A Comprehensive Review of Peters Anomaly
What Is Peters Anomaly?
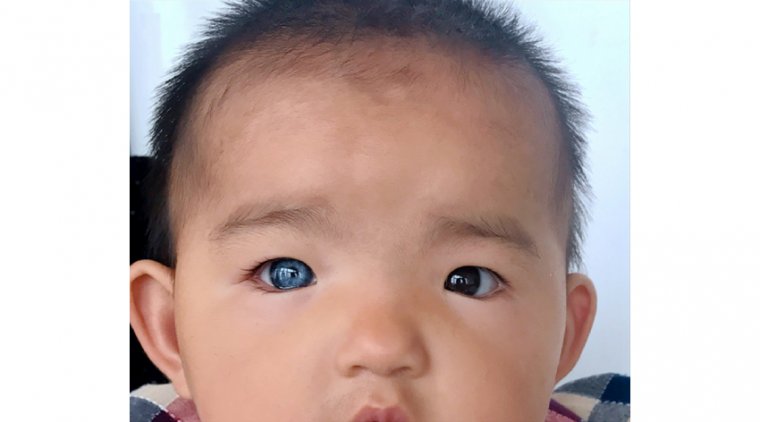
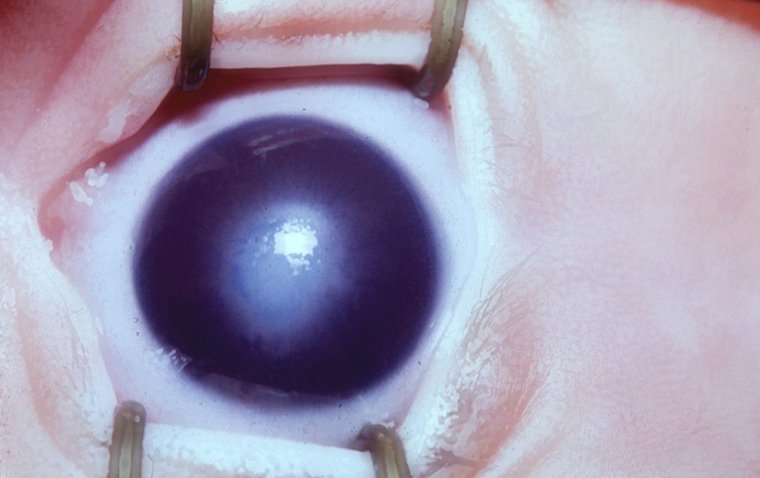
Peters anomaly is a rare congenital ocular condition primarily affecting the anterior segment of the eye. At its core, it's characterized by the abnormal development of the cornea's central layers and potential adhesions between the cornea and either the iris or the lens.
As a result, the affected eye may present with a central corneal opacity, which can range from a faint cloudiness to a dense white opacity, often accompanied by other eye abnormalities. The severity and presentation of Peters anomaly can vary, and in some cases, it might lead to significant vision impairment or blindness.
What Causes Peters Anomaly?
Peters Anomaly is a multifactorial condition, meaning that both genetic and environmental factors likely play a role in its development.
1. Genetic Factors
Several genetic mutations have been linked to peters anomaly. The most common ones involve genes like PITX2, CYP1B1, and FOXC1. In some families, multiple members might be affected, suggesting a hereditary component. Genetic testing and counseling can be beneficial for affected individuals and their families to understand the risk of recurrence in future generations.
2. Environmental Factors
While the precise environmental triggers are not yet clearly defined, certain in-utero exposures or maternal health conditions during pregnancy may contribute to the development of Peters Anomaly. For instance, prenatal exposure to certain medications or infections might increase the risk.
Risk Factors
Apart from genetic predispositions, other risk factors might include:
1. Maternal illnesses or infections during critical periods of fetal eye development.
2. Exposure to teratogenic drugs or substances during pregnancy.
3. A history of other ocular or systemic congenital anomalies in the child or family.
Types of Peters Anomaly
Peters Anomaly is a heterogeneous condition, presenting with varying degrees of severity and associated abnormalities. The condition is broadly classified into different types based on the clinical presentation:
Type I Peters Anomaly
● Central Corneal Opacity: This is the most characteristic feature of Type I. A white or clouded area appears in the central part of the cornea.
● Adhesions: There are iridocorneal or keratolenticular adhesions, where the cornea adheres to either the iris or the lens.
● Normal Descemet's membrane and endothelium: These deeper layers of the cornea are typically unaffected in Type I.
