Dry Eye Disease (DED) & Meibomian Gland Dysfunction (MGD)
Dry Eye Disease (DED)
Dry Eye Disease (DED) is a common ocular disorder affecting millions of people worldwide. It is a chronic and progressive condition that can lead to significant discomfort, decreased quality of life, and visual disturbances.
Causes of Dry Eye Disease
DED can be caused by a variety of factors, including:
|
Causes |
Description |
|
Age |
As we age, the production of tears decreases, leading to dry eyes. |
|
Hormonal changes |
Women are more likely to develop DED due to hormonal changes during pregnancy, menopause, and the use of birth control pills. |
|
Environmental factors |
Exposure to dry or windy conditions, air conditioning, and smoke can cause DED. |
|
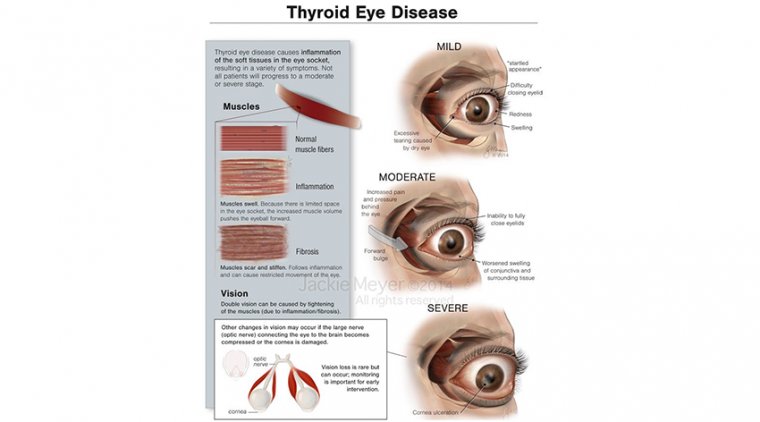
Systemic diseases |
Rheumatoid arthritis, Sjogren's syndrome, and thyroid disorders can lead to DED. |
|
Medications |
Certain medications, such as antihistamines, decongestants, and antidepressants, can cause DED. |
Symptoms of Dry Eye Disease
The symptoms of DED can vary from mild to severe and can include:
|
Symptoms |
Description |
|
Dryness |
The eyes may feel dry, gritty, or itchy. |
|
Redness |
The eyes may be red or bloodshot. |
|
Irritation |
The eyes may feel irritated or burning. |
|
Sensitivity to light |
The eyes may be sensitive to light. |
|
Blurred vision |
Vision may be blurry or fluctuate. |
Diagnosis of Dry Eye Disease
The diagnosis of DED typically involves a comprehensive eye examination, which may include:
|
Diagnosis |
Description |
|
Evaluation of tear production |
A Schirmer test or tear breakup time test may be used to measure the quantity and quality of tears. |
|
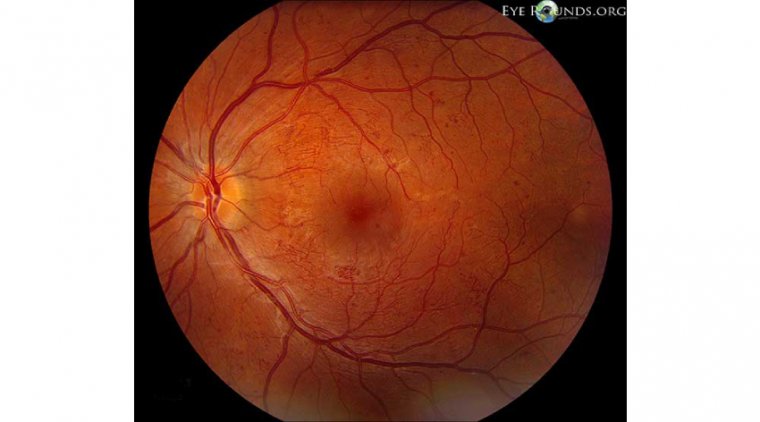
