What is Suprachoroidal Hemorrhage
What Is Suprachoroidal Hemorrhage?
Suprachoroidal hemorrhage is a sight-destroying pathology. It arises when there is a rupture of long or short ciliary arteries during an intraocular surgery and blood is contained in the space between the choroid and the sclera.
SCH can be classified according to the size and extent of bleeding, its association with intraocular surgery (whether the hemorrhage is intraoperative or postoperative), and aggravating factors like spontaneous bleeding, penetrating trauma, or perioperative).
What Causes Suprachoroidal Hemorrhage?
Multiple risk factors and causes are recognized to be connected with SCH, like senescence, regular use of certain medications such as an anticoagulant or antiplatelet drugs, history of a hypertensive, non-compliant patient, history of atherosclerosis or diabetes Mellitus in a patient.
Ocular Risks
Ocular risks are identified mostly during the history taking process, for instance, a history of ocular pathologies like glaucoma, high myopia, aphakia, ocular trauma, intraocular surgery or previous SCH are suggestive of SCH. Other than that, raised intraocular pressure before the surgery and Choroidal hemangioma substantially increase the chances of SCH.
During or post-surgery several reasons contribute to SCH are acute drop in IOP, general anesthesia or retrobulbar anesthesia, Valsalva-type maneuvers, complicated eye surgery, or vitreous loss during cataract surgery.
Signs and Symptoms of Suprachoroidal Hemorrhage
● Extreme ocular pain and discomfort
● Headache and nausea with or without vomiting (deteriorating on Valsalva maneuvers)
● Diminished visual acuity
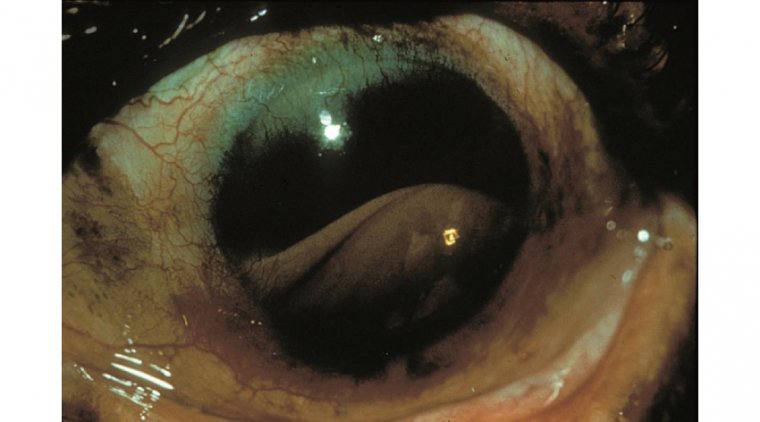
● Shallow Anterior chamber
● Absent Red Reflex
● High IOP
● Vitreous prolapse into the anterior chamber
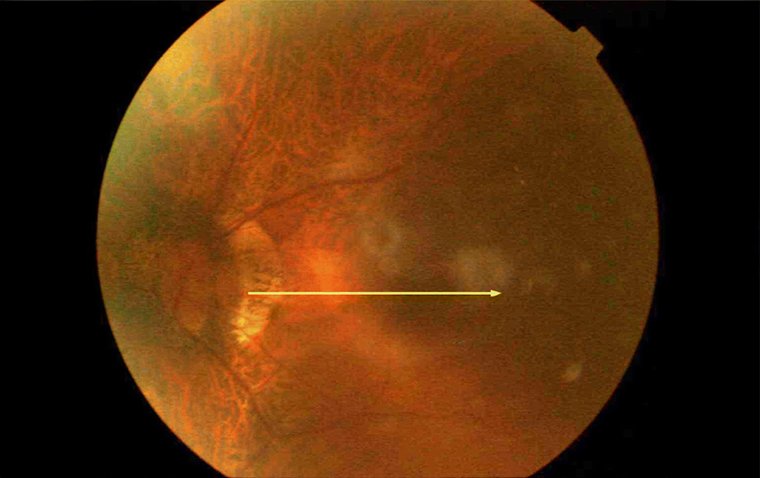
● Choroidal elevation
● Wrinkling and bulging of the posterior capsule
● Bulge of intraocular contents as an example iris or vitreous prolapse
How Is It Diagnosed?
History
There are numerous features from the patient's medical and ocular history suggestive of SCH. SCH can be diagnosed clinically based on the history, signs, and symptoms of the patient backed by clinical examination and ocular tests done on a patient by the ophthalmologist. Multimodal imaging techniques to identify SCH correctly are as under: -
● Optical coherence tomography (OCT)
● Computed tomography (CT) and Magnetic resonance imaging (MRI)
● FA and ICG (to exclude other causes)
● Ultrasonography (B scan and A scan) to determine the site and degree of the bleeding and the condition of the retina and vitreous.
How to Manage Suprachoroidal Hemorrhage?
If an intraoperative SCH is assumed, it is crucial to stop further hemorrhage and the expulsion of intraocular contents. This is achieved by instantaneous tamponade of bleeding vessels (directly applying pressure on the bleeding site or closure of all incisions). In case of ocular contents ousting, they need to be restored to their original anatomy promptly. If that is not possible then drainage of uncoagulated blood is obligatory to relax the pressure created in the eye.
After this, the anterior chamber is maintained vitreous with the viscoelastic agent or air. For SCH with RD, vitreoretinal traction, or vitreous hemorrhage the drainage procedure as well as vitrectomy or scleral buckling is done.
Your ophthalmologist may prescribe some medications in accordance with your symptoms like topical steroids to lessen ocular inflammation, topical cycloplegics like atropine, or oral analgesics for ocular pain. topical beta blockers to control IOP. Aspirin and NSAIDs are contraindicated as the antiplatelet property may exacerbate the hemorrhage.
(1).jpg)