Horner Syndrome
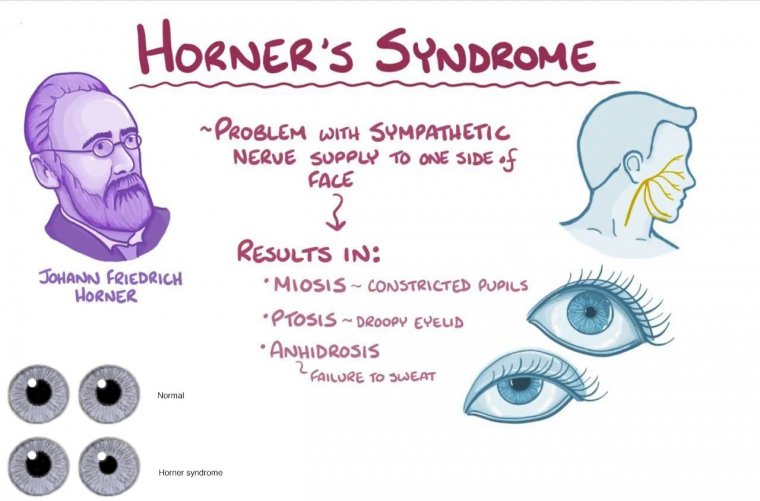
What is Horner’s Syndrome?
Horner's Syndrome is a rare neurological condition that affects the nerves controlling the pupil, eyelid, and facial sweating on one side of the face. It is caused by damage to the sympathetic nervous system, which is responsible for controlling certain involuntary functions of the body.
Horner's Syndrome Causes
There are several possible causes of Horner's syndrome, including:
Trauma
Trauma to the neck or head can cause damage to the sympathetic nerve pathway and lead to Horner's syndrome. Examples of trauma include whiplash injuries, neck surgery, or head injury.
Tumors
Tumors that grow along the sympathetic nerve pathway can compress and damage the nerve fibers, leading to Horner's syndrome. Tumors that can cause Horner's syndrome include lung cancer, neuroblastoma, and tumors of the thyroid gland or carotid artery.
Vascular Disorders
Conditions that affect blood flow to the brainstem or carotid artery can cause Horner's syndrome. Examples of such conditions include atherosclerosis, arterial dissection, and aneurysms.
Neurological Disorders
Certain neurological disorders can cause Horner's syndrome. These include stroke, multiple sclerosis, and syringomyelia.
Infections
In rare cases, infections such as Lyme disease or tuberculosis can cause Horner's syndrome.
Congenital Horner's Syndrome
In some cases, Horner's syndrome may be present at birth due to a congenital abnormality in the sympathetic nerve pathway.
