Transscleral Cyclophotocoagulation: An Alternative to Traditional Glaucoma Surgery
What Is Transscleral Cyclophotocoagulation?
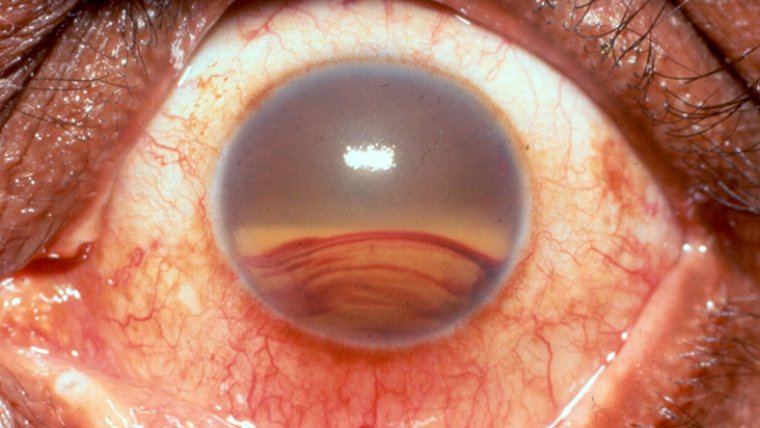
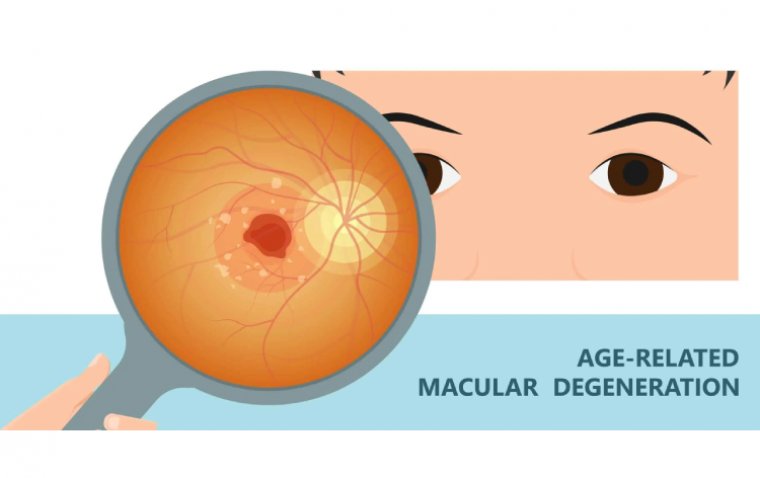
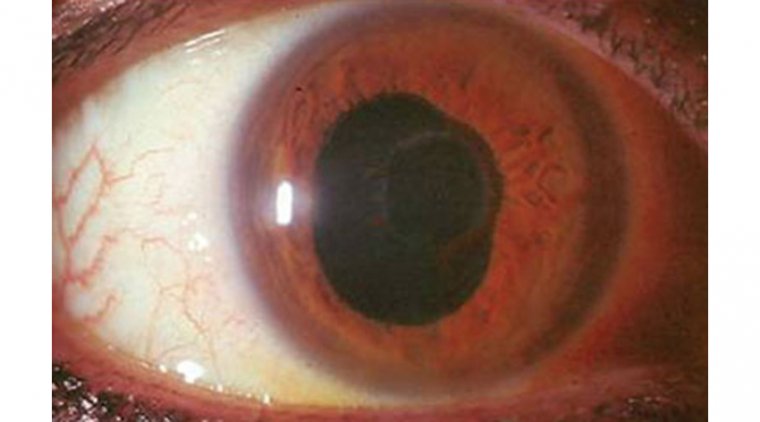
Transscleral Cyclophotocoagulation (TCP) is a minimally invasive surgical procedure used to treat glaucoma, a group of eye diseases that cause damage to the optic nerve resulting in vision loss. It is an alternative to traditional glaucoma surgeries that involve creating a new drainage channel to lower the eye's intraocular pressure (IOP). Instead, TCP uses laser energy to reduce the production of aqueous humour, the fluid that fills the anterior chamber of the eye and lowers the IOP.
