When Pressure Drops: Exploring the Enigma of Hypotony Maculopathy
What Is Hypotony Maculopathy?
Borrowing from the language of meteorology, we often talk about intraocular pressure (IOP) in the eye akin to the atmospheric pressure that shapes our weather. But what happens when this pressure drops significantly, much like a sudden atmospheric low pressure leading to stormy conditions? The result is a unique and somewhat enigmatic condition we call Hypotony Maculopathy.
Definition and Overview
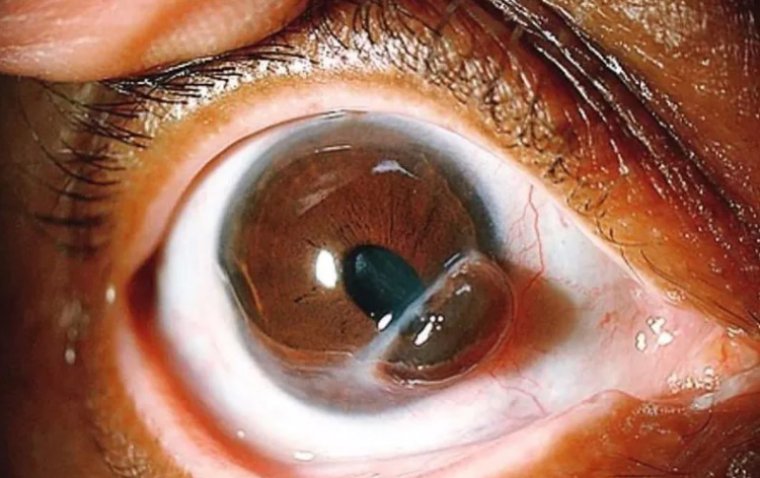
Hypotony Maculopathy is characterized by a drop in intraocular pressure (IOP) to a level that's significantly below the average range of 10 to 21 mm Hg. In simple terms, the eye is not sufficiently 'inflated', which can lead to a variety of complications. One of the most significant complications is a change in the macula, the central part of the retina responsible for detailed vision.
Just like a sudden drop in atmospheric pressure can give rise to turbulent weather, low intraocular pressure can bring about its own tempest within the eye, in the form of structural changes and visual disturbances. These changes, particularly in the macula, give this condition its name: Hypotony Maculopathy. This condition is both a fascinating and perplexing phenomenon, serving as a stark reminder of the delicate balance that maintains our ocular health.
Impact on the Macula
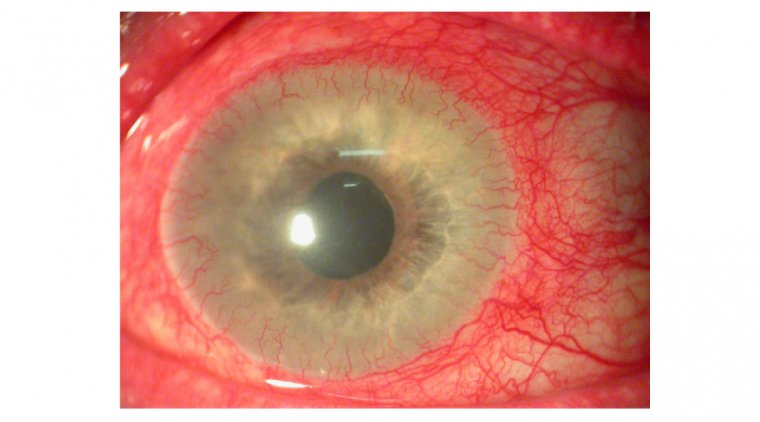
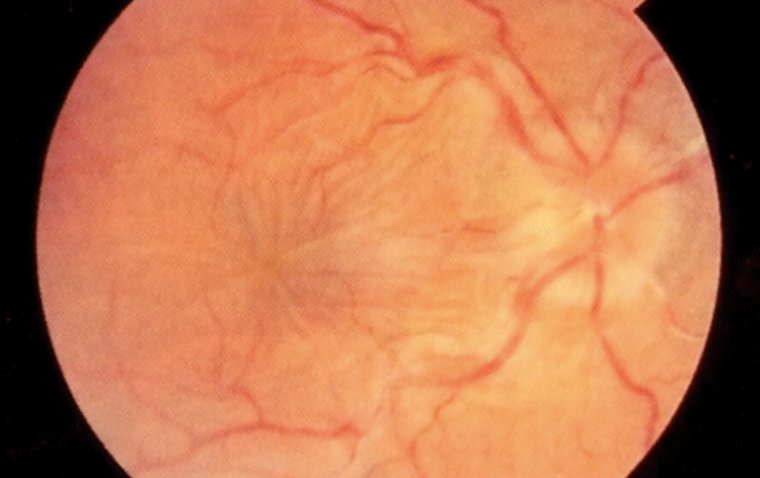
The macula, known for its role in providing sharp, clear, central vision, becomes a casualty of this pressure drop. In Hypotony Maculopathy, low IOP can lead to changes in the shape and structure of the macula, potentially causing wrinkling or edema (swelling). These changes can have a profound effect on the eye's ability to process fine detail, impacting activities that require sharp vision, such as reading or recognizing faces.
