Understanding Corneal Clouding: Causes, Symptoms, and Treatment
What Is Corneal Clouding?
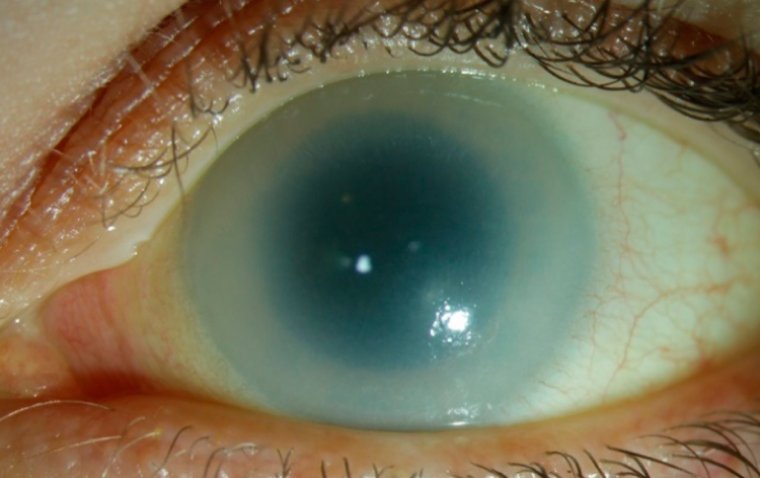
Corneal clouding, also known as corneal opacity, refers to a loss of transparency in the cornea, the clear front surface of the eye that allows light to enter and helps in focusing it onto the retina. A clear cornea is vital for vision, acting much like the lens of a camera, permitting light to pass through and facilitating the formation of a sharp image on the retina. Any opaqueness or clouding of the cornea can disrupt this delicate process.
When the cornea becomes clouded, it scatters or blocks light entering the eye, leading to a range of visual problems. These can vary from mild blurriness and vision distortion to severe impairment, potentially culminating in blindness depending on the extent of the clouding. The condition hence underscores the importance of maintaining corneal health for optimal vision.
Corneal Clouding vs. Cataracts
Corneal clouding and cataracts are both ocular conditions that can impact vision, but they affect different parts of the eye and have distinct causes, symptoms, and treatment options.
Corneal Clouding: This condition involves the loss of transparency in the cornea, the clear, front part of the eye that helps focus light onto the retina. Corneal clouding can be congenital or acquired due to injuries, infections, or other eye diseases. It interferes with the passage of light through the cornea, leading to blurry vision or even blindness in severe cases.
Cataracts: Cataracts, on the other hand, are a clouding of the eye's natural lens, which is located behind the iris and the pupil. Unlike the cornea, which is at the front of the eye, the lens is further back and plays a role in focusing light onto the retina. Cataracts are most commonly associated with aging but can also be caused by trauma, medications, or other health conditions like diabetes. They usually develop slowly and can affect one or both eyes.
Key Differences:
● Location: Corneal clouding affects the cornea, while cataracts affect the lens.
● Causes: Corneal clouding can be due to a variety of factors including congenital issues, injuries, and diseases. Cataracts are commonly age-related but can also be induced by other factors like medications or trauma.
● Symptoms: Both conditions lead to impaired vision, but the specific visual difficulties may differ.
● Treatment: Corneal clouding may require surgical intervention like corneal transplantation, while cataracts are typically treated through a surgical procedure that replaces the clouded lens with an artificial one.
What Causes Corneal Clouding?
Corneal clouding, or corneal opacity, can arise from a variety of sources, ranging from congenital conditions to acquired diseases and injuries. Understanding these underlying causes is critical for prevention and treatment. Here, we delve into common corneal clouding causes and associated risk factors.
1. Genetic Factors: Some individuals are born with corneal clouding as a result of genetic disorders. Conditions like congenital glaucoma or inherited metabolic disorders can lead to cloudiness in the cornea from birth.
2. Eye Injuries: Trauma to the eye, such as scratches, burns, or punctures, can damage the cornea and lead to clouding. Severe infections after eye surgeries could also lead to this condition.
3. Medical Conditions: Diseases like keratitis (inflammation of the cornea), uveitis (inflammation of the middle layer of the eye), and Fuchs' dystrophy (a degenerative condition affecting the cornea's endothelial cells) can cause corneal clouding.
4. Use of Certain Medications: Topical or systemic medications like corticosteroids could contribute to corneal changes when used inappropriately or for extended periods.
5. Age: While less common than age-related cataracts, the likelihood of developing corneal clouding can increase with age due to the gradual loss of corneal cells and other degenerative changes.
Risk Factors
Some of the risk factors that may make you more susceptible to corneal clouding include:
● Pre-existing eye conditions: Having conditions like glaucoma or chronic eye inflammation increases the risk.
● Environmental factors: Exposure to harmful chemicals, smoke, or excessive UV radiation.
● Poor contact lens hygiene: Improper cleaning or overuse of contact lenses can increase the risk of infections leading to cloudiness.
● Systemic diseases: Conditions like diabetes can indirectly influence eye health, including the cornea.
Symptoms and Diagnosis of Corneal Clouding
When it comes to understanding corneal clouding symptoms and their diagnosis, early identification is key for effective management and treatment. Below are some of the signs to look out for, as well as how medical professionals go about diagnosing this eye condition.