Horner's Syndrome Symptoms
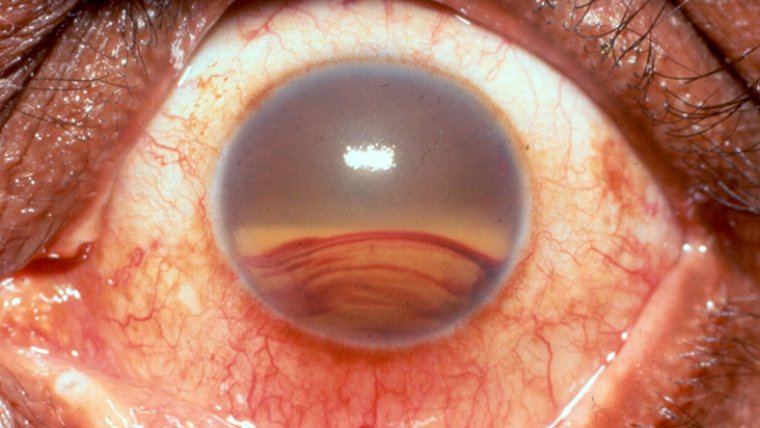
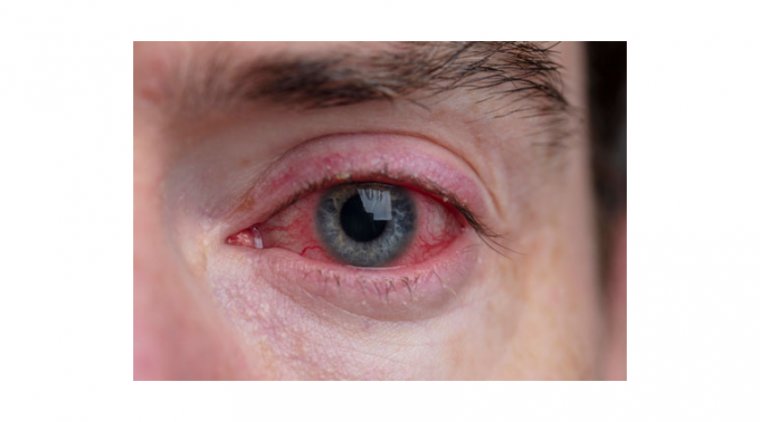
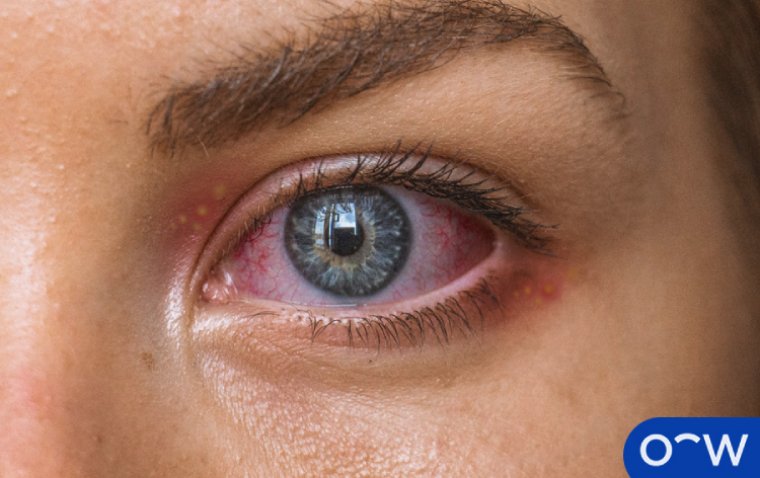
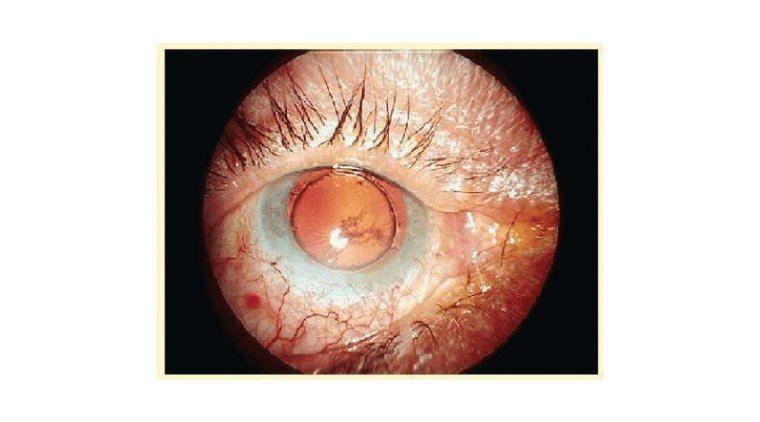
Horner syndrome symptoms include a drooping eyelid, constricted pupil, and decreased sweating on the affected side of the face. It may also cause changes in skin color, a sunken appearance of the eye, and redness of the eye. In some cases, Horner's Syndrome may also cause changes in facial expression and vision. The specific nerves that are affected in Horner's syndrome are the oculosympathetic fibers, which travel from the hypothalamus to the eye and face. These fibers originate in the brainstem and travel down the spinal cord before joining the sympathetic chain in the neck. From there, they ascend through the neck and enter the skull to reach the eye.
Ptosis

Ptosis is a medical condition characterized by the drooping of the upper eyelid. It can affect one or both eyelids and can range in severity from mild to severe. Ptosis can occur at any age, but it is more common in older individuals.
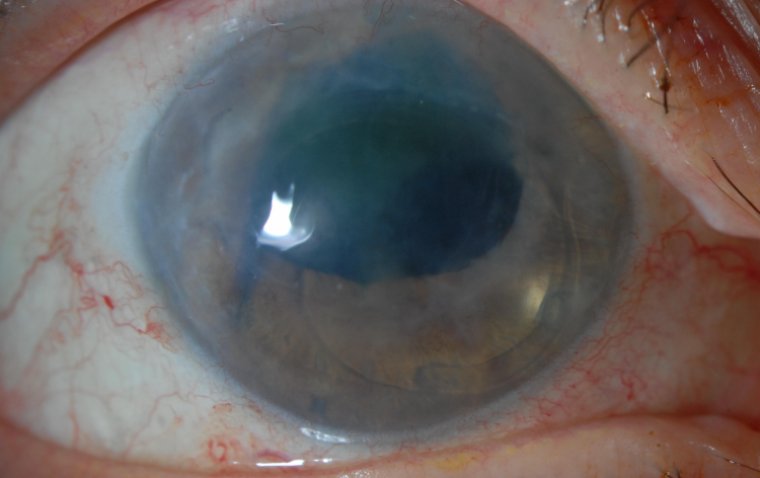
Miosis

Miosis is the medical term for constriction of the pupil, the small, circular opening in the center of the iris (the colored part of the eye). Miosis can cause a range of symptoms, including difficulty seeing in bright light, eye strain, and headaches. It can also lead to other vision problems, such as amblyopia (lazy eye) in children.
