Unraveling the Mystery of Pigment Dispersion Syndrome
What Is Pigment Dispersion Syndrome?
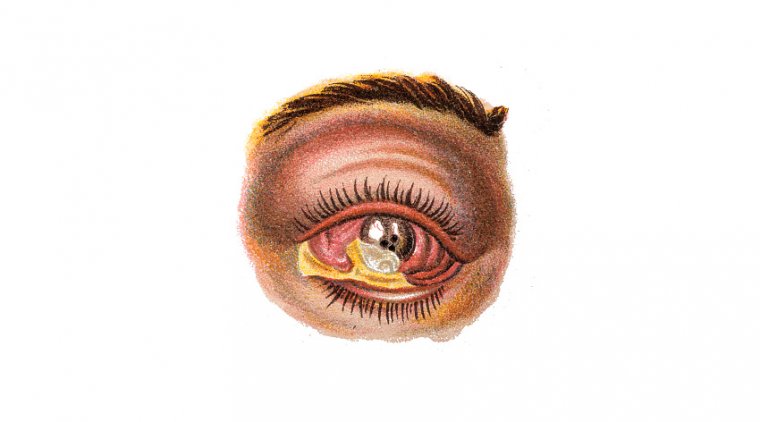
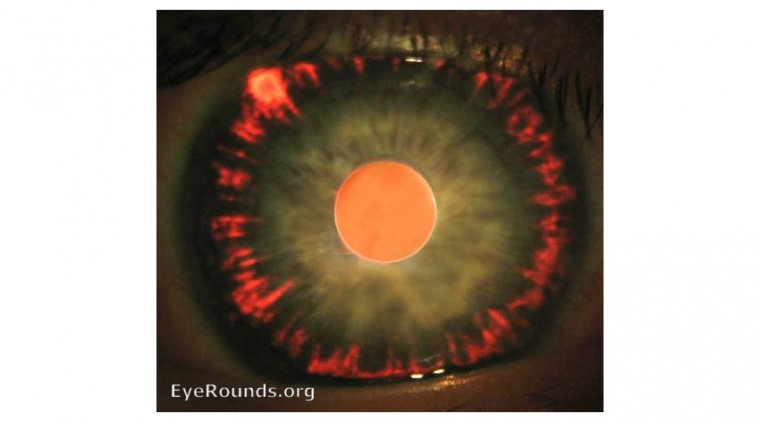
In the world of ophthalmology, some conditions are well-known and widely discussed, while others remain shrouded in mystery. One such enigmatic condition is pigment dispersion syndrome (PDS), a disorder that affects the eyes and can potentially lead to more severe complications. PDS is characterized by the dispersion of pigment granules within the eye, which can block the eye's drainage system and consequently increase intraocular pressure.
Pigment dispersion syndrome occurs when the pigment granules, which typically reside in the iris, are released into the aqueous humor – the clear fluid that fills the front part of the eye. Over time, these pigment particles can accumulate in the eye's drainage system, known as the trabecular meshwork, leading to reduced outflow of the aqueous humor. This blockage can eventually result in increased intraocular pressure and, if left untreated, may progress to pigmentary glaucoma, a potentially sight-threatening condition.
In this article, we will delve into the enigma of pigment dispersion syndrome, exploring its causes, symptoms, diagnosis, and treatment options. By shedding light on this lesser-known eye disorder, we aim to raise awareness and promote early detection and intervention, ultimately safeguarding the gift of sight.
What Causes Pigment Dispersion Syndrome?
Although the precise cause of pigment dispersion syndrome remains uncertain, several factors are believed to contribute to the development of this eye disorder. These factors can be classified into genetic predisposition, age, and refractive errors like high myopia (nearsightedness). Let's take a closer look at each of these factors:
● Genetic predisposition: There appears to be a genetic component to pigment dispersion syndrome, as it tends to run in families. Studies have shown that individuals with a family history of PDS or pigmentary glaucoma are at a higher risk of developing the condition. However, the exact genes involved in the development of PDS have yet to be identified.
● Age: Pigment dispersion syndrome typically affects individuals between the ages of 20 and 40, with the onset often occurring in early adulthood. Although PDS can affect people of all ages, the prevalence of the condition decreases with age, possibly due to anatomical changes in the eye.
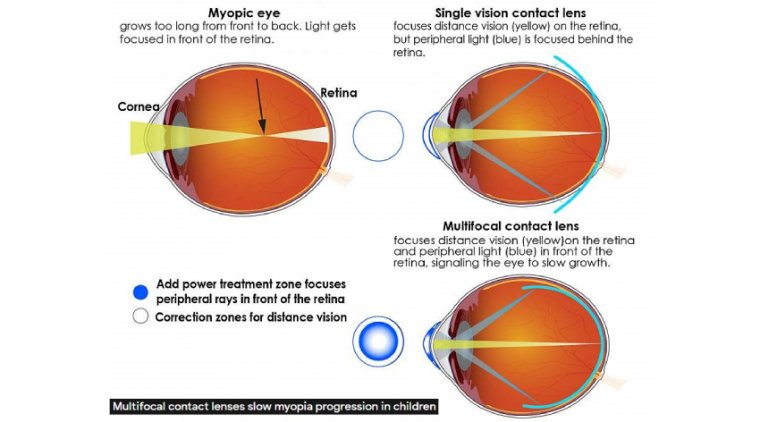
● High myopia (nearsightedness): Individuals with high myopia, or severe nearsightedness, may be at an increased risk of developing pigment dispersion syndrome. High myopia can cause structural changes in the eye, such as a more concave iris shape, which can contribute to the rubbing of the iris against the lens or other eye structures, leading to pigment dispersion.
