Eyes Irritated? It Could Be Squamous Blepharitis
What Is Squamous Blepharitis?
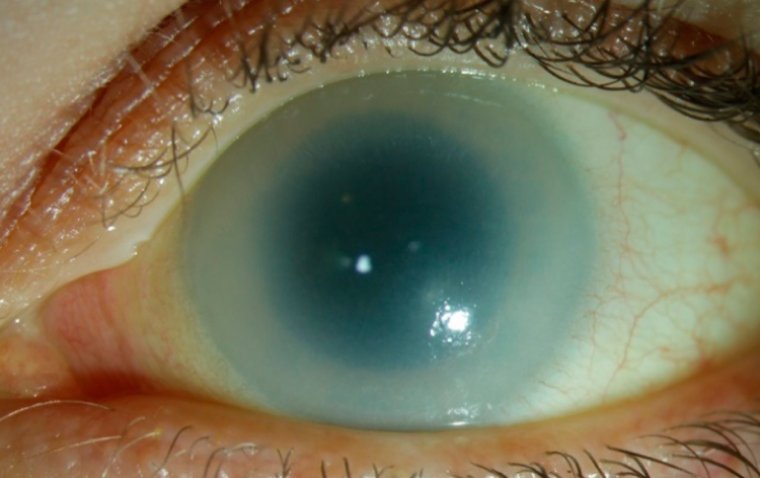
Squamous blepharitis is a condition characterized by inflammation of the eyelids, specifically affecting the squamous or outermost layer of the eyelid margin. This condition can have a significant impact on eye health, causing symptoms such as redness, itching, and irritation of the eyes.
Types of Squamous Blepharitis
Squamous blepharitis can be either acute or chronic, depending on the underlying causes and the course of the condition. Here's a breakdown of both:
1. Acute Squamous Blepharitis: Acute episodes of squamous blepharitis are characterized by sudden and severe symptoms. These episodes can be triggered by factors like infections, allergies, or environmental irritants. The symptoms of acute squamous blepharitis may include intense redness, swelling, crusting, and discomfort of the eyelids. While these symptoms can be quite bothersome, they often respond well to prompt treatment, such as antibiotics or anti-inflammatory medications.
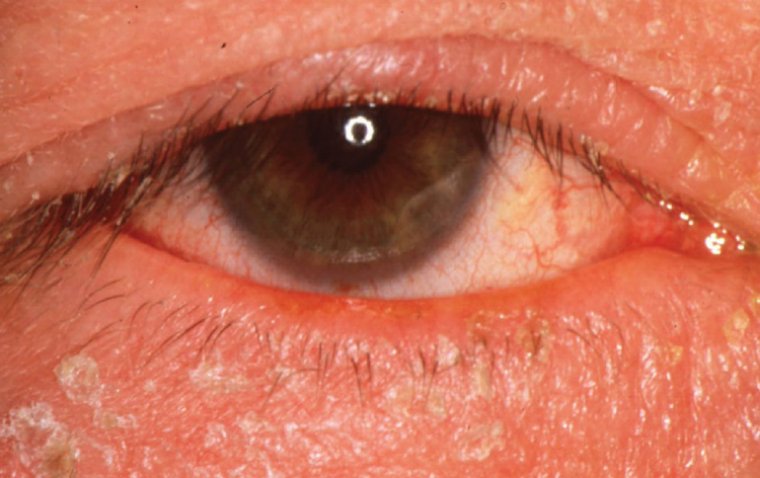
2. Chronic Squamous Blepharitis: Chronic squamous blepharitis is characterized by persistent and recurrent symptoms that can last for an extended period, often months or even years. This form of blepharitis is typically associated with underlying conditions like seborrheic dermatitis, rosacea, or meibomian gland dysfunction. Common symptoms include mild redness, flakiness, and irritation of the eyelids. Chronic blepharitis tends to require ongoing management, including regular eyelid hygiene, lubricating eye drops, and, in some cases, prescription medications.
