Microscale Eye Implant Could Be Used to Treat Diabetes and Other Diseases
In Sweden, researchers have created a microscale device designed for implantation in the eye, opening up new paths for cell-based treatments for conditions like diabetes.
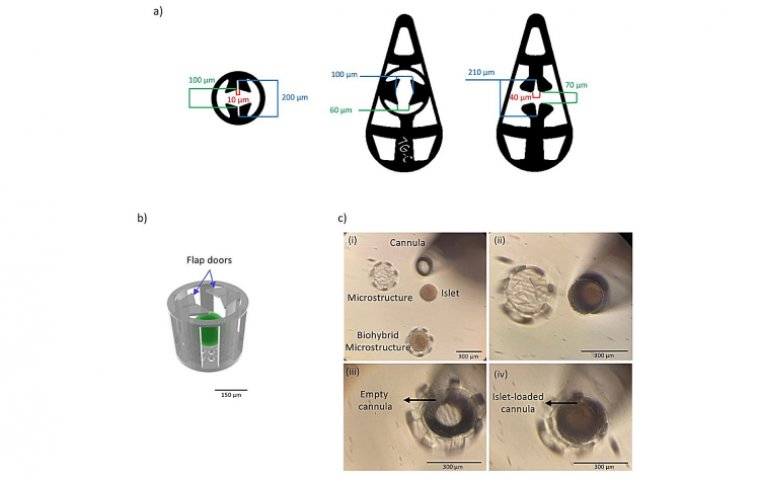
Developed by a team from KTH Royal Institute of Technology and Karolinska Institutet, this 3D-printed device aims to encapsulate insulin-producing pancreatic cells and electronic sensors. Their findings have been published in the journal Advanced Materials.
The collaboration between KTH and Karolinska Institutet has facilitated precise placement of micro-organs, particularly pancreatic islets or islets of Langerhans, within the eye without requiring sutures. This advancement holds promise for cell-based therapies, such as the treatment of type 1 or type 2 diabetes, leveraging the eye as a platform.
According to Anna Herland, a senior lecturer in the Division of Bionanotechnology at SciLifeLab at KTH and the AIMES research center at KTH and Karolinska Institutet, the eye is an ideal choice for this technology due to its lack of immune cells that typically react negatively during the initial implantation phase. Its transparency also allows for visual and microscopic monitoring of the implant's progress over time.
The device is wedge-shaped, measuring approximately 240 micrometers in length, enabling it to be mechanically secured at the angle between the iris and the cornea within the anterior chamber of the eye (ACE). This research represents the initial instance of mechanically affixing a device in the anterior chamber of the eye.
"We designed the medical device to hold living mini-organs in a micro-cage and introduced the use of a flap door technique to avoid the need for additional fixation," says Wouter van der Wijngaart, professor in the Division of Micro- and Nanosystems at KTH.
In experiments conducted on mice, the device remained in place within the living organism for several months. Furthermore, the miniature organs rapidly integrated with the host animal's blood vessels and operated as expected, according to Herland.
Per-Olof Berggren, a professor of experimental endocrinology at Karolinska Institutet, brought his extensive experience in transplanting islets of Langerhans to the anterior chamber of the eye in mice to contribute to this research.
"The current unit is unique and will among other things form the basis for our continued work to develop an integrated microsystem for studying the function and survival of the islets of Langerhans in the anterior chamber of the eye," Berggren says. "This is also of great translational importance, as transplantation of Langerhans islands to the anterior chamber of the eye in humans is subject to clinical trials in patients with diabetes."
According to Herland, this technology addresses a significant hurdle in the advancement of cell therapies, including those for diabetes. Specifically, it eliminates the requirement for invasive techniques to monitor the graft's performance and guide patient care, ensuring the long-term success of transplants.
"Ours is a first step towards advanced medical microdevices that can both localize and monitor the function of cell grafts. Our design will enable future integration and use of more advanced device functions such as integrated electronics or drug release" she concluded.
For further exploration of how this innovation aligns with broader trends in the medical field, the article "The Role of 3D Printing Today and Tomorrow" provides insight into the growing impact of 3D printing technologies in medicine, including their potential to revolutionize treatments for a variety of conditions.
Reference
Hanie Kavand et al, 3D‐Printed Biohybrid Microstructures Enable Transplantation and Vascularization of Microtissues in the Anterior Chamber of the Eye, Advanced Materials (2023). DOI: 10.1002/adma.202306686
(1).jpg)