What is Neuro-Ophthalmology?
Headache, which has existed since the existence of man, is the most common medical complaint and affects more than 80% of the population.
One of the causes of headaches is eye-related problems. Patients complaining of headaches are usually referred to an ophthalmologist by another doctor.
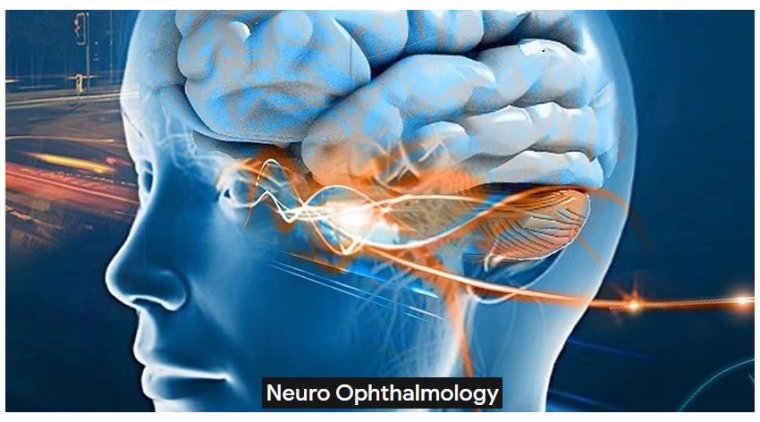
Neuro-ophthalmology is the branch of science that treats headaches caused by eye diseases and deals with common diseases of the eye and nervous system.
Seeing an object is possible when the image is perceived first in the eye and then in the visual center at the back of the brain. Sudden or progressive vision loss can occur when there is a problem with the visual pathways.
In diseases involving eye movements, the main symptom is double vision and the problem may be related to eye muscles, nerves, or control centers in the brain.
Neuro-ophthalmology is a branch of medicine concerned with visual problems related to diseases of the brain rather than diseases of the eyes themselves.
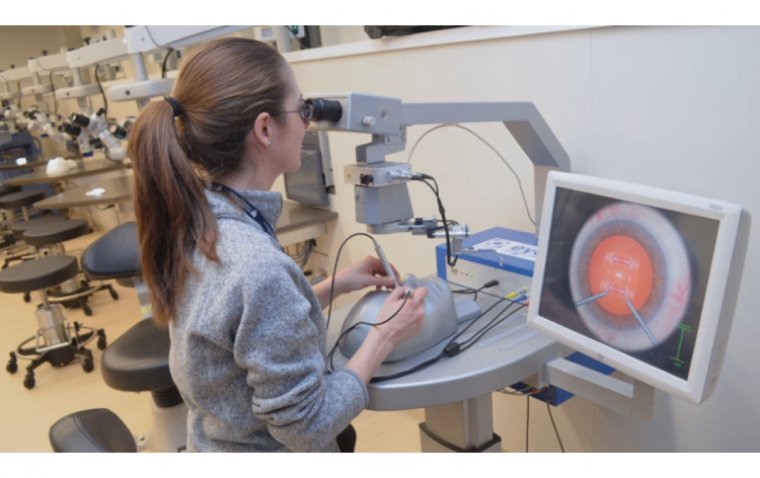
With training in both neurology and neuro-ophthalmology, neuro-ophthalmologists have a unique ability to evaluate patients from both standpoints.
While the eyes are responsible for collecting visual information, it’s the brain that makes sense of the images.
Carrying the messages from the eyes to the brain are the optic nerves, each consisting of more than 1 million nerve fibers. With this complex process comes the potential for a variety of vision problems.
Neuro-ophthalmology, a subspecialty of both neurology and ophthalmology, requires specialized training and expertise in problems of the eye, brain, nerves and muscles.
Neuro-ophthalmologists complete at least 5 years of clinical training after medical school and are usually board certified in Neurology, Ophthalmology, or both.
Neuro-ophthalmologists have unique abilities to evaluate patients from the neurologic, ophthalmologic, and medical standpoints to diagnose and treat a wide variety of problems.
Costly medical testing is often avoided by seeing a neuro-ophthalmologist.
Neuro-ophthalmology is experiencing an exciting growth in diagnostic and treatment options, especially with targeted antibody testing and therapy.
New Therapies & Diagnostics
Tocilizumab (Actemra, Genentech) for giant cell arteritis (GCA). Patients with GCA now have access to the first FDA-approved treatment for the disease.
This is noteworthy because GCA is the most common form of vasculitis affecting adults over age 50, and historically, steroids with all their unfavorable adverse effects have been the only treatment. This drug is a sea change in GCA treatment.
Tocilizumab is an anti–interleukin 6 receptor antibody that reduces B-cell activation, acute phase reactants, and differentiation of T-helper cells.
The approval in May 2017 was based on the results of the GiACTA trial (NCT01791153), in which dosing was weekly or every other week along with a 26-week prednisone taper.
The regimen was superior to steroids alone. Tocilizumab is recommended as both a first-line therapy and second-line therapy in cases with poor high-dose steroid tolerance.
Teprotumumab (Tepezza, Horizon Therapeutics) for thyroid eye disease (TED). Teprotumumab, approved by the FDA in January 2020, is the first therapy for TED.