Type II Peters Anomaly
● Extensive Corneal Opacity: The corneal clouding in Type II is usually more severe and can involve the entire cornea.
● Abnormalities in Descemet's membrane and endothelium: Unlike Type I, Type II is characterized by abnormalities in the deeper layers of the cornea.
● Possible lens abnormalities: The lens can be dislocated, cataractous, or may even be absent (aphakia).
Peters Plus Syndrome
This is a more complex form of Peters Anomaly associated with systemic features. Apart from the corneal opacity and adhesions seen in classic Peters Anomaly:
● Short stature: Affected individuals are often shorter than their peers.
● Brachydactyly: Shortening of the fingers and toes.
● Cleft lip/palate: Some individuals may present with facial anomalies like a cleft lip or palate.
● Developmental delay: There can be varying degrees of intellectual disability or developmental delay.
Unveiling Peters Anomaly Symptoms
Peters Anomaly, a rare congenital ocular disorder, manifests primarily as corneal abnormalities. Recognizing the signs early can aid in better management and potential vision preservation. Here's a comprehensive look at the symptoms:
1. Corneal Opacity: The most distinguishing feature of Peters Anomaly is a cloudy or white appearance in the cornea, particularly the central portion. This opacity can range from a faint haze to a dense cloud, obstructing vision.
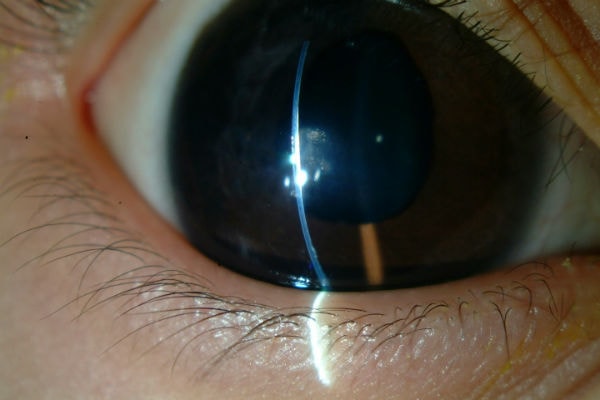
2. Iridocorneal or Keratolenticular Adhesions: These are attachments where the cornea sticks to either the iris (the colored part of the eye) or the lens. This can affect the eye's normal anatomy and interfere with vision.
3. Vision Impairment: Depending on the severity of the corneal opacity and any associated abnormalities, individuals with Peters Anomaly may experience reduced vision. In severe cases, it can lead to legal blindness.
4. Lens Abnormalities: In some individuals, especially those with Type II Peters Anomaly, there might be abnormalities of the lens, including cataracts, lens dislocation, or the complete absence of the lens (aphakia).
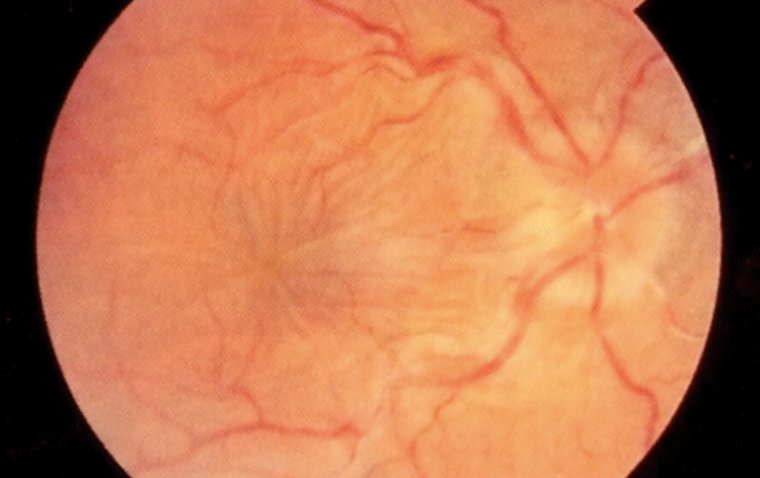
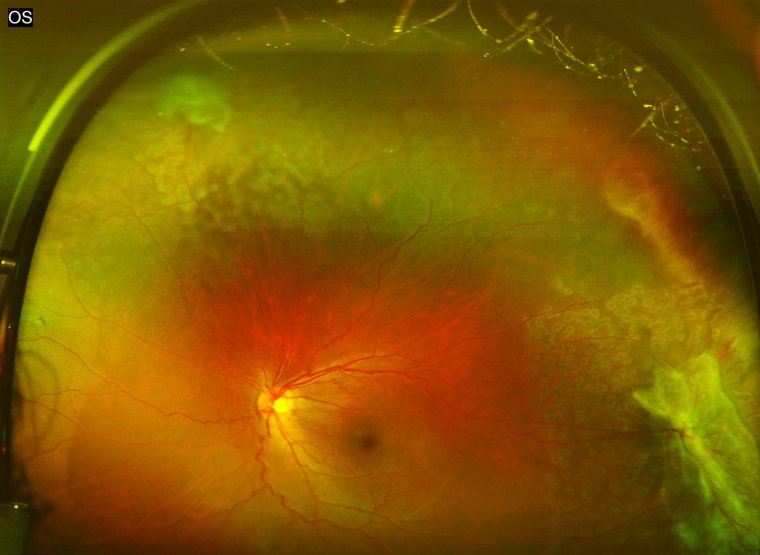
5. Secondary Glaucoma: The abnormal adhesions and anatomical changes in the eye can lead to increased intraocular pressure, resulting in glaucoma, a condition that can further reduce vision and even cause blindness if not treated.
