Ocular Myasthenia Gravis: Insights into Symptoms, Diagnosis, and Treatment
In the fascinating realm of medicine, where every condition has its unique story, Ocular Myasthenia Gravis (OMG) spins a captivating narrative of its own. As a mysterious subset of the broader Myasthenia Gravis family, OMG often lurks behind the curtains of confusing symptoms, complicating the plot with its mercurial nature and elusive diagnosis. In this unfolding drama, the protagonist is the human eye, displaying an intriguing performance through symptoms like ptosis and diplopia. Yet, to comprehend the full script of OMG, we must step beyond the proscenium arch of the eye and venture into the auditorium of autoimmune disorders.
This comprehensive exploration takes you on a journey, highlighting the causes, symptoms, diagnostic strategies, and management options for this complex condition. Our exploration seeks to provide clarity to healthcare providers and offer solace to those navigating the bewildering maze of OMG, hoping to turn the spotlight on a path towards better understanding and effective management.
What Are the Symptoms of Ocular Myasthenia Gravis?
Ocular Myasthenia Gravis (OMG) presents itself through a series of symptoms that act as the red flags pointing towards this neurological condition. These symptoms play a vital role in identifying the condition and determining the course of treatment. Here, we delve deeper into the symptoms of OMG, which are categorized as follows:
1. Eye-related Symptoms
The inaugural signs of OMG usually involve the eyes. The two most notable symptoms are:
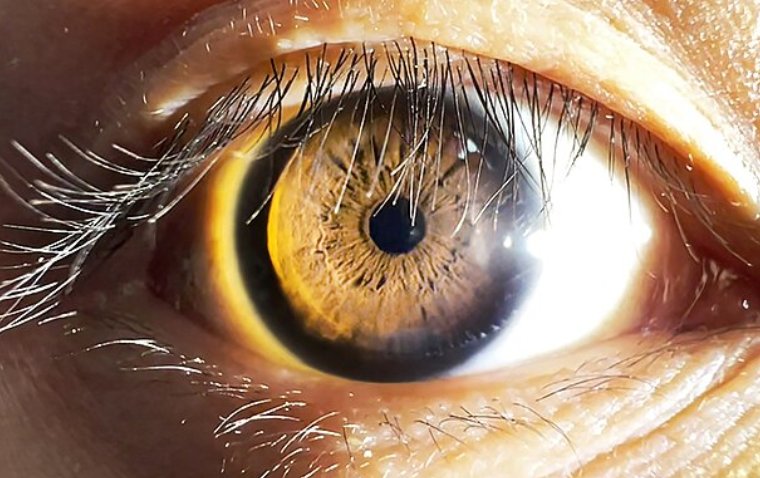
● Ptosis: This is marked by a unilateral or bilateral drooping of the eyelids. Ptosis can create a tired or sleepy appearance and, in severe cases, can even obstruct vision.
● Diplopia: More commonly known as double vision, this condition can cause a person to see two images of a single object. Diplopia can occur either horizontally or vertically and usually affects both eyes.
2. Fluctuating Severity of Symptoms
A distinctive feature of OMG is the variability in the intensity of symptoms. Patients might notice:
● An increase in symptom severity during periods of physical exertion or emotional stress, and a decrease during rest.
● A variability in the manifestation of symptoms that may fluctuate over the course of a day, or even from one day to the next.
3. Beyond Ocular Involvement
While the name suggests a limitation to the eyes, the story of OMG often extends its chapters beyond the ocular realm. There may be associated symptoms such as:
● Dysphagia: This symptom is characterized by difficulty swallowing, which might progress to the extent of preventing adequate nutrition.
● Changes in Facial Expression: Patients may experience difficulty in smiling, frowning, or other facial expressions due to muscle weakness.
● Limb Weakness: In rare cases, OMG may affect the muscles in the limbs, causing a generalized sense of weakness and fatigue.
How to Diagnose Ocular Myasthenia Gravis
Navigating the intricate maze of Ocular Myasthenia Gravis (OMG) is a process that involves careful examination, shrewd evaluation, and application of precise diagnostic tools. Here's a look at how the process of diagnosing OMG unfolds:
1. Evaluation of Symptoms, Clinical Examination, and Medical History
The first and most critical step in diagnosing OMG involves a detailed assessment of symptoms, coupled with an exhaustive clinical examination. The fluctuating nature of ptosis and diplopia, hallmark signs of OMG, can often provide clinicians with their initial clue. Additionally, an extensive review of the patient's medical history, including any known autoimmune disorders, contributes significantly to the diagnostic process.