Ulcerative vs Squamous Blepharitis
Ulcerative blepharitis and squamous blepharitis are two distinct subtypes of blepharitis, each with its own characteristics and underlying causes.
Ulcerative blepharitis is characterized by the presence of tiny sores or ulcers along the eyelid margins. These ulcers may cause discomfort, crusting, and matting of the eyelashes. The most common cause of ulcerative blepharitis is bacterial, often due to an overgrowth of Staphylococcus bacteria.
On the other hand, squamous blepharitis primarily affects the squamous or outermost layer of the eyelid margin. It is characterized by flaky, scaly, or waxy debris along the eyelashes and eyelid margin. While bacterial involvement can also play a role in squamous blepharitis, it is often associated with other conditions like seborrheic dermatitis or dry eye syndrome.
What Causes Squamous Blepharitis?
Squamous blepharitis can have various underlying causes, often related to factors affecting the outermost layer of the eyelid margin. Here are some common causes and contributing factors:
1. Poor Eyelid Hygiene: One of the primary causes of squamous blepharitis is inadequate eyelid hygiene. Failure to clean the eyelid margins properly can lead to the accumulation of debris, oils, and dead skin cells, creating an environment conducive to the growth of bacteria and fungi.
2. Seborrheic Dermatitis: This is a skin condition that can affect the eyelids and is characterized by flaky, oily, and red skin. It's often linked to squamous blepharitis, as the excessive oil production can contribute to the buildup of debris along the eyelid margin.
3. Dry Eye Syndrome: Individuals with dry eye syndrome may experience squamous blepharitis due to insufficient tear production. Tears help maintain the health of the eyelid margin, and their absence can lead to irritation and flaking.
4. Allergies: Allergic reactions to substances like pollen, dust mites, or pet dander can cause inflammation along the eyelid margin, leading to squamous blepharitis.
5. Bacterial or Fungal Infections: While squamous blepharitis is primarily associated with issues related to the squamous layer of the eyelid, it can also involve bacterial or fungal infections in some cases.
6. Systemic Conditions: Certain systemic conditions, such as rosacea and psoriasis, can increase the risk of developing squamous blepharitis.
7. Medications: Some medications, like isotretinoin (used to treat acne), can lead to changes in the meibomian glands and increase the risk of blepharitis.
Symptoms of Squamous Blepharitis
Squamous blepharitis can manifest through a range of uncomfortable and noticeable symptoms. These symptoms may vary in intensity and can include:
● Redness: Redness of the eyelid margins is a common symptom of squamous blepharitis. It occurs due to inflammation in the area.
● Flaky or Scaly Skin: Individuals with squamous blepharitis often experience flaky or scaly skin along the edges of the eyelids. This can lead to a feeling of itchiness or irritation.
● Crust Formation: The accumulation of debris, oils, and skin cells along the eyelid margin can result in the formation of crusts or scales. These may appear especially noticeable in the morning after waking up.
● Eyelash Problems: Squamous blepharitis can affect the health of eyelashes. They may become misaligned or even fall out due to the inflammation and irritation.
● Burning or Stinging Sensation: Some individuals with squamous blepharitis report a burning or stinging sensation, particularly along the eyelid margins.
● Excessive Tearing or Dry Eyes: Paradoxically, squamous blepharitis can lead to both excessive tearing and dry eyes. The inflammation along the eyelid margin can disrupt the normal functioning of the meibomian glands, affecting tear composition and distribution.
● Photophobia: Sensitivity to light, known as photophobia, can be a symptom of squamous blepharitis. The eye's increased sensitivity may cause discomfort in bright or sunny conditions.
● Blurry Vision: In some cases, squamous blepharitis can lead to blurry or fluctuating vision, especially if it affects the tear film's stability.
Diagnosis and Assessment of Squamous Blepharitis
Diagnosing and assessing squamous blepharitis typically involves a comprehensive evaluation by an eye care professional, such as an ophthalmologist or optometrist. The process may include the following components:
Medical History: The eye care provider will begin by taking a detailed medical history. They will inquire about any symptoms you are experiencing, the duration of these symptoms, and any relevant medical conditions, allergies, or medications you are currently taking.
