2025 Recap: Top 10 Breakthroughs in Ophthalmology Research
Ophthalmology research in 2025 was defined by significant progress in regenerative medicine, drug delivery innovation, gene therapy, and vision restoration technologies. Scientists advanced the frontiers of retinal regeneration, stem cell therapy, long-acting glaucoma treatments, and device-based interventions for age-related vision loss. From laboratory discoveries to first-in-human trials, these developments are laying the foundation for more durable, accessible, and transformative eye care solutions.
Ophthalmology Breaking News has selected 10 standout breakthroughs that reflect this year’s most impactful scientific and clinical milestones.
1. Vision Restoration Breakthrough: Retinal Therapy Achieves First Long-Term Neural Regeneration
In a major advancement for regenerative ophthalmology, researchers at KAIST, in collaboration with Celliaz Inc., have achieved the first long-term neural regeneration in mammalian retinas. The study, published in Nature Communications, demonstrated that blocking the protein PROX1 enabled the regeneration of retinal neurons in disease-model mice, leading to sustained vision restoration for over six months. This breakthrough addresses a significant unmet need, as current therapies only slow retinal degeneration but do not reverse damage. By identifying PROX1 as a key barrier to retinal repair, the researchers developed a novel antibody therapy to neutralize its effects, unlocking the regenerative potential of Müller glia cells.
The antibody, developed by Celliaz Inc. and known as CLZ001, successfully triggered retinal neuron regeneration and vision recovery in both acquired and congenital retinal degeneration models. Delivered via injection or gene therapy, the treatment restored retinal function with long-lasting results. Celliaz Inc. is now optimizing the therapy and preparing for clinical trials by 2028, targeting patients with currently untreatable forms of retinal disease. If successful in human studies, this approach could revolutionize treatment for millions at risk of blindness, offering hope where none previously existed.
2. New Drug Delivery Method Shows Promise for Long-Lasting Glaucoma Relief
Researchers at the University of Toronto have developed a novel, non-invasive drug delivery system that could transform glaucoma management by replacing daily eye drops with a single injection lasting up to seven weeks. Published in Advanced Materials, the study highlights the use of colloidal drug aggregates (CDAs), self-assembling nano-particles, combined with a hydrogel to deliver the glaucoma drug timolol in a slow-release formulation. Injected into the subconjunctival space beneath the eyelid, this method showed a 200-fold increase in efficacy compared to traditional eye drops and successfully maintained drug presence without leakage. The innovation addresses common issues in glaucoma care, including poor patient adherence and the risks associated with more invasive procedures.
Led by Professor Molly Shoichet and supported by Dr. Jeremy Sivak, the team’s work demonstrates the potential for safer, longer-lasting glaucoma treatment with fewer complications. The researchers are now optimizing drug formulation for clinical trials, focusing on stability, manufacturability, and regulatory readiness. Their goal is to introduce a monthly or bi-monthly outpatient injection to improve patient outcomes and adherence. This new approach, if successful in human trials, could significantly reduce the treatment burden for millions of glaucoma patients worldwide.
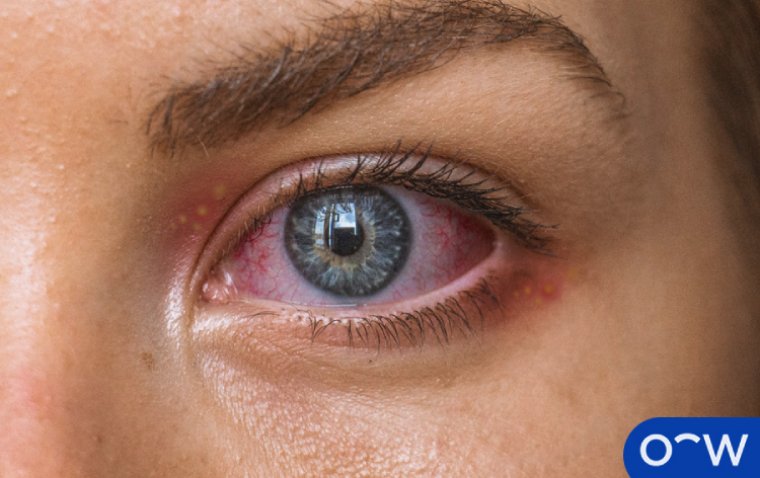
3. Stem Cell Transplant Shows Safety Promise for Wet AMD Treatment
A clinical study published in Stem Cell Reports offers promising early evidence that stem cell transplantation could be a safe and effective treatment for advanced wet age-related macular degeneration (AMD), a leading cause of blindness. Researchers from Third Military Medical University Southwest Hospital in China evaluated a two-step treatment in 10 patients: surgical removal of abnormal blood vessels in the macula followed by transplantation of stem cell-derived retinal cells. The study found that patients who received complete removal of vascular lesions showed improved retinal structure and stable or improved vision over a 12-month period, with minimal side effects.