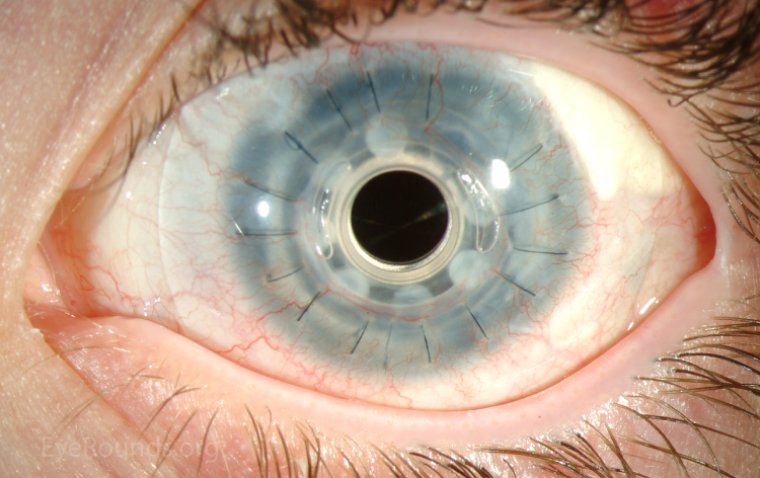
Credit: Research Gate
Common symptoms of corneal clouding include:
● Blurred Vision: One of the earliest signs is a gradual or sudden blurring of vision, making it difficult to focus on objects.
● Glare Sensitivity: Individuals may find it challenging to tolerate bright lights and may experience glare, particularly at night.
● Reduced Visual Acuity: A decline in the clarity or sharpness of vision can be a telling sign.
● Halos around Lights: Some people report seeing halos or rings around lights, especially in darker settings.
● Discomfort or Pain: Though less common, some may experience a sense of discomfort or even pain in the eye.
● Foreign Body Sensation: A feeling as if something is stuck in the eye, even when there is nothing there.
Diagnosis
Medical professionals utilize a variety of tools and tests to diagnose corneal clouding:
1. Comprehensive Eye Examination: An ophthalmologist will conduct a thorough eye exam, which may include a visual acuity test to measure the sharpness of your vision.
2. Slit-Lamp Examination: This test allows the doctor to take a closer look at the different layers of the eye, including the cornea, by using a specialized microscope.
3. Corneal Topography: This imaging test maps out the cornea's surface, providing a detailed view that helps in the diagnosis.
4. Optical Coherence Tomography (OCT): A non-invasive imaging test that produces detailed images of the eye, helping to identify any changes in the corneal layers.
Treatment Options for Corneal Clouding
Recognizing the signs and symptoms of corneal clouding can lead to early intervention, which is crucial for effective management of the condition. Let's explore the various corneal clouding treatment options, from medications to surgical interventions.
Medications
● Eye drops: Doctors may prescribe medicated eye drops that aim to reduce inflammation or infection, depending on the underlying cause of the clouding.
● Antibiotics: If the clouding is due to an infection, antibiotic eye drops or ointments may be recommended.
● Anti-inflammatory drugs: Corticosteroid eye drops may be used to control inflammation, particularly in cases related to injury or surgery.
Surgical Procedures
● Phototherapeutic Keratectomy (PTK): This laser surgery removes surface corneal scars and may be an option for some patients.
● Lamellar Keratoplasty: This involves replacing only the diseased layers of the cornea, preserving the healthy layers.
Corneal Transplantation
● Penetrating Keratoplasty: Also known as full-thickness corneal transplantation, this procedure replaces the entire cornea with a healthy donor cornea.
● Descemet's Stripping Automated Endothelial Keratoplasty (DSAEK): This is a partial-thickness corneal transplant that replaces only the back layers of the cornea.
Surgery for corneal clouding often becomes the go-to option when medications are ineffective or when vision loss is significant.
How to Prevent Corneal Clouding
Taking precautionary measures is essential for safeguarding your eyes from corneal clouding. Being proactive about eye health can significantly reduce the risk of developing this condition. Here are some preventive strategies that can be instrumental:
● Sports Safety: Always wear protective eyewear while playing high-impact sports or participating in activities that pose a risk of eye injury.
● Workplace Safety: If you work in an environment where airborne particles, chemicals, or intense light is present, appropriate eye protection, like safety goggles, is a must.
● Early Detection: Regular eye examinations allow healthcare professionals to detect signs of corneal clouding early, improving the chances for successful treatment.
● Monitor Changes: Regular check-ups can track changes in your vision and eye health, serving as an early warning system for conditions like corneal clouding.
● No Smoking: Smoking increases the risk of various eye conditions, including corneal clouding. Quitting smoking can be one of the best ways to protect your eyes.
● UV Protection: Always wear sunglasses that provide 100% protection from harmful UV rays to minimize the risk of eye damage.
● Balanced Diet: Eating a diet rich in vitamins and antioxidants can help maintain eye health.
● Stay Hydrated: Keeping well-hydrated can also benefit the eyes, as dehydration can worsen dry eyes, a contributing factor to corneal issues.
Summary
Corneal clouding is a serious eye condition that affects vision by obstructing the clarity of the cornea, the eye's front surface. The causes can be varied, ranging from genetic predispositions and eye injuries to underlying medical conditions. Symptoms commonly include blurred vision and an increased sensitivity to glare.
Diagnosing corneal clouding early is crucial for effective treatment. This is achieved through comprehensive eye examinations and imaging techniques by healthcare professionals. Various treatment options exist, from medications to surgical procedures like corneal transplantation, emphasizing the importance of early intervention for optimal outcomes.
Prevention is an integral part of managing the risk of developing corneal clouding. Simple measures such as eye protection during high-risk activities, regular eye check-ups, and lifestyle changes can go a long way in maintaining eye health.
If you suspect you are experiencing symptoms of corneal clouding, it is imperative to consult a medical professional for an accurate diagnosis and appropriate treatment plan. Your eyes are your windows to the world; take proactive steps to keep them clear and healthy.
(1).jpg)