Keratoprosthesis: A Comprehensive Guide to Artificial Cornea Implants
What Is Keratoprosthesis?
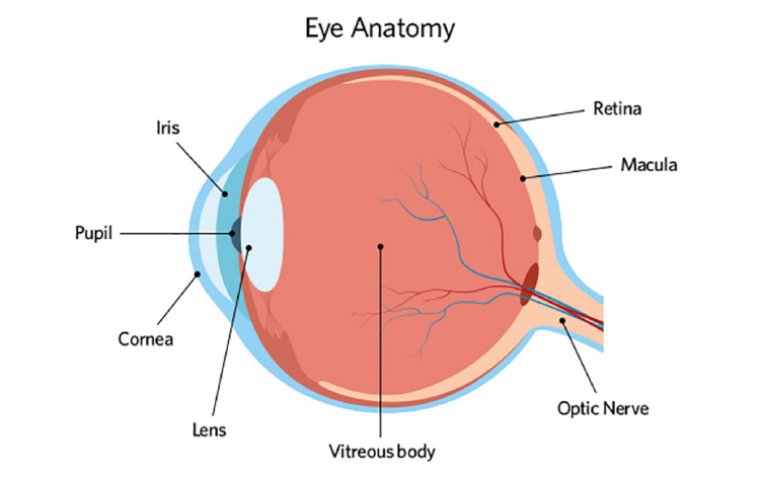
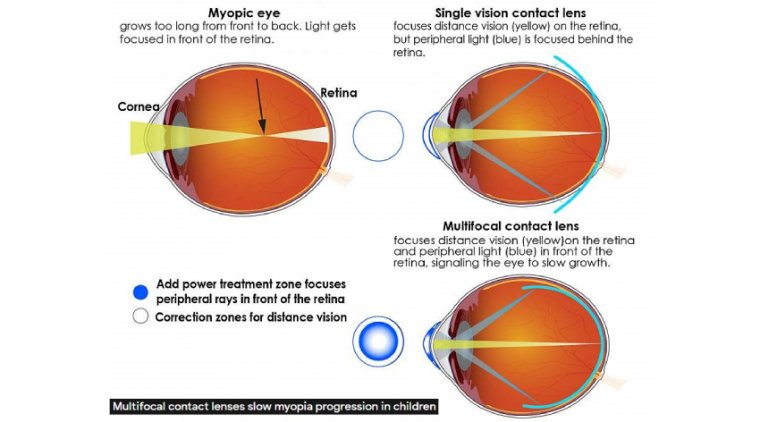
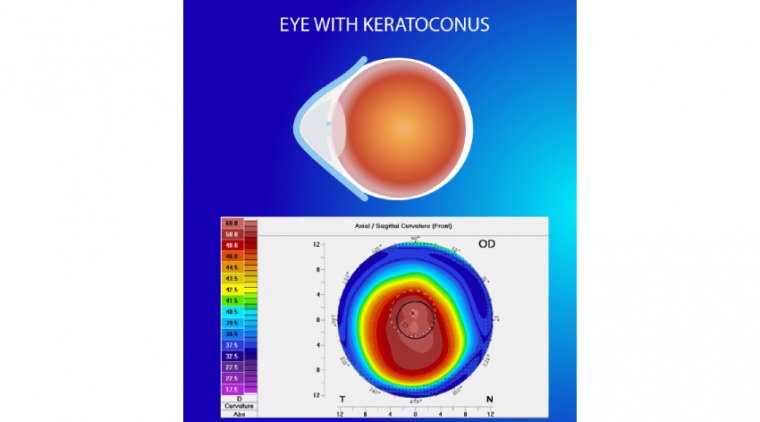
Keratoprosthesis refers to an innovative surgical procedure designed to restore vision in individuals suffering from severe corneal disease or damage. The term 'keratoprosthesis' is derived from the Greek words 'kerato,' meaning cornea, and 'prosthesis,' meaning artificial addition. The cornea, being the eye's outermost layer, plays a critical role in focusing light onto the retina, a process essential for clear vision. However, diseases or damage to the cornea can significantly impair visual acuity.