External Examination: The eye care professional will perform an external examination of your eyes and eyelids. They will visually inspect the eyelid margins for signs of inflammation, redness, flakiness, and crusting.
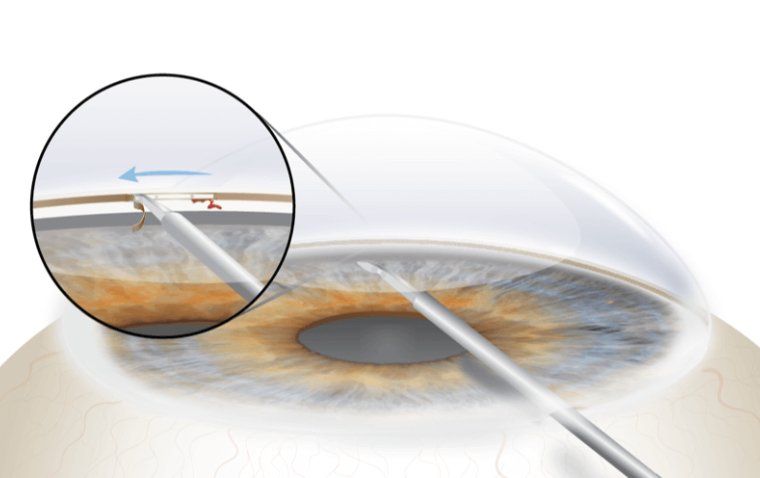
Slit-Lamp Examination: A slit-lamp biomicroscope is a specialized instrument that allows for a magnified and well-illuminated view of the eye's structures. Your eye care provider may use this to closely examine the eyelid margins, eyelashes, and the anterior surface of the eye.
Tear Film Assessment: The tear film is crucial for maintaining ocular health. Your provider may assess the quality and quantity of your tears, which can be affected by squamous blepharitis. Special dyes may be used to evaluate tear distribution and stability.
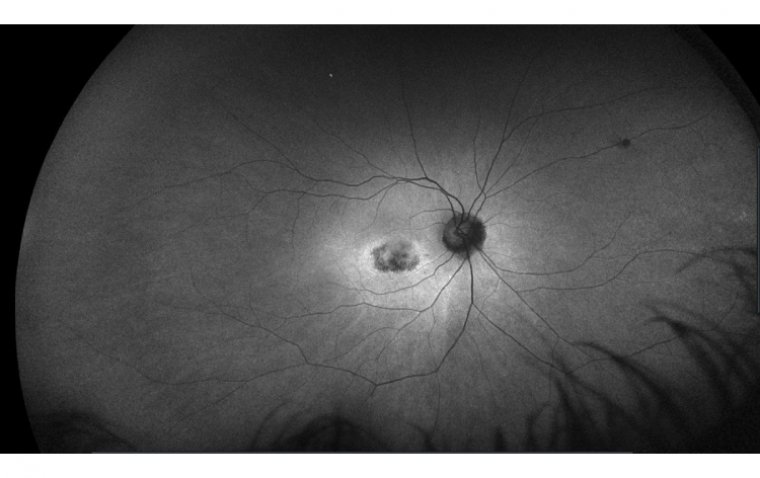
Meibomian Gland Assessment: These are the glands in your eyelids responsible for producing the oily component of tears. Dysfunction of the meibomian glands is common in blepharitis. Your ophthalmologist may evaluate the health and function of these glands.
Microbial Cultures: In some cases, your eye care provider may collect samples from the eyelid margin to identify any underlying bacterial or fungal infections.
Specialized Tests: Depending on the severity and extent of the condition, additional tests such as corneal staining or meibography (imaging of meibomian glands) may be performed.
Assessment of Visual Acuity: If squamous blepharitis has affected your vision, your ophthalmologist will assess your visual acuity to determine the impact and whether corrective measures are needed.
How Is Squamous Blepharitis Treated?
