The Revolutionary Phacoemulsification Procedure: An In-Depth Look at Modern Cataract Surgery
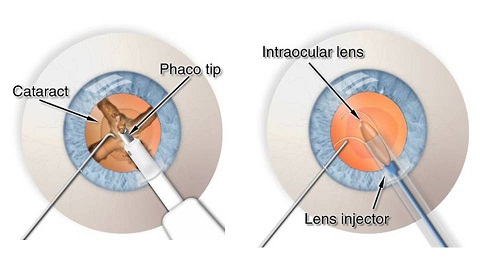
The phacoemulsification procedure has transformed cataract surgery, offering a less invasive and more efficient method for cataract removal. This advanced surgical technique uses ultrasonic vibrations to emulsify the cloudy lens, which is then aspirated out and replaced with an artificial intraocular lens (IOL). This method is favored for its smaller incisions, faster recovery times, and lower risk of complications compared to traditional methods.
What is Phacoemulsification?
The phacoemulsification procedure has become the standard approach in cataract surgery due to its minimally invasive nature. It involves making a small incision in the cornea through which an ultrasonic probe is inserted. This probe emits high-frequency sound waves that emulsify the lens, allowing it to be removed with minimal disruption to the surrounding eye structures. The small incision size, typically less than 3 millimeters, promotes faster healing and reduces the risk of complications such as induced astigmatism.
Phacoemulsification Steps
The phacoemulsification procedure is a meticulous and advanced surgical technique used to remove cataracts and restore clear vision. Here are the detailed steps involved in the process:
1. Anesthesia Use In Phacoemulsification
The procedure begins with the administration of anesthesia to ensure the patient experiences no discomfort during surgery. Typically, local anesthesia is used, which can be administered as eye drops (topical anesthesia) or via an injection around the eye (retrobulbar or peribulbar anesthesia). This step is crucial for numbing the eye and preventing any pain during the phacoemulsification cataract surgery.
2. Incision
A small incision, usually less than 3 millimeters, is made in the cornea, the clear dome-shaped surface that covers the front of the eye. This incision allows the surgeon to insert the surgical instruments needed for the procedure. The size and placement of the incision are designed to minimize disruption and promote faster healing. The incision's precision is a hallmark of the phacoemulsification technique, allowing for a self-sealing wound that typically does not require sutures.
3. Capsulorhexis
In this step, a circular opening is created in the front portion of the lens capsule. This is known as capsulorhexis, and it allows access to the cataractous lens. The opening must be perfectly circular and centered to ensure the effective removal of the lens and the stable placement of the intraocular lens (IOL). The precision of this step is vital for the overall success of the phacoemulsification procedure.
4. Ultrasonic Emulsification
An ultrasonic probe is then inserted through the incision to emulsify the cataract. This probe emits high-frequency sound waves that break up the cloudy lens into tiny fragments. This process is known as phacoemulsification. The emulsified lens material is then aspirated out of the eye using a gentle suction mechanism. The ability to emulsify and aspirate the lens material through a small incision is a key advantage of the phacoemulsification technique over traditional methods.
5. Lens Aspiration
After the cataract has been emulsified, the fragmented lens material is aspirated out of the eye. This step ensures that all remnants of the cloudy lens are removed, leaving the capsular bag clear and ready for the new lens. The aspiration process is carefully controlled to prevent any damage to the surrounding eye structures, particularly the delicate posterior capsule.
6. Intraocular Lens (IOL) Implantation
Once the cataract has been completely removed, an artificial intraocular lens (IOL) is implanted into the eye. The IOL is folded and inserted through the same small incision, where it unfolds and is positioned within the capsular bag. The IOL restores the eye's focusing ability, providing clear vision. This step completes the phacoemulsification procedure.
7. Wound Closure
The small incision made at the beginning of the surgery is designed to be self-sealing. This means that, in most cases, no stitches are required to close the wound. The self-sealing nature of the incision helps to reduce the risk of infection and promotes a quicker recovery. The surgeon will ensure that the incision is secure before concluding the surgery.
Each step of the phacoemulsification procedure is performed with precision and care, utilizing advanced phacoemulsification equipment and machines to ensure the best possible outcome for the patient.
Pre-Operative Preparation
Proper pre-operative preparation is crucial for the success of the phacoemulsification procedure. Ensuring that the patient is well-prepared helps minimize risks and optimize surgical outcomes. Here are the key steps involved in the pre-operative preparation for phacoemulsification cataract surgery:
1. Comprehensive Eye Examination
The first step in preparing for phacoemulsification is a thorough eye examination conducted by an ophthalmologist. This examination includes measuring the size and shape of the eye to determine the appropriate intraocular lens (IOL) for implantation. Tests such as biometry and keratometry are performed to calculate the correct IOL power, ensuring optimal visual outcomes post-surgery.
