Vision Restoration Breakthrough: Retinal Therapy Achieves First Long-Term Neural Regeneration
In a groundbreaking development for ophthalmology, researchers from KAIST have achieved the first successful induction of long-term neural regeneration in mammalian retinas, potentially paving the way to restore vision lost to degenerative retinal diseases.
Unmet Need in Retinal Regeneration
With over 300 million people worldwide at risk of vision loss due to retinal diseases, the need for restorative therapies has never been greater. While many treatments aim to slow disease progression, no approved therapy exists to reverse retinal damage and restore vision—until now.
Pioneering Research by KAIST and Celliaz Inc.
A research team led by Professor Jinwoo Kim from the Department of Biological Sciences at KAIST has developed a novel therapeutic approach that successfully regenerates retinal neurons and restores vision. The study, published in Nature Communications, was co-authored by Dr. Eun Jung Lee of Celliaz Inc. and Museong Kim, a Ph.D. candidate at KAIST.
Blocking PROX1 to Restore Retinal Nerve Function
The researchers identified the PROX1 (Prospero Homeobox 1) protein as a key inhibitor of retinal regeneration. In a disease-model mouse, administering a compound that blocks PROX1 enabled regeneration of retinal nerves and led to vision recovery lasting over six months.
This marks the first successful demonstration of long-term neural regeneration in the mammalian retina and represents a major leap forward in regenerative ophthalmology.
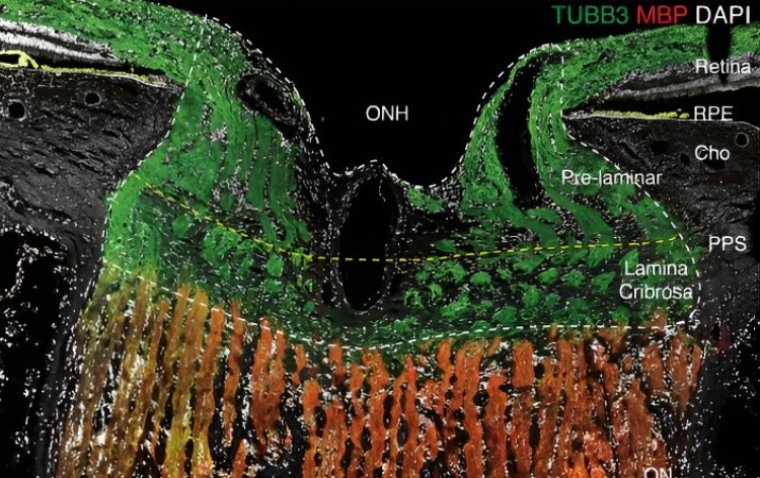
Understanding the Science Behind Regeneration
Cold-blooded species like fish naturally regenerate retinal neurons through the dedifferentiation of Müller glia into neural progenitor cells. In contrast, mammalian Müller glia lacks this capability, leading to permanent retinal damage.
The study revealed that in mammals, PROX1 accumulates in damaged Müller glia and inhibits their ability to dedifferentiate. Interestingly, this protein is not produced by the glia themselves but absorbed by surrounding neurons that fail to degrade it and instead secrete it.
A Novel Antibody Therapy Developed by Celliaz Inc.
To counter this mechanism, the researchers developed a therapeutic strategy to neutralize extracellular PROX1 before it interacts with Müller glia. This involved the use of a high-affinity PROX1-neutralizing antibody, discovered by Celliaz Inc., a biotech startup established from Professor Kim’s lab.
• When injected into disease-model mouse retinas, the antibody promoted significant neural regeneration.
• When delivered as a gene therapy in mice with congenital retinal degeneration, the treatment enabled sustained neuron production and vision restoration for over six months.
Toward Clinical Application by 2028
Celliaz Inc. is currently developing this retinal regeneration-inducing therapy for use in patients with various degenerative retinal conditions, including those for which no current treatments exist. The company aims to initiate clinical trials by 2028.
“We are finalizing improvements to the efficacy of the PROX1-neutralizing antibody (CLZ001) and aim to complete vision restoration efficacy and safety evaluations in multiple animal models before administering it to retinal disease patients,” said Dr. Eun Jung Lee. “Our goal is to provide a real solution for patients at risk of blindness who currently lack proper treatment options.”
Reference:
Eun Jung Lee et al, Restoration of retinal regenerative potential of Müller glia by disrupting intercellular Prox1 transfer, Nature Communications (2025). DOI: 10.1038/s41467-025-58290-8
(1).jpg)