.jpg)
What Causes Hypotony Maculopathy?
Hypotony Maculopathy, while not as common a forecast in the ophthalmic weather report, can be a rather ominous low-pressure system in our patients' eyes. Understanding the causative factors is crucial in navigating this stormy situation.
Underlying Causes and Risk Factors
Much like a complex weather system, hypotony maculopathy arises from a combination of factors. Essentially, anything that causes a significant decrease in intraocular pressure (IOP) can potentially lead to hypotony maculopathy.
Conditions and Procedures Leading to Reduced Intraocular Pressure
● Ocular Surgery: Certain types of ocular surgeries, particularly glaucoma surgery and retinal detachment repair, can lead to a drop in IOP. This can occur if there's over-filtration or leakage of aqueous humor following surgery.
● Ocular Trauma: Any injury to the eye that affects the production or drainage of aqueous humor can potentially lead to hypotony.
● Ocular Inflammation: Conditions causing inflammation within the eye, such as uveitis, can disrupt normal aqueous humor dynamics, possibly leading to hypotony.
Potential Contributors to Hypotony
The factors contributing to hypotony can be diverse and multifaceted:
1. Uveitis: Inflammation within the eye can affect the ciliary body, reducing aqueous humor production and leading to hypotony.
2. Ciliary Body Dysfunction: If the ciliary body, which produces the aqueous humor, is dysfunctional, there may not be enough fluid to maintain proper intraocular pressure. This can happen in conditions like ciliary body detachment or shutdown.
3. Excessive Drainage of Aqueous Humor: Some conditions or situations might result in excessive drainage of the aqueous humor, such as over-filtration following glaucoma surgery or a leaking wound post ocular surgery.
Signs and Symptoms of Hypotony Maculopathy
The first few raindrops heralding an impending storm, symptoms of Hypotony Maculopathy are warning signs that can help us identify and address this condition early. Like a skilled meteorologist spotting signs of a developing storm, a vigilant ophthalmologist must watch for these early indicators.
Symptoms of Hypotony Maculopathy
● Decreased Visual Acuity: The most common symptom associated with Hypotony Maculopathy is a decrease in visual acuity. This can vary from slight blurriness to a significant reduction in vision, depending on the severity of the condition.
● Distorted or Blurry Vision: Some patients may report metamorphopsia, a distortion or warping of vision. This symptom is often a result of macular changes caused by the low intraocular pressure.
● Central Vision Loss: In severe cases, Hypotony Maculopathy can lead to central vision loss, significantly affecting a person's ability to carry out tasks that require detailed vision, such as reading or recognizing faces.
Additional Signs and Symptoms
The "weather conditions" in the eye may exhibit additional signs suggestive of Hypotony Maculopathy:
Macular Edema: This involves swelling or thickening of the macula due to fluid accumulation. It can be seen during a fundoscopic exam and may result in distorted and diminished vision.
Choroidal Folds: These are visible creases or folds in the layer beneath the retina, often seen in Hypotony Maculopathy. They are typically observed during an ophthalmic exam.
Optic Nerve Head Swelling: Also known as optic disc edema, this is a sign of increased fluid pressure in the optic nerve. It can be seen during a comprehensive eye exam.
How to Diagnose Hypotony Maculopathy
Just as a meteorologist uses a barometer to measure atmospheric pressure changes signaling impending weather conditions, so too must an ophthalmologist utilize specific tools to diagnose hypotony maculopathy. Let's delve into how we identify this low-pressure system in the eye.
Diagnostic Process
The process of diagnosing hypotony maculopathy involves a combination of clinical history, physical examination, and specialized tests:
● History Taking: The first step is a comprehensive history, which can provide clues to potential causes of hypotony maculopathy. Prior ocular surgeries, trauma, or systemic diseases are particularly relevant.
● Physical Examination: This includes a detailed examination of the eye, with specific attention to the anterior segment for signs of trauma, inflammation, or surgical complications.
Evaluation of Intraocular Pressure
An essential component of diagnosing hypotony maculopathy is measuring intraocular pressure (IOP). This is usually done using a tonometer, a device that measures the resistance of the cornea to indentation.
*Normal IOP: Typically, IOP ranges between 10 and 21 mm Hg.
*Low IOP: Hypotony is generally defined as an IOP of 5 mm Hg or less, although maculopathy can occur at higher pressures in some individuals.
Examination of the Macula and Additional Diagnostic Tests
Fundus Examination: This involves examining the back of the eye, including the retina and macula, for signs of hypotony maculopathy such as choroidal folds or macular edema.
Optical Coherence Tomography (OCT): This non-invasive imaging test can provide a detailed view of the retina and help identify changes consistent with hypotony maculopathy, such as retinal thickening or folds.
Fluorescein Angiography: While not typically necessary for diagnosis, this test can help rule out other conditions and evaluate the extent of retinal damage in certain cases.