The treatment of squamous blepharitis typically involves a combination of home care practices and, in some cases, prescribed medications. Here are the key treatment methods:
1. Eyelid Hygiene: Proper eyelid hygiene is a fundamental aspect of managing squamous blepharitis. This involves gently cleaning the eyelids and eyelashes to remove accumulated debris and crusts. The following steps are often recommended:
● Apply a warm compress to the closed eyelids for about 5-10 minutes to soften crusts and loosen debris.
● Use a clean, warm washcloth or a commercially available lid scrub solution to clean the eyelids. Gently scrub along the eyelid margins, focusing on the base of the eyelashes.
● Rinse the eyelids thoroughly with warm water and pat them dry with a clean towel.
2. Topical Antibiotics or Steroids: In cases of squamous blepharitis associated with bacterial infections or significant inflammation, your eye care provider may prescribe topical antibiotics or steroids. These medications can help reduce inflammation and control infection.
3. Artificial Tears: Lubricating eye drops, known as artificial tears or tear substitutes, can alleviate dryness and discomfort associated with squamous blepharitis. They help maintain a healthy tear film and reduce irritation.
4. Oral Medications: In some instances, especially when squamous blepharitis is linked to underlying medical conditions like rosacea or seborrheic dermatitis, your healthcare provider may recommend oral medications like antibiotics or anti-inflammatory drugs.
5. Management of Underlying Conditions: Treating any associated medical conditions, such as rosacea or dandruff, is essential. Controlling these underlying conditions can help alleviate blepharitis symptoms.
6. Eyelid Scrubs and Cleansers: Your eye care provider may recommend specific eyelid scrubs or cleansers designed to maintain eyelid hygiene. These products are available over-the-counter or as prescription-strength solutions.
7. Follow-Up Care: Regular follow-up appointments with your eye care provider are crucial to monitor your progress and adjust the treatment plan as needed. They can also evaluate the effectiveness of the prescribed medications and suggest modifications if required.
8. Lifestyle Modifications: Lifestyle changes can be helpful in managing squamous blepharitis. These include:
● Avoiding eye makeup during active episodes of blepharitis.
● Using hypoallergenic or non-comedogenic cosmetics if makeup is necessary.
● Practicing good hand hygiene to prevent the spread of bacteria.
● Maintaining a balanced diet rich in omega-3 fatty acids, which may have anti-inflammatory effects on the eyes.
Is Squamous Blepharitis Contagious?
Squamous blepharitis itself is not contagious. It is not caused by a viral or bacterial infection that can be transmitted from person to person through direct contact. Instead, squamous blepharitis is typically associated with underlying factors such as poor eyelid hygiene, meibomian gland dysfunction, or skin conditions like seborrheic dermatitis or rosacea.
However, it's essential to note that some conditions that can contribute to or accompany squamous blepharitis, such as staphylococcal infections of the skin or conjunctivitis (pink eye), can be contagious. In these cases, the contagious element is the underlying infection rather than the blepharitis itself.
While squamous blepharitis is not directly contagious, good hygiene practices are crucial to prevent its exacerbation and to reduce the risk of developing secondary infections or complications. This includes regular eyelid hygiene, avoiding sharing personal items related to eye care, and practicing proper handwashing to minimize the risk of introducing harmful microorganisms to the eye area. If you suspect any contagious eye condition or have concerns about eye health, it's advisable to consult with an eye care professional for a proper evaluation and guidance on preventive measures.
Summary
Squamous blepharitis is a non-contagious eye condition characterized by inflammation of the eyelid margins. It can cause symptoms like redness, flaky skin, and eye discomfort. While it's not directly contagious, some underlying conditions that contribute to it, such as skin infections, can be contagious. Squamous blepharitis is typically chronic and requires ongoing management, which may include warm compresses and prescribed topical treatments. Good eyelid hygiene is essential to prevent its exacerbation. If you suspect squamous blepharitis or have concerns about your eye health, consult with an eye care professional for proper evaluation and guidance.
(1).jpg)