It's important to note that not everyone with these risk factors will develop pigment dispersion syndrome. The complex interplay of genetic, anatomical, and environmental factors likely determines the development and progression of this condition. Further research is needed to fully understand the underlying mechanisms of PDS and develop more targeted prevention and treatment strategies.
Symptoms of Pigment Dispersion Syndrome
Pigment dispersion syndrome can present with a variety of symptoms, ranging from subtle to more noticeable. In some cases, individuals with PDS may not experience any symptoms at all, making the condition difficult to detect without a comprehensive eye examination. Here are some common symptoms associated with pigment dispersion syndrome:
● Blurred vision: Individuals with PDS may experience episodes of blurred or hazy vision, particularly after engaging in activities that cause the eyes to dilate, such as exercising or being in a dimly lit environment. The dispersion of pigment granules can lead to increased intraocular pressure, which can temporarily affect vision quality.
● Eye pain: Some people with PDS may experience mild to moderate eye pain or discomfort, often described as a dull ache or pressure sensation. This discomfort can be attributed to the increased intraocular pressure associated with the condition.
● Halos around lights: The presence of pigment granules in the aqueous humor can cause light to scatter, resulting in halos or glare around lights, particularly in low-light conditions or at night.
● Floaters: Some individuals with PDS may notice floaters, which are small specks or spots that drift across the field of vision. Floaters can occur when pigment granules are released into the vitreous gel that fills the back of the eye.
Asymptomatic cases: In many instances, people with pigment dispersion syndrome may not experience any noticeable symptoms. These asymptomatic cases can pose a challenge for early detection and intervention, emphasizing the importance of regular eye examinations, especially for those with known risk factors.
Treatment of Pigment Dispersion Syndrome
The primary goal of treating pigment dispersion syndrome is to manage intraocular pressure, prevent the progression of the condition, and reduce the risk of complications such as pigmentary glaucoma. Treatment options may vary depending on the severity of the condition and the specific needs of the individual. Here are some common treatment options for pigment dispersion syndrome:
1. Eye drops: Medications in the form of eye drops are often the first line of treatment for PDS. These medications aim to reduce intraocular pressure by either increasing the outflow of aqueous humor or decreasing its production. Common types of eye drops used to manage PDS include prostaglandin analogs, beta-blockers, alpha agonists, and carbonic anhydrase inhibitors.
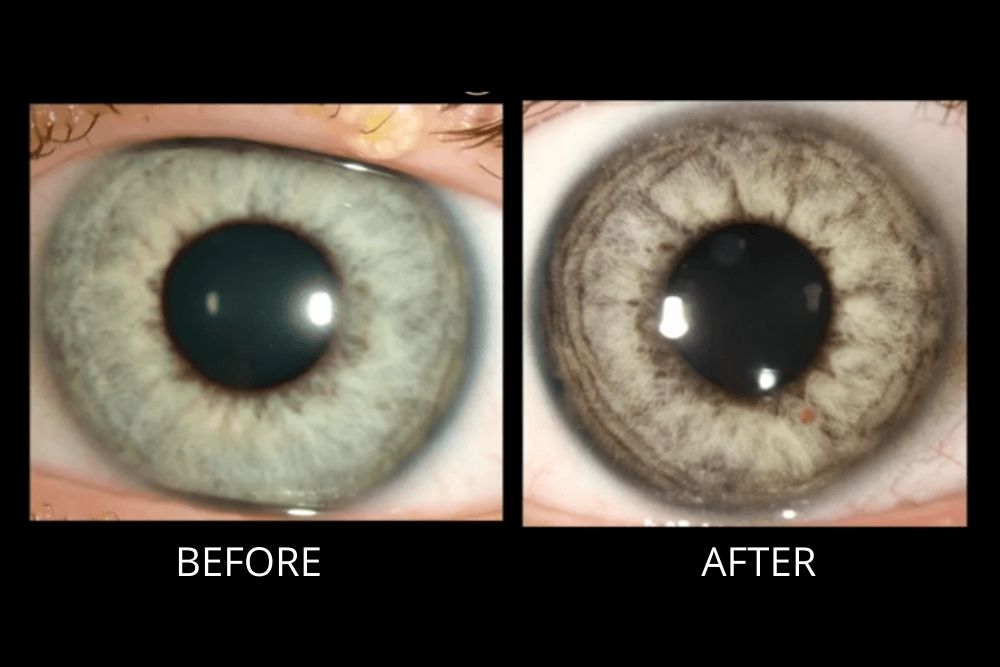
2. Laser surgery: In cases where eye drops are insufficient or not well-tolerated, laser surgery may be considered. Laser trabeculoplasty is a procedure that involves using a laser to create small openings in the trabecular meshwork, improving the drainage of aqueous humor and reducing intraocular pressure. This minimally invasive procedure can be performed in an outpatient setting and has a relatively low risk of complications.
