Restoring Vision with Limbal Stem Cell Transplantation
What Are Limbal Stem Cells?
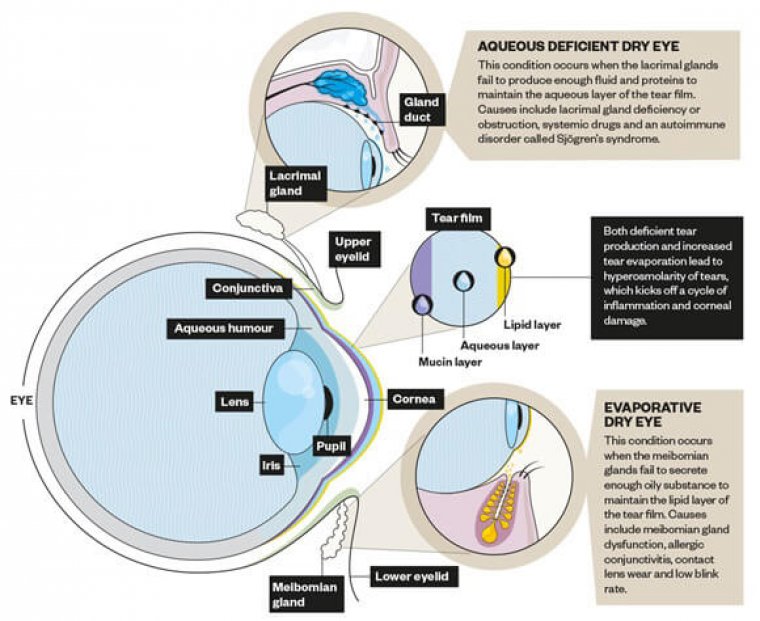
Limbal stem cells are adult stem cells found in the limbus, a region located between the cornea and the eye's conjunctiva. These cells are responsible for maintaining the health and integrity of the cornea, which is the clear, dome-shaped tissue that covers the front of the eye. The cornea is responsible for refracting light and focusing it onto the retina, which sends visual information to the brain.
Limbal stem cells play a critical role in the cornea's health by regenerating the corneal epithelium, which is the cornea's outermost layer. The corneal epithelium acts as a barrier that protects the cornea from the environment, including exposure to dust, pollutants, and other foreign particles. It also prevents infection and helps maintain the cornea's clarity, which is essential for good vision.
What Is A Limbal Stem Cell Transplantation?
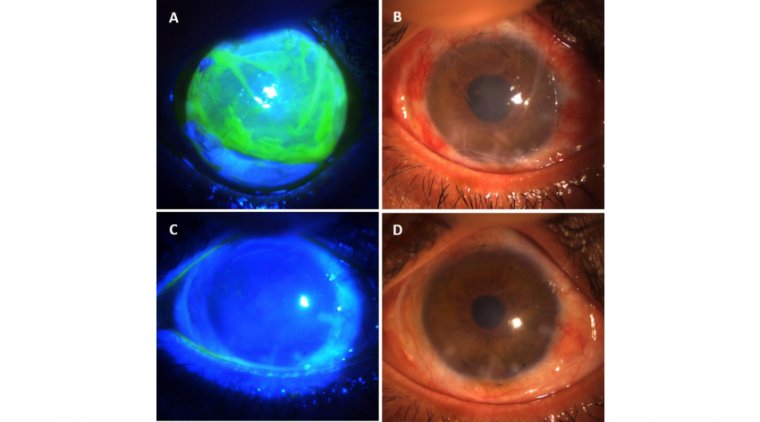
A limbal stem cell transplant is a surgical procedure that involves transplanting healthy limbal stem cells from a donor or the patient's healthy eye onto the affected eye to regenerate the corneal epithelium. The transplant helps restore the cornea's integrity and improve vision in cases of limbal stem cell deficiency (LSCD).
What Are The Different Types Of Limbal Stem Cell Transplants?
There are two main types of limbal stem cell transplants: autologous and allogeneic. Autologous transplants involve harvesting limbal stem cells from the patient's healthy eye and transplanting them onto the affected eye. On the other hand, allogeneic transplants involve obtaining limbal stem cells from a donor and transplanting them onto the affected eye.
Autologous limbal stem cell transplant is the preferred option when possible, as it avoids the risk of immune rejection of the transplanted tissue. The surgeon harvests a small piece of healthy limbus from the patient's healthy eye and transplants it onto the affected eye. The transplanted tissue can regenerate the corneal epithelium and restore the integrity of the cornea. Autologous transplants have a high success rate, mainly when the transplant is performed early in the course of the disease.