Historically, corneal transplant from a human donor was the go-to solution for severe corneal conditions. However, for patients with a high risk of transplant failure, this option may be limited. This is where keratoprosthesis, involving the implantation of an artificial cornea, comes into play. It offers a ray of hope for these individuals, opening new avenues for vision restoration. In the sections that follow, we look further into the world of keratoprosthesis, highlighting the types of artificial cornea implants, surgical techniques, and crucial postoperative care.
Types of Keratoprosthesis
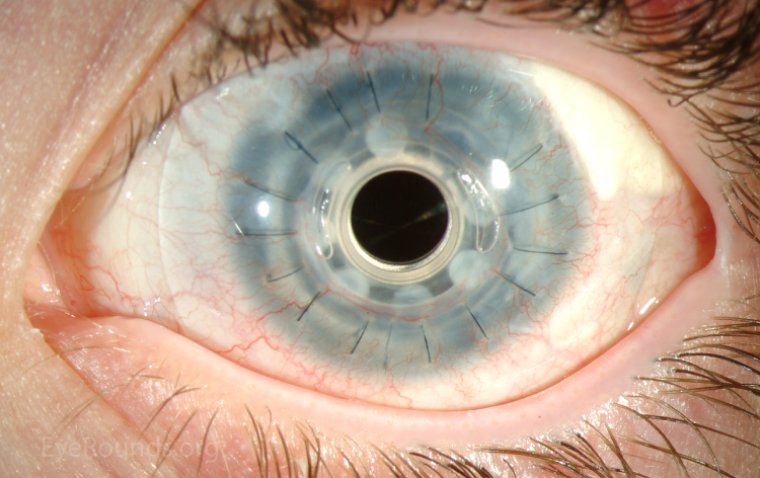
There are several types of artificial cornea implants available. The Boston Keratoprosthesis (BKPro), for instance, is one of the most widely used types. It's made of clear plastic with excellent tissue compatibility and durability. Another type is AlphaCor, a soft, flexible, and biocompatible synthetic cornea designed to integrate well with surrounding eye tissues.
The primary role of these artificial corneas is to restore the eye's ability to focus light onto the retina, thereby improving visual acuity. They are designed to mimic the natural cornea's refractive properties, making them effective in restoring vision.
The eligibility for keratoprosthesis varies depending on the individual's specific condition and overall health. It's generally considered for patients with repeated graft failure, severe ocular surface disease, or those with conditions that put them at high risk for graft rejection. The decision is made in consultation with an ophthalmologist who considers various factors, including the potential for vision improvement and the patient's ability to follow postoperative care.
Surgical Procedure and Techniques
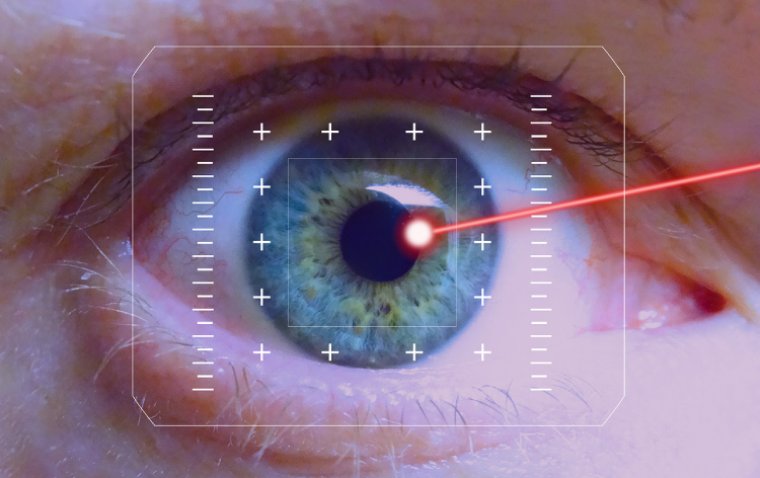
The procedure for keratoprosthesis implantation is performed under general or local anesthesia, with the specifics varying depending on the type of artificial cornea being used and the patient's overall eye health.
