What Is Posterior Capsular Opacification and How to Manage It
What Is Post-Capsular Opacification?
After a smooth sail through cataract surgery, post capsular opacification (PCO) can appear like a rogue wave, unexpected and potentially disruptive. It's not an iceberg that sinks the ship, but it's certainly worth keeping an eye on.
PCO, also known as 'secondary cataract,' is a common complication that may occur following cataract surgery. Despite its colloquial name, it isn't a new cataract, but rather an opacification, or clouding, of the posterior lens capsule – the thin, transparent membrane left intact during surgery to support the intraocular lens implant.
The posterior lens capsule is usually crystal clear following cataract surgery, providing an unobstructed path for light to reach the retina. However, in PCO, residual lens epithelial cells left behind after surgery proliferate, migrate, and undergo fibrous metaplasia or lens fiber regeneration, causing the capsule to become hazy.
The impact on visual acuity can be akin to looking through a frosted glass window. Common symptoms experienced by affected individuals may include blurred vision, difficulty with bright lights, and experiencing glare or a sense of 'halo' around lights. Though this 'foggy' situation may seem disheartening, fear not – managing PCO is usually straightforward and can bring clear skies back into the patient's view.
Causes and Risk Factors for Post-Capsular Opacification
Just as diverse winds can steer a ship off its intended course, a variety of factors can influence the development of post capsular opacification. Let's unfurl the sails and explore these potential navigational hazards.
Post capsular opacification primarily results from the proliferation and abnormal differentiation of residual lens epithelial cells left on the lens capsule during cataract surgery. Despite the surgeon's best efforts, it's almost impossible to remove all of these cells during the procedure.
Several risk factors can contribute to an increased likelihood of developing PCO. These include:
● Patient Age: Younger patients tend to have a higher risk of developing PCO, likely due to the more vigorous cellular activity in their lens capsules.
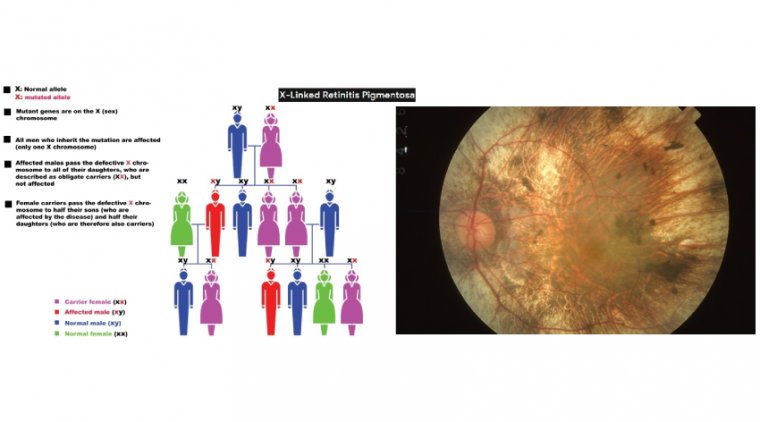
● Pre-existing Eye Conditions: Certain eye conditions, such as high myopia, retinitis pigmentosa, or uveitis, can increase the risk of PCO.
● Surgical Techniques: Specific surgical methods or decisions, such as the technique used for capsulorhexis, the degree of cortical cleanup, and the use of intraoperative anti-inflammatory drugs, can influence the risk.
● Lens Implant Types: The design, material, and edge profile of the intraocular lens (IOL) used during surgery can also affect the development of PCO.
Signs and Symptoms of Post-Capsular Opacification
Navigating the sea of post capsular opacification can sometimes feel like charting a course through a fog bank. While the journey might begin with clear skies, the signs and symptoms of PCO can gradually creep in, much like an encroaching mist.
Decreased visual acuity is often the first sign that alerts patients and their ophthalmologists to the presence of PCO. The world may start to seem less sharp, less vivid, as if obscured by a semi-transparent veil.
Glare or halos around lights can also serve as harbingers of PCO, especially noticeable in low light or night-time conditions. For the affected individual, oncoming headlights or street lamps may appear to be surrounded by a hazy ring or bright streaks of light, making night-time navigation a challenge.
Progressive decline in vision clarity is another common symptom. Unlike the sudden onset of cataract symptoms, PCO tends to roll in slowly, subtly reducing visual quality over weeks or months.
Other symptoms that may occasionally hoist their flags include blurred vision, double vision, or a reduction in contrast sensitivity, making it difficult for individuals to perceive subtle differences in shades or textures.
How to Diagnose Post-Capsular Opacification
Identifying post-capsular opacification requires a keen eye and a careful examination process, much like spotting a lighthouse on a foggy night.
The diagnostic journey for PCO begins with a comprehensive eye examination. The ophthalmologist will ask the patient about their symptoms and perform a detailed assessment of the eye, including an examination of the posterior capsule using a slit lamp. This instrument provides a magnified view of the eye's structures and can reveal any opacification of the posterior capsule.
Visual acuity tests form a significant part of this examination. These tests are used to quantify the patient's visual impairment and monitor its progression over time. They range from the standard Snellen chart - the one with progressively smaller letters - to more complex assessments like contrast sensitivity tests or glare testing.