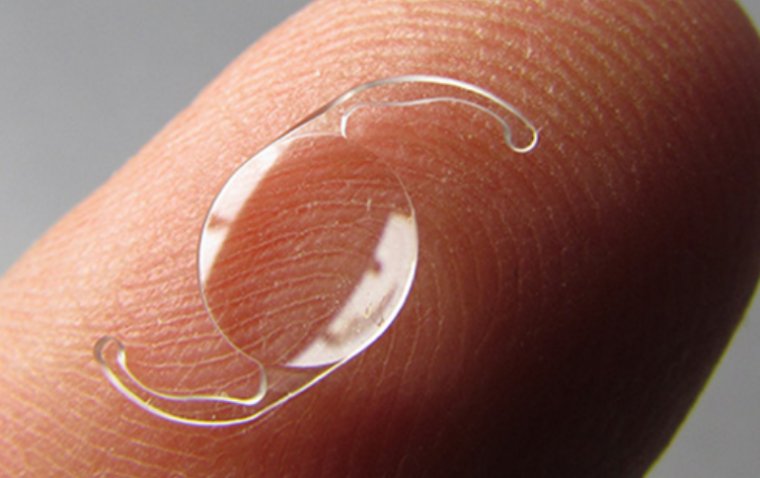
3. Surgery: In more severe cases or when other treatments have failed, surgical interventions may be necessary. Trabeculectomy is a surgical procedure that involves creating a small drainage channel in the eye to allow the aqueous humor to bypass the blocked trabecular meshwork, thereby reducing intraocular pressure. Alternatively, implantation of a glaucoma drainage device may be considered, which involves inserting a small tube to help drain the aqueous humor from the eye.
4. Lifestyle modifications: Although not a direct treatment for PDS, certain lifestyle changes may help manage the condition and support overall eye health. These changes may include maintaining a healthy weight, avoiding activities that cause rapid eye dilation, and wearing protective eyewear during sports or other activities that pose a risk of eye injury.
Can Pigment Dispersion Syndrome Be Prevented?
While it may not be possible to completely prevent pigment dispersion syndrome, particularly in individuals with a genetic predisposition, there are steps that can be taken to manage the condition and reduce the risk of complications. Here are some tips to help manage pigment dispersion syndrome:
1. Regular monitoring by a healthcare professional: Regular eye examinations are essential for early detection and management of pigment dispersion syndrome. If you have a family history of PDS or pigmentary glaucoma, inform your eye care professional, and schedule regular check-ups to monitor for any changes in your eye health.
2. Maintain a healthy lifestyle: A balanced diet, regular exercise, and maintaining a healthy weight can contribute to overall eye health and help manage conditions like PDS. However, it's important to avoid activities that may rapidly dilate the eyes or increase intraocular pressure, such as heavy weightlifting or intense cardiovascular exercises, as these can exacerbate pigment dispersion.
3. Avoid strenuous exercise or activities that may increase intraocular pressure: High-impact sports or activities that involve rapid eye dilation can cause pigment granules to disperse and accumulate in the trabecular meshwork, increasing intraocular pressure. Opt for low-impact exercises like swimming, walking, or yoga, and discuss any concerns with your eye care professional to determine which activities are safe for you.
4. Wear proper eye protection: To minimize the risk of eye injury, which could potentially worsen pigment dispersion syndrome, wear appropriate protective eyewear during sports or other activities that pose a risk of eye injury. This includes polycarbonate lenses, which offer a high level of impact resistance, and sports goggles with padding around the rims for additional protection.
To Conclude...
As we bring this journey of unraveling the mystery of pigment dispersion syndrome to a close, let's not lose sight of the key points we've illuminated along the way. Pigment dispersion syndrome, although lesser-known, is a significant eye disorder that can lead to complications like pigmentary glaucoma if left untreated.
While the precise cause of PDS remains a bit "hazy," we know that genetic predisposition, age, and high myopia can contribute to its development. Symptoms may include blurred vision, eye pain, halos around lights, or, in some cases, no symptoms at all. Early detection, regular monitoring, and prompt treatment are vital to managing PDS and preventing long-term vision loss.
Treatment options can range from eye drops to laser surgery and, in severe cases, surgical intervention. Although complete prevention of pigment dispersion syndrome may be out of reach, we can still keep an eye on managing the condition by adopting a healthy lifestyle, avoiding activities that may worsen the condition, and wearing proper eye protection.
In the end, understanding the enigma of pigment dispersion syndrome is the first step towards protecting our most precious gift – our vision. So, don't turn a blind eye to the importance of regular eye exams, early detection, and appropriate treatment. After all, seeing is believing!
(1).jpg)