The drug blocks the insulin-like growth factor (IGF)-1 receptor antibody of the thyroid stimulating hormone receptor/IGF-1 receptor complex and prevents fibroblast stimulation.
Teprotumumab is showing promise in reducing all aspects of thyroid orbitopathy, including optic neuropathy, and not just proptosis, which was the primary outcome measure in the phase 2 and 3 clinical trials.
The results of these promising trials have been released and there are more forthcoming that look at other features of the disease.
Test for anti–myelin oligodendrocyte glycoprotein (MOG) immunoglobulin G (IgG) antibody–associated disease (AD). Physicians faced with patients suspected of having a typical optic neuritis have a new diagnostic tool: the anti-MOG antibody test.
This can be ordered from the Mayo Clinic laboratory and other commercial laboratories and includes neuromyelitis optica (NMO) in the panel.
Some physicians may be concerned about bilateral disease, optic neuritis in the presence of obvious marked disc edema, longitudinal optic nerve enhancement on magnetic resonance images, and/or their pediatric patients.
The test is almost always performed as it can help counsel treatment and prognosis, which is more favorable in the MOGAD group than the NMO group.
Test for aquaporin-4 chloride channel antibody. Physicians have another diagnostic test at their fingertips when NMO is suspected.
Patients may have bilateral severe optic neuropathy with longitudinal optic nerve enhancement, longitudinal cervical spine lesions, relapsing course, or involvement of the optic chiasm and other central nervous system structures such as the area postrema. NMO is more common in women.
The test is available from Mayo Clinic and other commercial laboratories. Importantly, in this very severe disease, steroids are not the treatment choice; plasmapheresis and intravenous immunoglobulin therapies are initiated quickly in patients who have no improvement with steroids after a 5-day course or in whom an NMO diagnosis is immediately suspected based on clinical history.
Oral megadose steroids. When treating patients with typical optic neuritis, these drugs are as efficacious as intravenous steroids. The bioequivalent dose of 1250 mg taken orally is equivalent to 1000 mg administered intravenously.
This treatment is now acceptable based on current findings. This is especially appealing for adherent, insightful patients with no access to an infusion center.
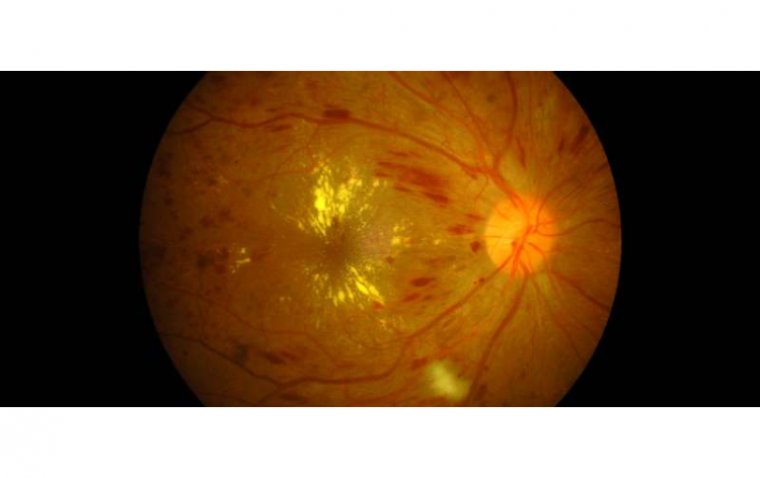
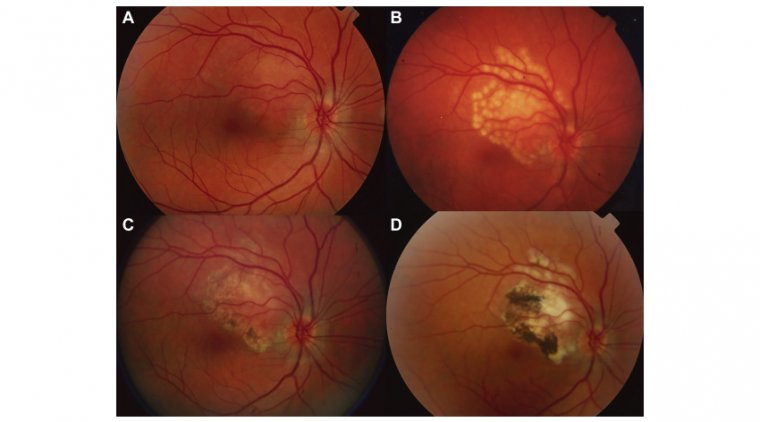
Stroke treatment for branch retinal artery occlusion and central retinal artery occlusion (BRAO, CRAO). The retinal artery occlusions are defined as embolic strokes based on a new classification by the American Heart Association and American Stroke Association.
Patients should be sent to the emergency department for a stroke work-up. Many stroke centers will consider CRAO acute reperfusion therapies, which are being investigated in several ongoing international clinical trials.
It is not just steroids anymore. But when it is, we have more options. Test for MOGAD/NMO on all atypical optic neuritis patients. Remember that new retinal artery occlusions require an acute stroke work-up.
(1).jpg)