Specific assessments of the posterior capsule are often necessary to confirm the diagnosis of PCO. These may involve imaging techniques such as optical coherence tomography (OCT), which can provide detailed images of the capsule and help determine the extent of the opacification.
The differential diagnoses that need to be considered form a wide array. Other causes of visual impairment or complications following cataract surgery, such as cystoid macular edema, retinal detachment, or IOL dislocation, need to be ruled out before confirming the diagnosis of PCO.
The diagnostic process for PCO is akin to navigating through uncharted waters; it requires careful observation, precise measurement, and an understanding of the surrounding seascape to arrive at the correct destination.
Treatment Options for Post-Capsular Opacification
Setting sail for the shores of effective treatment for post capsular opacification, we're met with a handful of potent solutions. As an ophthalmologist, it's our duty to choose the one best suited for our patient's unique circumstances.
Arguably, the flagship treatment for PCO is a procedure known as a posterior capsulotomy. This non-invasive technique, akin to parting a cloudy sea, involves creating a small opening in the cloudy posterior capsule, allowing light to pass through unobstructed and restore clear vision. This is typically done using a method called Nd:YAG laser capsulotomy. It's an outpatient procedure, meaning patients can go home the same day, and it usually takes less than half an hour.
Laser-assisted capsulotomy has become the gold standard in treating PCO, owing to its effectiveness and safety. During the procedure, the laser creates an opening in the center of the posterior capsule without damaging the surrounding eye structures or the intraocular lens. The laser settings are carefully calibrated to achieve the best possible results.
In some cases, if the opacification is extensive or the laser procedure is not advisable, surgical techniques may be employed to address the opacification and improve visual outcomes. This might involve manually removing the cloudy capsule or even replacing the intraocular lens in some situations.
How to Prevent Post-Capsular Opacification
In our quest to keep the waters of our patient's ocular health crystal clear, prevention plays a vital role, just as a seasoned sailor would stay vigilant to avoid a brewing storm.
The prevention of post-capsular opacification is primarily linked to the cataract surgery itself. The surgical techniques employed can have a profound effect on the likelihood of developing PCO. Certain maneuvers during surgery, such as ensuring complete removal of cortical material and polishing the posterior capsule, can decrease the incidence of opacification.
The type of intraocular lens (IOL) used during cataract surgery also holds sway over the risk of PCO. Certain IOL designs and materials are associated with a lower rate of opacification. For instance, hydrophobic acrylic IOLs have been shown to exhibit lower PCO rates than other types.
Adjunctive therapies may also serve as auxiliary sails, aiding in our journey towards PCO prevention. For example, the application of anti-mitotic drugs during surgery or postoperative use of non-steroidal anti-inflammatory drugs (NSAIDs) may reduce the incidence of PCO.
Navigating these preventative measures requires knowledge, expertise, and adaptability - not unlike a skilled mariner charting a course through challenging waters. But with our compass set firmly on the goal of achieving the best possible outcomes for our patients, we can confidently steer clear of the stormy seas of post-capsular opacification.
Latest Research and Advances in Post-Capsular Opacification
As the world of ophthalmology continues to unfurl its vast expanses, research, and advancements in the field of post-capsular opacification are making waves in improving patient outcomes.
Recent years have witnessed a surge in research efforts focused on developing innovative treatment approaches for PCO. Among these, studies exploring the use of femtosecond lasers for capsulotomy procedures show promise in enhancing precision and safety. The technology may offer a more controlled and accurate way to create an opening in the posterior capsule, potentially reducing complications and improving visual outcomes.
In the realm of intraocular lens design and materials, innovation is also in full swing. Emerging research is examining the use of novel IOL materials and designs that may reduce the risk of PCO. Biocompatible materials that minimize cellular proliferation on the lens capsule are a particular area of interest.
Additionally, novel drug therapies are being explored to prevent or manage PCO. This includes investigations into pharmacologic agents that can inhibit lens epithelial cell proliferation, migration, or metaplasia, which are key processes leading to PCO development.
The future of post-capsular opacification management looks bright with these advancements on the horizon. Like a lighthouse guiding ships through dark waters, these scientific strides offer the hope of safer journeys and clearer visions for our patients.
To Conclude...
As we close the lids on our comprehensive examination of posterior capsular opacification (PCO), it becomes ever more apparent that our journey in ophthalmology is not just about clear vision but clear understanding too.
From its cause to diagnosis and management, each aspect of PCO is like a facet of a carefully crafted lens, refracting our perception of this post-cataract surgery complication. Through this exploration, we have gained insights into not just its impact on vision but also on the quality of life for our patients.
In the world of ophthalmology, every blink counts, and every detail matters. The persistent endeavor to minimize PCO and improve patient outcomes is an inherent part of our duty, similar to how the posterior capsule itself is an integral part of the visual system. We must continue to refine our surgical techniques, develop better intraocular lens designs, and explore innovative treatments to enhance the lives of our patients.
Research is the vision that guides us towards a better understanding and management of PCO. With promising advancements on the horizon, we stand poised at the threshold of an exciting future in PCO management. Let's keep our eyes on the prize and continue striving towards a future where every post-cataract patient enjoys the clearest of visions, without the shadow of PCO.
As we often say in the business, let's not lose sight of the goal! Or as I prefer to say, let's not lose 'site' of the posterior capsule. Remember, a world in focus is our best prognosis!
(1).jpg)