regular monitoring and, sometimes, medication adjustments to manage the condition effectively.
Importance of Consistent Medical Follow-Up
Given the dynamic nature of MG symptoms, consistent medical follow-up is crucial for long-term management. Regular appointments with a healthcare team—comprising neurologists, ophthalmologists, and other specialists—are necessary for:
1. Monitoring Symptoms: Routine checks can help assess the effectiveness of current treatments and make necessary adjustments.
2. Diagnostic Tests: Periodic tests such as repetitive nerve stimulation or blood tests for acetylcholine receptor antibodies may be done to monitor disease progression.
3. Treatment Modifications: As new treatments for MG become available or as your symptoms change, your medication regimen may need to be updated.
4. Managing Complications: Regular monitoring can also help in the early detection of potential complications such as respiratory issues or other eye-related problems.
5. Quality of Life Assessments: Your healthcare team will also want to monitor how MG is affecting your day-to-day life, including any impact on your vision from ptosis, to ensure that the treatment plan is aligned with your quality of life goals.
How to Prevent Myasthenia Gravis Ptosis
Significance of Early Diagnosis
Early diagnosis of Myasthenia Gravis (MG) can make a significant difference in the management of symptoms and overall quality of life for patients. Prompt identification allows for immediate treatment intervention, which is essential in preventing complications and improving long-term outcomes. This is especially crucial when ptosis is a presenting symptom, as timely treatment can mitigate its impact on vision and daily activities.
Proactive Management for Overall Health
● Consistent Medication: Adhering to the prescribed medication schedule is critical for managing MG symptoms effectively. Skipping or delaying doses can exacerbate symptoms like ptosis and contribute to flare-ups.
● Lifestyle Adjustments: Incorporating a balanced diet, adequate hydration, and exercise (as tolerated and recommended) can support overall health, potentially reducing the severity and frequency of MG symptoms, including ptosis.
● Stress Management: Stress is known to trigger or worsen MG symptoms. Stress management techniques such as deep breathing, meditation, or counseling can be beneficial.
● Immunizations: Keeping up-to-date with vaccinations, especially for respiratory illnesses, can prevent complications that could worsen MG symptoms.
● Avoiding Triggers: Some medications like certain antibiotics, muscle relaxants, and beta-blockers can exacerbate MG symptoms. Discuss with your healthcare provider about potential triggers to avoid.
● Education and Advocacy: Being well-informed about the condition and staying updated with the latest research can empower patients to make informed decisions. Support groups and advocacy organizations can provide valuable resources and emotional support.
Summary
Myasthenia Gravis (MG) is an autoimmune neuromuscular disorder that can have a profound impact on muscle strength and control, including the muscles that control the eyelids. Ptosis, or drooping of the eyelids, is often one of the early and common symptoms of MG. Understanding the intricacies of how MG causes ptosis is crucial, as it directly relates to the malfunctioning of acetylcholine receptors and resultant muscle weakness. Diagnostic methods for MG-related ptosis are specialized and can include a variety of tests such as the Tensilon (edrophonium) test, repetitive nerve stimulation, and blood tests.
Treatment for MG-related ptosis is multifaceted, involving medications like cholinesterase inhibitors, immunosuppressive therapies, and corticosteroids. In some cases, surgical intervention may be considered for managing ptosis that severely impacts the patient's quality of life. Long-term outlook and proactive management are key, with regular medical follow-ups essential for monitoring and managing symptoms effectively.
It's imperative for individuals experiencing symptoms of ptosis, particularly when accompanied by other signs of muscle weakness, to seek prompt medical evaluation for an accurate diagnosis. Given the fluctuating nature of MG symptoms, ongoing medical supervision is crucial for effective treatment and improving the quality of life.
FAQ
Myasthenia gravis ptosis is a medical condition characterized by drooping of one or both eyelids due to muscle weakness caused by myasthenia gravis (MG). MG is an autoimmune disorder that affects neuromuscular communication.
(1).jpg)