TCP is typically performed on patients who have not responded to other forms of glaucoma treatment, such as eye drops, oral medications, or laser trabeculoplasty. It is also an option for patients who are unsuitable candidates for traditional glaucoma surgeries due to their age or health status. TCP can be performed in an outpatient setting and does not require general anaesthesia.
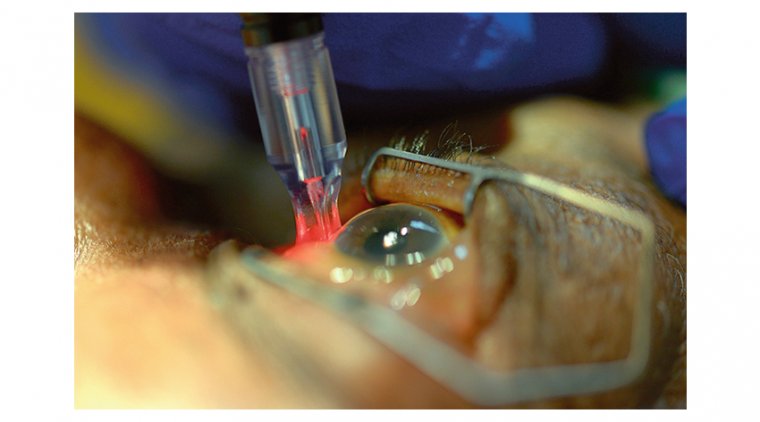
How Is Transscleral Cyclophotocoagulation Performed?
1. Anesthesia: The patient is given local anaesthesia with numbing drops to the eye.
2. Incision: A small incision is made in the conjunctiva, the thin membrane covering the eye's white part.
3. Probe insertion: The surgeon inserts a specially designed probe through the incision to deliver laser energy to the ciliary body, the part of the eye that produces aqueous humour.
4. Laser application: Laser energy destroys the ciliary body tissue, reducing the production of aqueous humour and lowering the intraocular pressure (IOP).
5. Monitoring: The surgeon monitors the patient's eye pressure during the procedure to ensure that the desired IOP reduction is achieved.
6. Closure: The incision in the conjunctiva is closed with stitches or glue.
7. Postoperative care: The patient may be prescribed eye drops and oral pain medication to manage postoperative symptoms such as discomfort and redness in the eye. They may also be advised to avoid strenuous activity and use protective eyewear during healing.
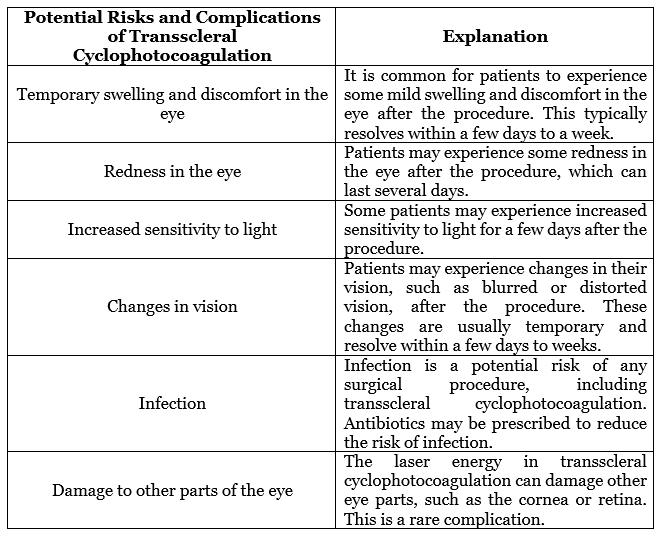
What Are The Potential Risks And Complications Of Transscleral Cyclophotocoagulation?
How Effective Is Transscleral Cyclophotocoagulation in Reducing Intraocular Pressure?