Examination of the ocular surface |
The doctor may use a slit lamp to examine the cornea and conjunctiva for signs of inflammation, scarring, or damage. |
|
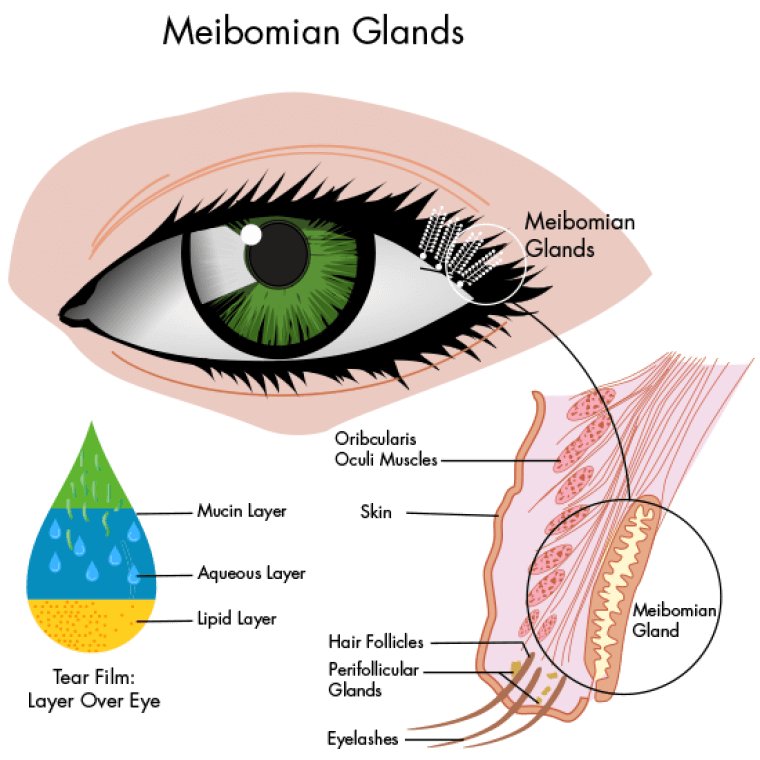
Assessment of meibomian gland function |
The meibomian glands produce the oil component of tears, and dysfunction of these glands can cause DED. The doctor may evaluate the meibomian gland function using meibography or other techniques. |
Treatment Options for Dry Eye Disease
|
Treatment |
Description |
|
Environmental Modifications |
Avoiding or reducing exposure to dry or windy conditions, using a humidifier, and taking breaks when using a computer can help alleviate symptoms. |
|
Artificial Tears |
The use of lubricating eye drops or ointments can help moisturize the eyes |
|
Medications |
Prescription medications, such as cyclosporine and lifitegrast, can help reduce inflammation and increase tear production. |
|
Lipid-Based Eye Drops |
These eye drops contain lipids that help restore the lipid layer of the tear film, which can help reduce tear evaporation and improve tear film stability. |
|
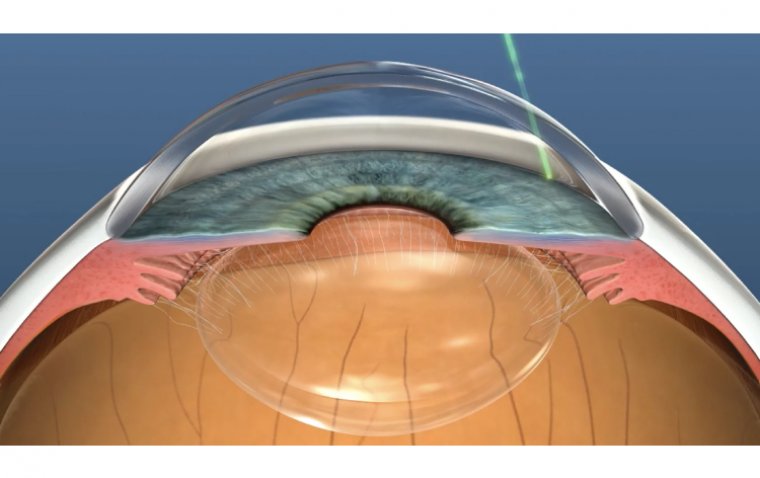
Punctal Plugs |
These tiny devices are inserted into the tear ducts to help retain tears on the ocular surface |
|
Intense Pulsed Light Therapy |
This therapy uses a specific wavelength of light to reduce inflammation and improve meibomian gland function. |
Meibomian Gland Dysfunction (MGD)
Meibomian Gland Dysfunction (MGD) is a common condition that affects the function of the meibomian glands, which are located in the eyelids and produce the oil component of tears. MGD can lead to evaporative dry eye disease and other ocular surface problems.