Conversely, patients who underwent only partial removal of the lesions experienced ongoing inflammation, bleeding, and no significant visual improvement, highlighting the importance of full lesion removal for successful transplant outcomes. While the findings mark a step forward in retinal repair for wet AMD, the authors emphasize the need for larger studies to assess long-term safety and refine surgical techniques. If validated in broader trials, this combined surgical, and stem cell-based approach could provide new hope for patients with late-stage wet AMD who do not respond to conventional treatments like anti-VEGF therapy.
4. Researchers Develop Pig Retinal Cells to Advance Eye Treatments
Researchers at the University of Wisconsin–Madison, in collaboration with the Morgridge Institute for Research, have successfully developed pig retinal organoids, 3D tissue structures that mimic the retina. This advancement, published in Stem Cell Reports, provides a crucial model for testing stem cell therapies aimed at restoring vision in degenerative eye diseases. The challenge in the field has been the immune incompatibility of human cells in animal models. Since pig and human retinas share many similarities, scientists believe these pig-derived retinal organoids offer a promising solution for evaluating the safety and effectiveness of lab-grown photoreceptors before human trials.
To create the pig retinal organoids, researchers used pluripotent stem cells and adapted protocols originally developed for human cells to align with pigs’ faster developmental timelines. The organoids were validated using advanced techniques such as immunocytochemistry and single-cell RNA sequencing, which confirmed the presence of key retinal cell types. Moving forward, the team plans to transplant pig photoreceptors into pig retinas to test integration and function. This breakthrough represents a major step toward developing stem cell-based treatments for vision loss and could accelerate preclinical testing for a range of retinal diseases.
5. NIH Researchers Demonstrate Promise of PEDF-Based Eye Drops for Inherited Retinal Diseases
Researchers at the National Eye Institute (NEI), part of the NIH, have developed experimental eye drops containing fragments of pigment epithelium-derived factor (PEDF), a natural retinal protein, to slow retinal degeneration. Published in Communications Medicine, the study shows that two peptide variants, 17-mer and H105A, can penetrate ocular tissues and protect photoreceptors in animal models of retinitis pigmentosa (RP) without toxicity. Notably, H105A preserved up to 75% of photoreceptors and retinal responsiveness, suggesting the drops could extend the treatment window for gene therapy in conditions like RP and dry AMD.
In further experiments, peptide-pretreated animals responded well to gene therapy, maintaining vision for at least six months. Human-derived retinal tissue exposed to the peptides also showed resilience under stress, indicating strong translational potential. While not a cure, these PEDF-based drops represent a promising non-invasive therapeutic strategy for inherited retinal diseases. Human clinical trials are anticipated, as researchers aim to offer a broadly accessible, vision-preserving option for patients with limited treatment alternatives.
6. Human Retinal Stem-Like Cells Discovered with Potential to Repair Vision Loss
A team led by Wenzhou Medical University has discovered a unique population of human neural retinal stem-like cells with the potential to regenerate damaged retinal tissue, offering new hope for treating retinal degenerative diseases like retinitis pigmentosa and age-related macular degeneration (AMD). Using single-cell and spatial transcriptomics on human fetal retinal tissue, researchers identified these cells in the ciliary marginal zone and confirmed their presence in retinal organoids. The cells exhibited markers of self-renewal and the ability to differentiate into key retinal cell types, such as photoreceptors and ganglion cells.
Functionally, these stem-like cells migrated to injured areas in retinal organoids and successfully regenerated retinal tissue in mouse models of inherited degeneration. Transplanted cells survived for up to 24 weeks, integrated with host retinal structures, formed synapses, and improved both structure and vision, without causing tumors. These findings suggest that retinal organoids could become a scalable source for regenerative therapies. While further research is needed to ensure safety and immune compatibility, this breakthrough lays the groundwork for future stem cell-based treatments aimed at restoring vision.