Transscleral cyclophotocoagulation (TCP) effectively reduces intraocular pressure (IOP) in patients with glaucoma. The exact reduction in IOP can vary depending on the patient's case and the severity of their glaucoma.
Several studies have evaluated the effectiveness of TCP in reducing IOP. A study published in the Journal of Glaucoma found that TCP reduced IOP by an average of 30% in patients with primary open-angle glaucoma. Another study published in the Journal of Ophthalmology found that TCP reduced IOP by an average of 31% in patients with refractory glaucoma who had previously undergone other forms of treatment.
In addition to reducing IOP, TCP has decreased the need for additional glaucoma treatments, such as eye drops or other surgeries. A study published in the Journal of Glaucoma found that TCP reduced the need for additional treatments by 38% in patients with primary open-angle glaucoma.
How Long Does It Take To See the Results of Transscleral Cyclophotocoagulation?
The time it takes to see the results of transscleral cyclophotocoagulation (TCP) can vary depending on the individual patient and the severity of their glaucoma.
In some cases, patients may experience a reduction in intraocular pressure (IOP) within a few days of the procedure. However, it may take several weeks for the full effect of TCP.
During this time, patients may continue to take glaucoma medications as directed by their ophthalmologist. It is essential to continue taking medications until instructed otherwise by a healthcare provider. Suddenly stopping medication can lead to a rapid increase in IOP and potentially further vision loss.
Patients should have regular follow-up appointments with their ophthalmologist after the procedure to monitor their IOP and ensure they achieve the desired results. In some cases, additional TCP procedures or other forms of glaucoma treatment may be necessary to achieve optimal IOP control.
Can Transscleral Cyclophotocoagulation Be Repeated?
Yes, transscleral cyclophotocoagulation (TCP) can be repeated to maintain the desired reduction in intraocular pressure (IOP). The decision to repeat the procedure will depend on the individual patient's response to the initial procedure and the severity of their glaucoma.
In some cases, the initial TCP procedure may not achieve the desired reduction in IOP, or the effects may wear off over time. In these cases, a repeat TCP procedure may be recommended to reduce IOP further and prevent further vision loss.
It is important to note that repeat TCP procedures may carry an increased risk of complications, such as scarring of the eye tissue or damage to the optic nerve. Patients considering a repeat TCP procedure should discuss the potential risks and benefits with their ophthalmologist.
In addition, to repeat TCP procedures, other forms of glaucoma treatment may be necessary to maintain IOP control. This may include eye drops, oral medications, or other types of surgery.
Is Transscleral Cyclophotocoagulation a Permanent Solution For Glaucoma?
Transscleral cyclophotocoagulation (TCP) is not a permanent solution for glaucoma, but it can provide a long-lasting reduction in intraocular pressure (IOP) for many patients. The duration of the IOP-lowering effects of TCP can vary depending on the individual patient and the severity of their glaucoma.
In some cases, the effects of TCP may last for several years. However, the effects may wear off over time, and additional glaucoma treatments may be necessary to maintain IOP control.
Despite not being a permanent solution, TCP is a safe and effective treatment option for patients with glaucoma who have not responded to other forms of treatment. It is minimally invasive and does not require general anaesthesia, making it a suitable option for many patients.
Conclusion
In conclusion, transscleral cyclophotocoagulation (TCP) is a safe and effective option for patients with glaucoma who have not responded to other forms of treatment. This minimally invasive procedure uses laser energy to reduce the production of aqueous humour and lower intraocular pressure, providing long-lasting relief for many patients.
While TCP may not be a permanent solution for glaucoma, it can provide significant benefits and reduce the need for additional glaucoma treatments. Patients considering TCP should discuss the potential risks and benefits of the procedure with their ophthalmologist to determine if it is the right option for their case. With advances in technology and medical knowledge, treatments for glaucoma are continually improving, providing hope for improved vision and quality of life for those living with this condition.
Author: Dr. Muhammad Saad, Resident Ophthalmologist at AlShifa Trust Eye Hospital in Rawalpindi,Pakistan
(1).jpg)