2. Medical History Review
A detailed review of the patient’s medical history is essential. This includes discussing any existing medical conditions, allergies, and medications currently being taken. Certain medications, especially those affecting blood clotting, may need to be adjusted before the surgery. The ophthalmologist will also inquire about any previous eye surgeries or conditions that might impact the phacoemulsification procedure.
3. Anesthesia Consultation
Since phacoemulsification cataract surgery is typically performed under local anesthesia, an anesthesia consultation may be required. The anesthesia used can be topical (eye drops) or regional (injection around the eye). The anesthesiologist will determine the most suitable type based on the patient’s health and comfort levels. Understanding the anesthesia plan helps the patient know what to expect during the surgery.
4. Patient Instructions

Patients are given specific pre-operative instructions to follow. These typically include:
● Fasting: Patients may be advised to avoid eating or drinking for several hours before the surgery to reduce the risk of complications.
● Medications: Instructions on whether to continue or temporarily stop certain medications will be provided. For example, blood thinners may need to be paused to prevent excessive bleeding during the procedure.
● Hygiene: Patients are often instructed to avoid applying makeup, lotions, or perfumes on the day of the surgery to maintain sterility in the surgical area.
5. Use of Pre-Operative Eye Drops
Pre-operative eye drops may be prescribed to reduce the risk of infection and inflammation. These drops are typically started a few days before the surgery. Antibiotic and anti-inflammatory drops help prepare the eye and ensure it is in the best possible condition for the procedure.
6. Transportation Arrangements
Since phacoemulsification is usually performed on an outpatient basis, patients need to arrange for transportation to and from the surgical center. The effects of anesthesia can impair vision and coordination temporarily, making it unsafe for patients to drive themselves.
7. Discussion of Risks and Benefits
A thorough discussion of the phacoemulsification procedure’s risks and benefits is an essential part of pre-operative preparation. The ophthalmologist will explain potential complications and the expected recovery process. This discussion helps set realistic expectations and allows patients to make informed decisions about their eye health.
By meticulously preparing for the phacoemulsification procedure, both patients and healthcare providers can contribute to a smooth surgical experience and favorable outcomes.
Post-Operative Care for Phacoemulsification
Proper post-operative care is crucial to ensure a smooth recovery and optimal visual outcomes after the phacoemulsification procedure. Following the guidelines provided by your ophthalmologist will help minimize the risk of complications and promote healing. Here are the key components of post-operative care for phacoemulsification cataract surgery:
1. Use of Prescribed Eye Drops
Patients are typically prescribed a regimen of eye drops to use after the surgery. These include antibiotics to prevent infection, anti-inflammatory drops to reduce swelling, and sometimes steroid drops to control inflammation. It is essential to use these drops as directed to ensure proper healing and avoid complications.
2. Activity Restrictions
After the phacoemulsification procedure, patients should avoid activities that could strain the eyes or increase intraocular pressure. This includes heavy lifting, bending over, and strenuous exercise. Protecting the eye from potential trauma is vital during the initial recovery period.
3. Wearing Protective Eyewear
To prevent accidental rubbing or injury to the eye, patients are often advised to wear protective eyewear, especially while sleeping. An eye shield or goggles can help safeguard the eye during the delicate healing process.
4. Avoiding Contaminants After Phacoemulsification
It is important to keep the eye clean and avoid exposure to dust, smoke, and water. Patients should refrain from swimming or using hot tubs until their ophthalmologist confirms it is safe. Additionally, avoiding makeup around the eye can help prevent infections.
5. Follow-Up Appointments
Regular follow-up appointments with the ophthalmologist are critical to monitor the healing process. These visits allow the doctor to check for signs of infection, inflammation, or other complications. Adjustments to medications and care routines can be made based on these evaluations.
6. Managing Discomfort After Phacoemulsification
Some discomfort, mild pain, or itching is normal after phacoemulsification cataract surgery. Over-the-counter pain relievers can be used to manage these symptoms. However, any severe pain or sudden vision changes should be reported to the ophthalmologist immediately.
● Vision Adjustments
Patients may experience fluctuations in vision during the recovery period. It is important to give the eyes time to heal and adjust to the new intraocular lens (IOL). Typically, vision stabilizes within a few weeks, but full recovery can take up to a few months.
● Recognizing Complications
Being aware of potential phacoemulsification complications is important for prompt intervention. Signs of complications include persistent pain, significant vision changes, increased redness, or discharge from the eye. Reporting these symptoms to the ophthalmologist promptly can help address issues before they worsen.
By diligently following these post-operative care instructions, patients can ensure a smooth recovery and enjoy the benefits of the phacoemulsification procedure.