Allogeneic limbal stem cell transplant is a suitable option when the patient's healthy eye does not have enough limbal stem cells or if the disease is too advanced to harvest sufficient healthy tissue. The donor tissue is carefully screened to minimize the risk of immune rejection and disease transmission. The success rate of allogeneic transplants can be lower than autologous transplants, but the procedure can potentially restore the corneal epithelium and improve vision in severe cases.
What Are The Potential Complications Of Limbal Stem Cell Transplants?
Limbal stem cell transplant can have potential complications, as with any surgical procedure. Some of the potential complications of limbal stem cell transplant include:
1. Immune rejection: The transplanted tissue may be recognized as foreign by the patient's immune system, leading to an immune response that can damage the transplanted tissue and compromise the success of the transplant.
2. Infection: The surgery carries a risk of infection, which can lead to inflammation and scarring of the cornea and may require additional treatment.
3. Recurrence of the limbal stem cell deficiency: In some cases, the limbal stem cell deficiency may recur, even after a successful transplant.
4. Corneal melting: This rare complication occurs when the cornea becomes thin and weak and is at risk of collapsing. It can occur due to factors such as inflammation, infection, and environmental exposure.
5. Graft-versus-host disease: This rare complication can occur with allogeneic transplants and is caused by the donor's immune cells attacking the recipient's body.
6. Visual disturbances: The patient may experience visual disturbances, such as blurring or ghosting, as the eye heals.
7. Corneal scarring: The transplant may not successfully restore the cornea's clarity and may result in corneal scarring.
Post-Operative Recovery Process
The recovery process after a limbal stem cell transplant can vary depending on the individual's specific case, the type of transplant, and the severity of the deficiency. However, some general guidelines can help individuals understand what to expect during recovery.
Immediately after surgery, the patient must rest and avoid any activities that could pressure the eye, such as bending, lifting, or straining. The surgeon may prescribe eye drops or ointments to reduce inflammation, prevent infection, and promote healing.
In the first few weeks after the surgery, the patient will need to attend several follow-up appointments with their surgeon to monitor the transplant's progress and ensure no complications. During these appointments, the surgeon will examine the eye and may perform additional tests, such as corneal topography or optical coherence tomography, to evaluate the success of the transplant.
As the eye heals, the patient may experience some discomfort, such as mild pain or itching, and visual disturbances, such as blurring or ghosting. These symptoms are typical and should gradually improve over time.
The patient must take several precautions during recovery, such as avoiding activities that could damage the eye, such as rubbing or touching the eye or swimming. The surgeon may recommend wearing an eye patch or protective eyewear to prevent accidental injury to the eye.
The recovery time can vary depending on the type of transplant and the severity of the limbal stem cell deficiency. In general, the recovery period can take several weeks to several months, and the patient may need to take time off from work or other activities to allow for adequate rest and healing.
The patient will need to attend regular follow-up appointments with their surgeon for several months after the surgery to monitor the transplant's progress and ensure no complications. Over time, the patient can expect to see improvements in vision and the overall health of the cornea.
How Long Does It Take To See Improvement In Vision After A Limbal Stem Cell Transplant?
The timeline for improvement in vision after a limbal stem cell transplant can vary depending on the individual's specific case and the type of transplant. However, in general, the patient can expect to gradually see improvements in vision over several weeks to several months.
After the surgery, the patient's vision may be blurry or hazy due to the inflammation of the eye. It may take several weeks for the swelling to subside and for the eye to heal sufficiently for the patient to see improvement in vision. Additionally, the cornea may take time to regenerate and stabilize, affecting vision clarity.
In some cases, the patient may see improvement in vision within a few weeks of the surgery, mainly if the transplant was performed early in the course of the disease and the cornea is healthy. In other cases, it may take several months or longer for the patient to see significant improvement in vision.
The patient's visual acuity will be evaluated at each follow-up appointment with the surgeon, who will monitor the transplant's progress and ensure no complications. The surgeon may also recommend visual aids, such as glasses or contact lenses, to help the patient achieve optimal visual acuity.
It is important to note that the timeline for improvement in vision after a limbal stem cell transplant can vary depending on the individual's specific case and the severity of the deficiency. The patient should discuss their vision improvement expectations with their surgeon and understand that the recovery process can take time. With proper care and follow-up, most patients can expect significant vision and corneal health improvement over time.
Author: Dr. Muhammad Saad, Post Graduate Resident at Al-Shifa Trust Eye Hospital in Rawalpindi, Pakistan
(1).jpg)
.PNG)