Treatment Options for Hypotony Maculopathy
Just as a weather forecast guides us in choosing the right gear, understanding the available treatment options for hypotony maculopathy can help us equip our patients with the best care plan. This section will be our umbrella, protecting us from the downpour of uncertainty that often accompanies this condition.
Managing Intraocular Pressure
The primary goal in treating hypotony maculopathy is to increase intraocular pressure (IOP) and prevent further damage to the macula. This involves:
● Observation: In some mild cases, simply monitoring the condition may be enough. The IOP may return to normal levels on its own, especially if the hypotony is postoperative.
● Medications: Topical and systemic corticosteroids may be used to reduce inflammation and increase IOP.
● Lifestyle Modifications: Certain changes, such as avoiding high fluid intake and certain body postures, may help increase IOP.
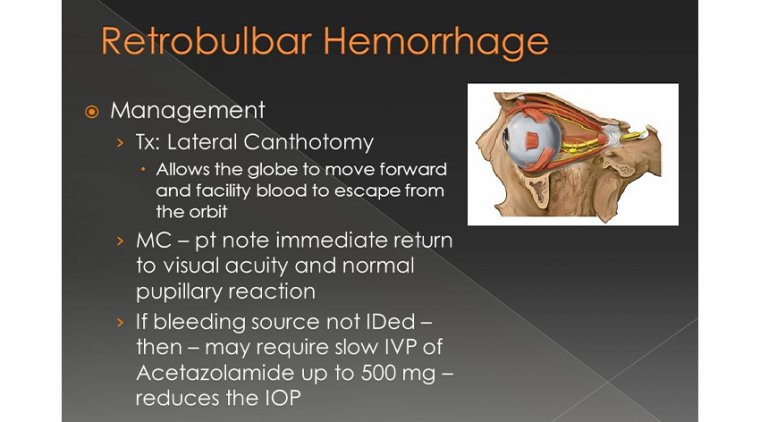
Surgical Interventions
When conservative measures fail to increase IOP adequately or if there is an identifiable cause that can be corrected surgically, several procedures can be considered:
Patching the Leaking Site: If a leak is identified as the cause of hypotony, surgical repair of the site may be undertaken to prevent further leakage of aqueous humor.
Implantation of Tissue Grafts: In cases where overfiltration is due to a surgically created drainage pathway, a graft can be implanted to slow the drainage.
Use of Drainage Devices: Drainage devices may be inserted to control aqueous humor flow and maintain a balanced IOP.
Prevention and Risk Reduction
The adage "prevention is better than cure" rings particularly true in the context of hypotony maculopathy. As healthcare providers, we must equip ourselves with the proverbial raincoat and umbrella to shield our patients from this 'low-pressure system.'
Preventive Measures and Risk Reduction Strategies
In the medical field, our weather forecasts come in the form of preventative strategies. Here are some preventive measures that can potentially reduce the risk of hypotony maculopathy:
● Appropriate Surgical Techniques: Careful surgical techniques and handling of ocular tissues during ocular surgery, particularly glaucoma surgery, can minimize the risk of postoperative hypotony.
● Cautious Management of Ocular Inflammation: Prompt and adequate management of ocular inflammatory conditions such as uveitis can help prevent hypotony.
● Postoperative Care: Rigorous postoperative follow-up and management can identify and address any reduction in IOP early on.
Research and Advances in Hypotony Maculopathy
Like intrepid explorers charting the unexplored territories of our world, researchers are pioneering advancements in our understanding of hypotony maculopathy. This section takes a peek at these 'cartographers' of the ophthalmic landscape.
Current research efforts in hypotony maculopathy are primarily focused on:
● New Diagnostic Tools: Researchers are exploring advanced imaging techniques to detect hypotony maculopathy earlier and with greater precision.
● Novel Therapeutic Approaches: Clinical trials are investigating new drugs and surgical techniques to increase intraocular pressure and prevent macular changes.
● Understanding Pathophysiology: More in-depth studies are being conducted to further understand the pathophysiological mechanisms that contribute to hypotony maculopathy.
With these advances, we are not merely predicting the 'weather patterns' of hypotony maculopathy, but also shaping the way we manage this condition.
To Conclude...
In the world of ophthalmology, we're all too familiar with the storms that conditions like hypotony maculopathy can bring. As we've navigated through the low-pressure system of this condition, we've seen its causes, its effects, and its potential treatment options. We've also looked at how we can prepare our patients for any 'weather conditions' they may face, through preventative measures and patient education.
But the forecast isn't entirely gloomy. With ongoing research and advancements in the field, the future looks promising. We're developing more refined diagnostic tools, exploring novel therapeutic interventions, and deepening our understanding of the pathophysiology of hypotony maculopathy. Just as a seasoned mariner learns to read the changing skies, we too are learning more each day about this unique condition, enabling us to better steer our patients through their journeys.
So while hypotony maculopathy may continue to present us with challenges, we can take comfort in the fact that we are not weathering this storm alone. Together, with our shared knowledge and determination, we'll continue to break the clouds of uncertainty and shine a light on better patient outcomes.
After all, even the rainiest days can't last forever, and as every seasoned ophthalmologist knows - after the storm, there's always a rainbow.
(1).jpg)