Benefits of Phacoemulsification
The phacoemulsification procedure offers numerous advantages over traditional cataract surgery methods, making it the preferred choice for many ophthalmologists and patients. Here are some key benefits of phacoemulsification:
1. Smaller Incisions
One of the primary benefits of the phacoemulsification technique is the use of smaller incisions. Typically, incisions are less than 3 millimeters, which helps to reduce surgical trauma. Smaller incisions lead to quicker healing and a lower risk of infection and other complications.
2. Faster Recovery Time
Due to the minimally invasive nature of the phacoemulsification procedure, patients experience faster recovery times compared to traditional methods. Most patients notice significant improvement in their vision within a few days, and the overall recovery period is shorter, allowing for a quicker return to normal activities.
3. Reduced Risk of Complications
The precision of the phacoemulsification process and the use of advanced phacoemulsification equipment reduce the risk of complications during and after surgery. The smaller incisions and controlled ultrasonic emulsification lower the chances of induced astigmatism and other intraoperative complications.
4. Improved Visual Outcomes
Phacoemulsification cataract surgery generally results in better visual outcomes. The precise removal of the cataractous lens and the stable placement of the intraocular lens (IOL) contribute to clearer and more stable vision post-surgery.
5. Less Postoperative Discomfort
Patients undergoing the phacoemulsification procedure typically experience less postoperative discomfort compared to those who undergo traditional cataract surgery. The smaller incisions and less invasive nature of the procedure mean less irritation and faster healing of the surgical site.
6. Higher Precision
The use of ultrasonic vibrations to emulsify the cataract allows for a high degree of precision. This technology enables the surgeon to remove the lens efficiently without affecting the surrounding tissues, leading to more predictable and successful surgical outcomes.
7. Versatility and Adaptability
The phacoemulsification technique is versatile and can be adapted to suit various types of cataracts. This flexibility makes it an excellent choice for a wide range of patients, including those with different levels of cataract severity.
8. Improved Patient Satisfaction
Due to the combination of smaller incisions, faster recovery, and better visual outcomes, patient satisfaction with phacoemulsification cataract surgery is generally high. Patients appreciate the quick return to daily activities and the significant improvement in their quality of life.
The benefits of phacoemulsification make it a superior option for cataract surgery, providing patients with a safer, more efficient, and highly effective treatment for cataracts.
Risks and Complications of Phacoemulsification Surgery

While the phacoemulsification procedure is generally safe and highly effective, like any surgical intervention, it carries potential risks and complications. Understanding these risks helps patients make informed decisions and prepares them for the post-operative period. Here are some of the possible complications associated with phacoemulsification cataract surgery:
1. Intraoperative Complications
● Capsular Tears: During the phacoemulsification technique, a tear in the lens capsule can occur. This complication may require additional surgical steps to stabilize the lens implant.
● Corneal Burns: The ultrasonic probe used in phacoemulsification generates heat, which, if not properly managed, can cause burns to the cornea. This risk is mitigated by using cooling irrigation fluids and careful surgical technique.
● Zonular Dehiscence: The fibers that hold the lens in place (zonules) can become damaged during the procedure, leading to instability of the lens implant.
2. Postoperative Complications of Phacoemulsification
● Infection (Endophthalmitis): Although rare, infection inside the eye can occur, which is a serious complication requiring immediate treatment with antibiotics. Proper sterilization techniques and the use of antibiotic eye drops help minimize this risk.
● Increased Intraocular Pressure: Some patients may experience elevated intraocular pressure following surgery, which can be managed with medication or additional procedures if necessary.
● Inflammation: Post-operative inflammation is common and typically managed with anti-inflammatory eye drops. Persistent inflammation may require extended treatment.
● Posterior Capsular Opacification (PCO): Also known as secondary cataract, this complication occurs when the back of the lens capsule becomes cloudy after surgery. PCO can be treated with a quick and painless laser procedure known as YAG laser capsulotomy.
3. Retinal Complications
● Retinal Detachment: Although rare, the risk of retinal detachment increases slightly after cataract surgery. Symptoms such as flashes of light, floaters, or a shadow in the field of vision should be reported immediately to an ophthalmologist.
● Cystoid Macular Edema (CME): This condition involves swelling of the central retina and can affect vision. CME is usually treated with anti-inflammatory medications.
4. Visual Disturbances
● Dislocation of the Intraocular Lens (IOL): In some cases, the implanted lens may become displaced. This may require surgical repositioning of the IOL.
● Astigmatism: Though the risk is reduced with phacoemulsification, some patients may experience changes in the shape of the cornea, leading to astigmatism. Corrective lenses or additional procedures may be needed to address this issue.
Despite these potential risks and complications, the phacoemulsification procedure is widely regarded as safe and effective, with a high success rate and a low incidence of serious complications.