Causes of Meibomian Gland Dysfunction
|
Causes |
Description |
|
Aging |
As we age, the meibomian glands can become obstructed, leading to dysfunction. |
|
Hormonal changes |
Hormonal changes, such as those that occur during menopause, can affect the function of the meibomian glands. |
|
Environmental factors |
Exposure to dry or windy conditions, air conditioning, and smoke can lead to MGD. |
|
Systemic diseases |
Certain systemic diseases, such as rosacea, can affect the meibomian glands and lead to dysfunction. |
Symptoms of Meibomian Gland Dysfunction
|
Symptoms |
Description |
|
Dryness |
The eyes may feel dry or gritty. |
|
Redness |
The eyes may be red or bloodshot. |
|
Irritation |
The eyes may feel irritated or burning. |
|
Sensitivity to light |
The eyes may be sensitive to light. |
|
Blurred vision |
Vision may be blurry or fluctuate. |
|
Eyelid inflammation |
Inflammation of the eyelids, known as blepharitis, is a common symptom of MGD. |
Diagnosis of Meibomian Gland Dysfunction
The diagnosis of MGD typically involves a comprehensive eye examination, and it is similar as Dry Eye Disease diagnosis except;
|
Diagnosis |
Description |
|
Evaluation of eyelid inflammation |
The doctor may assess the degree of eyelid inflammation using a variety of methods, such as the Blepharitis Index. |
Treatment Options for Meibomian Gland Dysfunction
|
Treatment |
Description |
|
Warm compresses |
Applying warm compresses to the eyelids can help soften the oil in the meibomian glands and improve gland function. |
|
Lid hygiene |
Proper eyelid hygiene, including daily lid scrubs, can help reduce inflammation and improve gland function. |
|
Medications |
Prescription medications, such as antibiotics and anti-inflammatory drugs, may be used to treat underlying eyelid inflammation and improve gland function. |
|
Lipid-based eye drops |
These eye drops contain lipids that help restore the lipid layer of the tear film, which can help reduce tear evaporation and improve tear film stability. |
|
Punctal plugs |
These tiny devices are inserted into the tear ducts to help retain tears on the ocular surface. |
|
Intense pulsed light therapy |
This therapy uses a specific wavelength of light to reduce inflammation and improve meibomian gland function. |
The Connection between Dry Eye Disease and Meibomian Gland Dysfunction
MGD is the most common underlying cause of evaporative DED, accounting for up to 86% of cases. The dysfunction or obstruction of the meibomian glands leads to a reduction in the lipid layer of the tear film, causing an increased rate of tear evaporation and destabilization of the tear film.
Additionally, the inflammation caused by MGD can damage the ocular surface and further exacerbate the symptoms of DED. The chronic inflammation can also lead to the loss of meibomian gland function and even atrophy, making the condition more difficult to treat.
In conclusion, DED and MGD are closely interconnected, with MGD being the most common underlying cause of evaporative DED. Understanding the connection between these two conditions is essential for the proper diagnosis and management of DED, and early intervention is critical to preventing further damage to the ocular surface.
(1).jpg)