Anhidrosis
Anhidrosis is the medical term for reduced sweating, or the inability to sweat normally. The most common symptom of anhidrosis is reduced sweating or the inability to sweat, particularly in response to heat or physical activity. Other symptoms may include dry skin, heat intolerance, and overheating.
Diagnosis of Horner’s Syndrome
Diagnosing Horner's Syndrome involves a thorough physical examination, medical history review, and specialized tests. The diagnosis is based on the presence of the three classic signs: a drooping eyelid (ptosis), a constricted pupil (miosis), and decreased sweating (anhidrosis) on the affected side of the face.
During a physical examination, the healthcare provider may perform a number of tests to assess the patient's pupil size, symmetry, and reactivity. They may also assess the patient's eyelid position and muscle function, as well as the skin temperature and color on the affected side of the face.
Specialized tests may also be performed to help confirm the diagnosis of Horner's Syndrome. One such test is the cocaine test, which involves placing a few drops of a cocaine solution into the affected eye. If the patient has Horner's Syndrome, the affected pupil will not dilate as much as the unaffected pupil.
Other tests that may be used to diagnose Horner's Syndrome include imaging studies, such as CT or MRI scans, to evaluate the brain and neck for any tumors or other abnormalities. Blood tests or other diagnostic procedures may also be recommended to help identify any underlying medical conditions that may be causing the symptoms.
Treatment of Horner’s Syndrome
The treatment for Horner's Syndrome varies depending on the underlying cause and severity of the symptoms. If the condition is due to a temporary or benign cause, such as a mild injury or infection, treatment may not be necessary as the symptoms may resolve on their own over time.
If the cause of Horner's Syndrome is more serious, such as a tumor or other medical condition, the underlying condition will need to be treated in order to alleviate the symptoms of Horner's Syndrome.
In some cases, medications may be prescribed to help manage the symptoms of Horner's Syndrome. For example, eye drops may be used to help alleviate dryness or irritation of the affected eye. Other medications, such as alpha-adrenergic agonists, may be used to help dilate the affected pupil.
Surgery may also be recommended for some cases of Horner's Syndrome. For example, if the condition is caused by a tumor, surgical removal of the tumor may be necessary to alleviate the symptoms of Horner's Syndrome. In some cases, surgery may also be used to correct eyelid drooping or other facial asymmetries caused by the condition.
Physical therapy and rehabilitation may also be recommended for people with Horner's Syndrome. This may include exercises to strengthen the facial muscles, improve eye coordination, or reduce neck and shoulder tension that may exacerbate symptoms.
In addition to medical treatments, lifestyle changes may also be recommended to help manage the symptoms of Horner's Syndrome. For example, people with the condition may be advised to avoid bright lights or sunlight, use sunglasses to protect their eyes, and practice good hygiene to prevent infections.
Retrospective Review
According to Dr Aaron M. Fairbanks, a senior ophthalmology resident at Mayo Clinic, United States, no definitive information is available about the pathologies associated with Horner’s syndrome and the incidence rate in US adults is unknown. Dr. Fairbanks and his associates set out to determine the syndrome's population-based incidence in adults, assess the underlying causes and disease manifestations, and examine the utility of imaging in patients with a neurologically isolated Horner's syndrome because no population-based studies of the syndrome had been conducted in the US.

The researchers retrospectively reviewed each patient's medical records in Olmsted County, Minnesota, who was diagnosed with Horner syndrome between January 1, 2000, and December 31, 2018, using the Rochester Epidemiology Project database. This project claims that the research team looked into the patient charts to determine the proper diagnoses, collected the patient's demographic information, present signs and symptoms, imaging results, and etiologies, and then assessed all of the outcomes.
78 confirmed —out of the 736 patients discovered during the examination of cases—were included in the study. The remaining patients were disqualified due to their non-residency status, the development of their diseases outside the study's time range, or miscoded or inaccurate diagnoses.
Findings
All of the patients were Caucasian, with an average age of 57. During the study period, the age- and sex-adjusted incidence of Horner syndrome was 4.24/100,000/year, with no variation by gender or across time.
The researchers noted that there was a substantial difference between age groups, with older patients having a higher incidence of Horner syndrome. Neurologists made the initial diagnosis in 75% of instances, followed by ophthalmologists, with the majority of diagnoses being made clinically. “Interestingly,” Dr Fairbanks said, “idiopathic cases were more likely to be confirmed with cocaine or apraclonidine eyedrop testing, and stroke, surgical and dangerous causes were more often diagnosed clinically.”
Conclusion
Horner's Syndrome is a rare condition that can cause a range of symptoms and challenges for those affected. However, with proper diagnosis and management, many people are able to live fulfilling lives. If you suspect you may have Horner's Syndrome, it's important to consult with a healthcare professional for proper diagnosis and treatment.
(1).jpg)