How Much Does Phacoemulsification Cost in 2024?
The phacoemulsification procedure’s cost can vary significantly depending on various factors such as geographic location, the surgeon's expertise, and the specifics of the procedure itself. Here is a detailed overview of the cost considerations for phacoemulsification cataract surgery:
1. Cost in the United States
In the U.S., the cost of phacoemulsification typically ranges from $2,100 to $4,000 per eye. This variation is influenced by factors such as the surgeon’s fees, facility costs, and the type of intraocular lens (IOL) implanted during the procedure.
2. Cost in the United Kingdom
In the UK, the cost ranges from £1,700 to £3,500 per eye. This range reflects differences in private clinic fees, the complexity of the surgery, and additional services such as pre- and post-operative care.
3. Cost in Türkiye
Turkiye offers more affordable options for phacoemulsification surgery, with costs ranging from $700 to $1,500 per eye. This lower cost can be attributed to the generally lower cost of medical services in Turkiye compared to Western countries. Despite the lower cost, the quality of care in reputable clinics and hospitals is comparable to international standards.
4. Insurance Coverage
In many cases, phacoemulsification surgery is covered by health insurance policies, particularly if the surgery is deemed medically necessary due to significant vision impairment. Medicare in the U.S. typically covers the cost of cataract surgery if certain criteria are met. Private insurance plans may also provide coverage, but it is essential to check with the insurance provider to understand the specifics of what is covered and any out-of-pocket expenses that might be incurred.
1. Factors Influencing Cost
● Surgeon’s Expertise: Experienced surgeons may charge higher fees, but their expertise can result in better outcomes and lower complication rates.
● Type of IOL: Premium IOLs, such as those correcting astigmatism or providing multifocal vision, can increase the overall cost of the procedure.
● Facility Fees: Surgery performed in a hospital may be more expensive than in an outpatient surgical center due to higher facility charges.
● Geographic Location: The cost can vary significantly depending on the region, with urban areas typically having higher costs compared to rural areas.
Understanding these cost considerations is crucial for patients planning to undergo the phacoemulsification procedure. It helps in budgeting for the surgery and making informed decisions about where to have the procedure done. Additionally, exploring options such as medical loans or financing plans offered by clinics can help manage the financial aspect of this sight-restoring surgery.
Patient Experiences

The phacoemulsification procedure has significantly improved the quality of life for many patients undergoing cataract surgery. Here are some real testimonials and common questions addressed by those who have undergone the procedure.
1. Patricia Gray (London Ophthalmology Centre)
Procedure: Bilateral phacoemulsification with intraocular lens (IOL) implantation
Experience: Patricia had a successful bilateral phacoemulsification surgery, leading to a significant improvement in her vision. She appreciated the detailed pre-operative consultations and the compassionate post-operative care provided by her surgeon. The rapid recovery allowed her to return to her daily activities much sooner than expected, experiencing minimal discomfort during the healing process. (https://londonoc.co.uk/testimonials-press/)
2. Chief JA (London Ophthalmology Centre)
Procedure: Right Xen implant and left microincision phacoemulsification with IOL.
Outcome: Chief JA experienced a significant reduction in intraocular pressure and an improvement in visual clarity. He praised the professionalism and expertise of the surgical team, which he described as world-class, and highlighted the comprehensive care received during his recovery period. (https://londonoc.co.uk/testimonials-press/)
3. Patient at Lotus Vision (Dr. Nemi, Alpharetta, GA)
Procedure: Phacoemulsification cataract removal
Experience: A patient at Lotus Vision reported excellent results following their phacoemulsification procedure. They found the use of advanced technology, such as the Centurion Vision System, to significantly enhance the precision and outcome of the surgery. The patient experienced minimal discomfort and a quick recovery, allowing them to resume normal activities within a few days. (https://www.lotusvision.com/cataract/cataract-surgery-atlanta/phacoemulsification/)
Summary
The phacoemulsification procedure, considered the gold standard in cataract surgery, employs ultrasonic vibrations to delicately remove clouded lenses, replacing them with artificial intraocular lenses (IOLs). This minimally invasive technique, marked by small incisions, swift recoveries, and reduced complications compared to traditional methods, has revolutionized vision restoration. Its meticulous steps include anesthesia administration, precise incisions, lens emulsification, IOL implantation, and wound closure. Phacoemulsification boasts superior benefits, including quicker healing, less postoperative discomfort, and improved visual outcomes.
However, like any surgery, it carries risks such as infection and retinal complications, though these are rare. With costs varying by location and factors like surgeon expertise and IOL type, patients benefit from understanding these aspects to make informed decisions. Patient testimonials underscore the transformative impact of phacoemulsification, celebrating enhanced vision and restored quality of life.
(1).jpg)