6. Nystagmus: Some children with Peters Anomaly develop involuntary eye movements, or nystagmus, usually as a response to poor vision.
7. Strabismus: Misalignment of the eyes, commonly known as "crossed eyes" or "squint," can also be a symptom.
How to Diagnose Peters Anomaly
Identifying Peters Anomaly is paramount for immediate intervention and to ensure the best possible visual and developmental outcomes for affected individuals. Here’s a comprehensive insight into the diagnostic procedures:
Clinical Examination: The most fundamental step is a thorough ophthalmological examination. An ophthalmologist will use a slit-lamp, a device that provides a magnified view of the eye's structures, to inspect the cornea, iris, and lens. The presence of central corneal opacity, along with other eye anomalies, can strongly suggest Peters Anomaly.
Ultrasound Biomicroscopy (UBM): UBM can provide detailed imaging of the anterior segment of the eye, especially when corneal opacity makes it difficult to visualize internal structures directly. This test can detect iridocorneal or keratolenticular adhesions.
Optical Coherence Tomography (OCT): OCT of the anterior segment can provide high-resolution cross-sectional images of the cornea and anterior chamber. This helps in assessing the depth and extent of corneal abnormalities.
Genetic Testing: As there are hereditary patterns associated with Peters Anomaly, genetic testing can be invaluable. Certain genes, when mutated, are linked to the anomaly. Genetic testing can help confirm the diagnosis, especially in ambiguous cases or when planning for familial counseling.
Systemic Evaluation: Considering Peters Anomaly can sometimes be part of a broader syndrome, a pediatric or genetic evaluation may be recommended to rule out associated systemic abnormalities or syndromes like Peters Plus Syndrome.
Family History: A detailed family history can be informative, especially if there are other family members with similar ocular or systemic features. This can give hints about a possible hereditary pattern.
Pediatric Examination: Since Peters Anomaly can present alongside developmental delays or other physical abnormalities, a thorough pediatric examination is crucial.
Importance of Early Detection: Early diagnosis of Peters Anomaly is pivotal. With timely intervention, potential complications can be managed, leading to improved visual outcomes. For those with hereditary patterns, early detection offers the advantage of genetic counseling, aiding future family planning decisions.
Peters Anomaly Treatment
Peters Anomaly, a congenital disorder of the anterior segment of the eye, requires specialized and often multidisciplinary care to ensure the best outcomes for affected individuals. This section provides a comprehensive insight into the treatments available:
Medical Interventions
● Lubricating Eye Drops: These are prescribed to alleviate dryness and discomfort. Given the frequent association of Peters anomaly with dry eye, lubricants can help maintain corneal health.
● Antibiotic Eye Drops: If there's a risk or presence of an eye infection due to a compromised corneal barrier, antibiotic drops might be prescribed.
● Topical Steroids: Inflammation can occasionally be a concern, for which topical steroids may be indicated, albeit with careful monitoring.