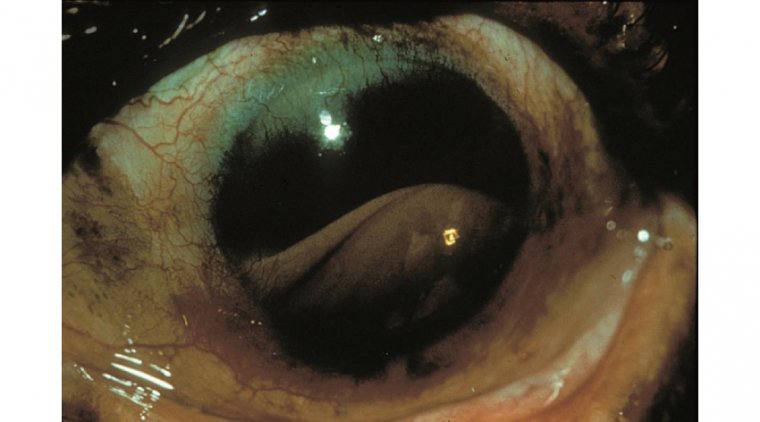
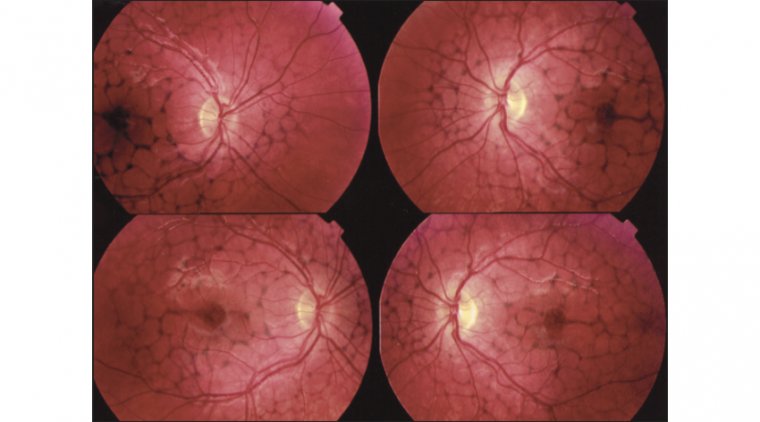
Prior to surgery, a thorough preoperative assessment is essential to evaluate the eye's health, including the status of the retina and optic nerve, and to ensure there are no contraindications to surgery. Other critical factors such as the patient's general health, potential for visual rehabilitation, and capacity for long-term follow-up are also considered.
In general, the surgery involves the removal of the central portion of the damaged or diseased cornea. The artificial cornea is then carefully positioned and secured in place. This can be done using various surgical techniques.
In a full-thickness keratoprosthesis procedure, the entire cornea is replaced with the artificial implant. In contrast, a lamellar keratoprosthesis procedure involves replacing only a portion of the cornea, preserving some of the patient's own corneal tissue.
A critical factor in the success of keratoprosthesis surgery is the experience of the surgeon and the support of a multidisciplinary team, including corneal specialists, glaucoma experts, and ocular surface disease specialists. This team-based approach ensures comprehensive care before, during, and after surgery.
Recent advancements in surgical techniques and artificial cornea design are continually improving outcomes for keratoprosthesis patients. For instance, the development of newer models of the Boston Keratoprosthesis has significantly improved biocompatibility and patient comfort. The continual refinement of surgical techniques and postoperative care has also reduced complications and enhanced visual outcomes, offering new hope for individuals with severe corneal disease.
.jpg)
Credit: Eye Rounds
Postoperative Care and Recovery
Postoperative care is a crucial component in the recovery process after keratoprosthesis implantation. Patients are typically prescribed a regimen of topical medications, including antibiotics to prevent infection and anti-inflammatory drugs to reduce inflammation. Immunosuppressive medications are often used long-term to mitigate the risk of immune reactions against the artificial cornea.