2. Diagnostic Tests
Following the preliminary examination, the physician may recommend specific tests that help confirm the diagnosis. These tests include:
● Acetylcholine Receptor Antibody Testing: This blood test looks for the presence of antibodies against the acetylcholine receptors at the neuromuscular junction. An elevated level of these antibodies can point towards a diagnosis of OMG.
● Repetitive Nerve Stimulation: This electrodiagnostic test measures the electrical activity of muscles and nerves and can reveal a characteristic pattern of muscle response often seen in patients with OMG.
3. Differential Diagnosis
It's essential to distinguish OMG from other ocular disorders that might present with similar symptoms, such as orbital myositis, Graves' ophthalmopathy, and cranial nerve palsies. Moreover, it's equally crucial to differentiate OMG from generalized Myasthenia Gravis (MG). While the symptoms of OMG are limited to the eye muscles, MG affects muscles throughout the body. Differentiating between these conditions can help guide appropriate treatment strategies and anticipate possible disease progression.
Management and Treatment Options
Mapping out the journey to manage and treat Ocular Myasthenia Gravis (OMG) involves a strategic blend of various therapeutic options. Here, we delve into the multifaceted approach to managing this condition:
1. Overview of Available Treatment Approaches
The treatment strategy for OMG is two-pronged, involving both pharmacological and non-pharmacological interventions. The pharmacological measures focus on reducing the symptoms and preventing the progression of the disease, while non-pharmacological strategies aim to manage the impact of symptoms on patients' daily lives. These may involve physical therapy, lifestyle modifications, and eye care routines.
2. Role of Acetylcholinesterase Inhibitors and Immunosuppressive Therapies
Medications play a crucial role in managing OMG. The frontline treatment often involves the use of acetylcholinesterase inhibitors such as pyridostigmine, which boost the levels of acetylcholine at the neuromuscular junction, enhancing muscle strength. In cases where acetylcholinesterase inhibitors are insufficient or when symptoms are severe, immunosuppressive drugs such as corticosteroids or azathioprine may be employed. These medications help reduce the immune system's attack on the body's own tissues, thereby alleviating symptoms.
3. Potential Benefits and Risks of Treatments in OMG
While the benefits of these treatments include improved muscle strength and reduction in symptom severity, they also come with potential risks. Side effects may include digestive problems, susceptibility to infections, bone loss, and mood changes, among others. Hence, it's crucial that patients are thoroughly educated about these possibilities before embarking on their treatment journey.
4. Importance of Individualized Treatment Plans and Regular Follow-Up
As with any condition, there's no 'one-size-fits-all' treatment for OMG. Management must be tailored to the individual's symptoms, overall health, lifestyle, and personal preferences. Regular follow-ups with healthcare providers ensure that the treatment plan remains effective and adaptable to the patient's changing condition. These visits also provide an opportunity to monitor for potential side effects and make adjustments as needed.
To Conclude…
In the grand theatre of the human body, Ocular Myasthenia Gravis (OMG) plays a challenging role. Its enigmatic symptoms, marked by fluctuating eye-related issues such as ptosis and diplopia, often extend their influence beyond the ocular realm. Unmasking this elusive character demands an in-depth evaluation of symptoms, rigorous clinical examination, detailed medical history, and precise diagnostic tests. Yet, distinguishing it from other ocular disorders and generalized Myasthenia Gravis forms a crucial aspect of the diagnosis, guiding the path to targeted treatment.
The spotlight on the management of OMG illuminates a blend of pharmacological and non-pharmacological strategies, underscoring the roles of acetylcholinesterase inhibitors and immunosuppressive therapies. These therapies, while bringing potential benefits, also tread the tightrope of risks. Thus, the journey of managing OMG involves the crafting of individualized treatment plans and the necessity of regular follow-ups. Like all grand narratives, the story of OMG is an evolving one, demanding continuous learning, understanding, and adapting to ensure that every patient finds their path to the best possible care.
(1).jpg)