Surgical Interventions
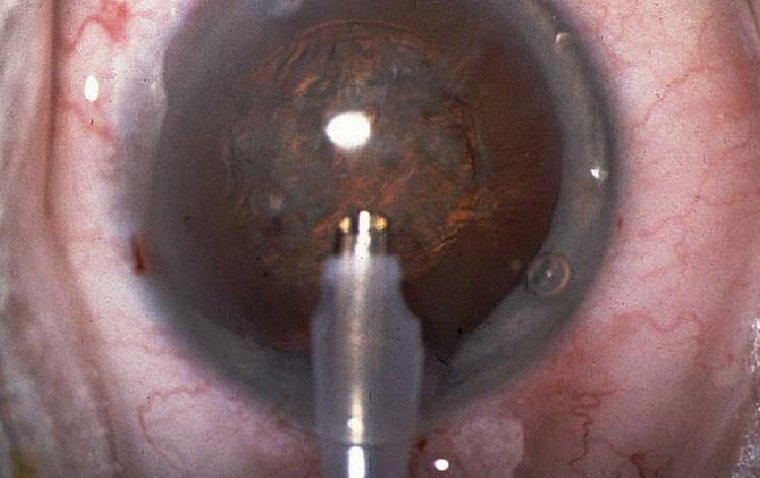
● Penetrating Keratoplasty (PK): This full-thickness corneal transplant may be considered for children with severe central corneal opacity affecting vision, especially when there's a potential for visual development.
● Deep Anterior Lamellar Keratoplasty (DALK): In cases where the back layer of the cornea is intact, this partial-thickness corneal transplant can be employed, offering fewer complications compared to PK.
● Goniotomy: If there's associated glaucoma, this procedure can help decrease intraocular pressure.
● Lens Procedures: In some cases, the lens of the eye might also be affected or can cause further complications. Procedures such as lens extraction or intraocular lens implantation might be considered.
Multidisciplinary Approach
The complexity of Peters Anomaly and its potential association with other systemic issues necessitates a holistic treatment approach.
● Pediatric Specialists: Given the potential association of Peters anomaly with developmental delays or other physical anomalies, a pediatrician's involvement is essential.
● Genetic Counselors: They play a role in family counseling, especially when a hereditary pattern is identified.
● Ophthalmologists: They lead the care in terms of ocular diagnosis, monitoring, and interventions.
● Vision Rehabilitation Specialists: They offer guidance on visual aids, techniques, and strategies to optimize the affected individual's functional vision and overall quality of life.
Research and Advancements
The realm of ophthalmology, particularly concerning congenital ocular anomalies like Peters Anomaly, has witnessed remarkable progress in recent years. With technology, genetics, and enhanced clinical practices coming to the fore, our understanding and management of Peters Anomaly continue to evolve. This section delves into the ongoing research and breakthroughs that promise hope and improved care for affected individuals.
1. Genetic Discoveries:
Recent advancements in genome sequencing have led to the identification of various genes associated with Peters Anomaly, such as PITX2, FOXE3, and PAX6. Understanding the genetic underpinnings helps in early diagnosis, better prognosis predictions, and potential genetic therapies.
Gene therapy research is in the early stages but holds promise for addressing the root genetic causes of the condition.
2. Stem Cell Research:
Stem cell treatments are gaining traction as a potential therapeutic strategy. Lab-grown corneal tissues derived from stem cells could offer a future alternative to traditional corneal transplants.
Studies are underway to understand the potential of stem cells in repairing damaged or underdeveloped ocular tissues in conditions like Peters Anomaly.
3. Advanced Imaging Techniques:
Novel imaging technologies such as high-resolution anterior segment optical coherence tomography (AS-OCT) have improved the detailed visualization of anterior segment abnormalities, aiding in accurate diagnosis and surgical planning.
4. Bioengineered Corneas:
Research is progressing on developing bioengineered corneas using collagen matrices and human cells. These hold the potential to replace damaged corneal tissue, offering an alternative to donor transplants.
5. Pharmacological Advancements:
Ongoing research is focusing on drugs that can modulate wound healing post-surgery, minimize scarring, and optimize graft success rates.
6. Holistic Treatment Protocols:
Recognizing the systemic implications of Peters Anomaly, there's a trend towards creating holistic treatment models that integrate ophthalmological care with pediatric, genetic, and psychological interventions.
Summary
Peters Anomaly is a complex ocular condition with both genetic and environmental underpinnings. Given its potential implications for vision and overall ocular health, the emphasis on early detection cannot be overstated. Prompt diagnosis paves the way for timely interventions, optimizing the chances of better visual outcomes and potentially preventing further complications.
Staying updated on the latest research and advancements can equip individuals and their caregivers with the knowledge to make informed decisions about care. As science continues to shed light on Peters Anomaly, it brings hope of improved treatments and a deeper understanding of the condition.
For those affected or at risk, maintaining an open line of communication with ophthalmologists and pediatric specialists is crucial. Personalized care tailored to the unique needs of each individual can make a significant difference in managing and potentially mitigating the effects of Peters Anomaly.
(1).jpg)