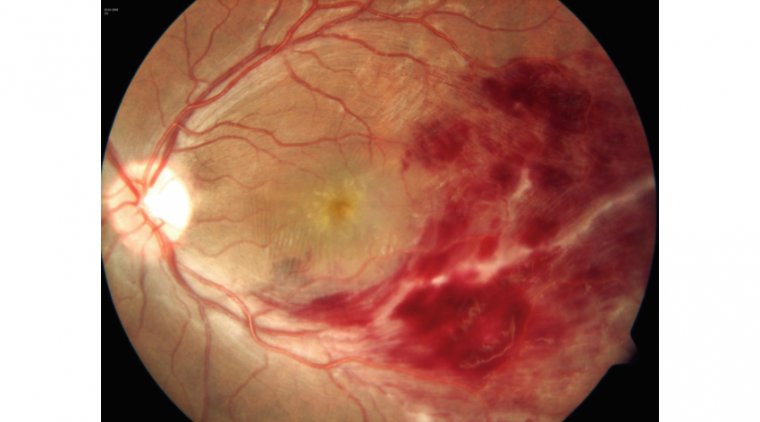
Regular follow-up visits are essential to monitor healing and assess the function of the artificial cornea. These visits also allow for the early detection and management of potential complications such as glaucoma, retinal detachment, or issues with the implant itself. The frequency of these visits may be high initially post-surgery and then gradually reduce over time, depending on the individual's healing progress and overall eye health.
Patients should be aware of the potential risks associated with keratoprosthesis, including the small chance of infection, persistent inflammation, or complications with the implant. However, with careful management, these risks can be significantly minimized.
Long-term maintenance is vital for the success of a keratoprosthesis. This includes adherence to medication regimens, maintaining good eye hygiene, protecting the eyes from injury, and promptly reporting any changes in vision or eye comfort to the healthcare provider.
Promoting healing and reducing the risk of complications involves a combination of medical management and patient participation. The role of patient awareness, adherence to postoperative care instructions, and commitment to follow-up care cannot be understated in the journey towards vision restoration after keratoprosthesis.
Benefits and Considerations
Keratoprosthesis presents a revolutionary solution for those suffering from severe corneal disease, offering potential benefits such as improved visual acuity and, subsequently, an enhanced quality of life. For many patients, particularly those for whom traditional corneal transplantation is not an option, keratoprosthesis may provide a renewed sense of hope and the opportunity to regain functional vision.
However, as with any surgical procedure, keratoprosthesis does come with its considerations and potential challenges. While the surgery itself can restore corneal clarity, the ultimate vision outcome depends on the health of other parts of the eye, particularly the retina and optic nerve.
There are also potential risks associated with the procedure, including infection, inflammation, glaucoma, and complications related to the implant itself. Furthermore, patients undergoing keratoprosthesis will require lifelong follow-up care and consistent use of medications to maintain the health of the eye and the function of the implant.
It's important for individuals considering keratoprosthesis to fully understand both the benefits and the potential challenges associated with the procedure. Consultation with a knowledgeable eye care professional is essential to discuss these factors, understand potential outcomes, and make an informed decision about this vision-restoring solution.
Summary
Keratoprosthesis represents a significant advance in ophthalmology, offering an alternative route for vision restoration in individuals with severe corneal disease. With the potential to improve visual acuity and enhance the quality of life, it is an option worth considering for those with limited alternatives. However, the procedure does come with considerations, including the need for lifelong monitoring and potential implant-related complications.
As advancements continue in keratoprosthesis technology and surgical techniques, the future for individuals with corneal disease holds promise. We encourage those interested in this procedure to seek professional advice and stay informed about the latest developments in artificial cornea implants. Remember, your vision is invaluable, and exploring all avenues for its preservation is a worthwhile endeavor.
(1).jpg)