7. Gene Therapy Reduces Eye Pressure in Mice, Offers Potential Alternative to Glaucoma Drops
A study published in PNAS Nexus highlights a promising gene therapy approach that could offer glaucoma patients a long-lasting, reversible alternative to daily eye drops. Using the CRISPR-Cas13d system, researchers led by Dr. Yang Sun targeted the mRNAs of Aquaporin 1 and Carbonic anhydrase type 2, genes involved in fluid production in the eye, to reduce intraocular pressure (IOP) in mice. Unlike conventional gene editing, this RNA-targeting method does not permanently alter DNA, allowing for adjustable treatment with fewer side effects than traditional glaucoma medications.
In treated mice, both wild-type and glaucoma models experienced significantly reduced IOP, demonstrating the potential efficacy of this technique. The therapy, localized to the ciliary body, may only require monthly or less frequent administration, addressing the common issue of poor adherence to daily eye drops. Although more research is needed, including optimization, safety testing, and human trials, this approach could significantly improve long-term glaucoma management and reduce the risk of vision loss for millions globally.
8. Snails Offer New Model for Eye Regeneration Research
Researchers at the Stowers Institute for Medical Research have identified the apple snail (Pomacea canaliculata) as a powerful new model for studying eye regeneration. Unlike humans, these snails can fully regenerate their complex, camera-type eyes, including the lens, cornea, and retina, after severe injury or even full amputation. The study, published in Nature Communications, outlines a four-stage regenerative process completed in just 28 days. Led by Dr. Alejandro Sánchez Alvarado and Dr. Alice Accorsi, the team also developed genetic tools for the snail model, enabling precise gene function studies using CRISPR technology.
A breakthrough was the confirmation of the pax6 gene’s critical role in eye development, as disrupting it resulted in eyeless snail embryos. This positions apple snails as a unique model that combines regenerative ability with genetic accessibility, allowing researchers to map and manipulate genes involved in sensory organ repair. The work opens new possibilities for understanding how complex organs like eyes can regenerate, potentially advancing future therapies for human vision loss conditions such as macular degeneration.
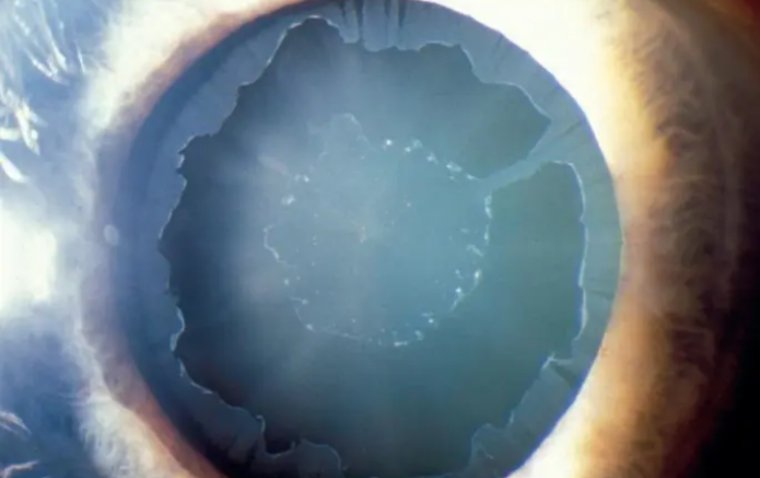
9. mRNA Vaccine Demonstrates Potential to Treat Age-Related Macular Degeneration
Researchers in Japan have developed an innovative mRNA vaccine that targets abnormal blood vessel growth in the retina, offering a potential new treatment for wet age-related macular degeneration (AMD). Unlike current anti-VEGF therapies that require frequent intravitreal injections, this vaccine is delivered intramuscularly and works by inducing antibodies against LRG1, a protein linked to angiogenesis in AMD. In preclinical mouse models, the vaccine reduced retinal leakage and lesion size by up to 85% and 82%, respectively, showing comparable efficacy to existing anti-VEGF treatments while avoiding invasive eye procedures.
The vaccine demonstrated strong antibody responses, a favorable safety profile, and did not interfere with normal retinal or vascular function. Researchers from the Institute of Science Tokyo and Yokohama City University suggest this approach could provide long-term protection with fewer doses, significantly reducing treatment burden. Inspired by the success of mRNA technology in COVID-19 vaccines, this study marks a promising step toward applying mRNA platforms to chronic eye diseases, potentially revolutionizing care for millions with neovascular AMD.
10. Retinal Implant Restores Central Vision in Advanced AMD
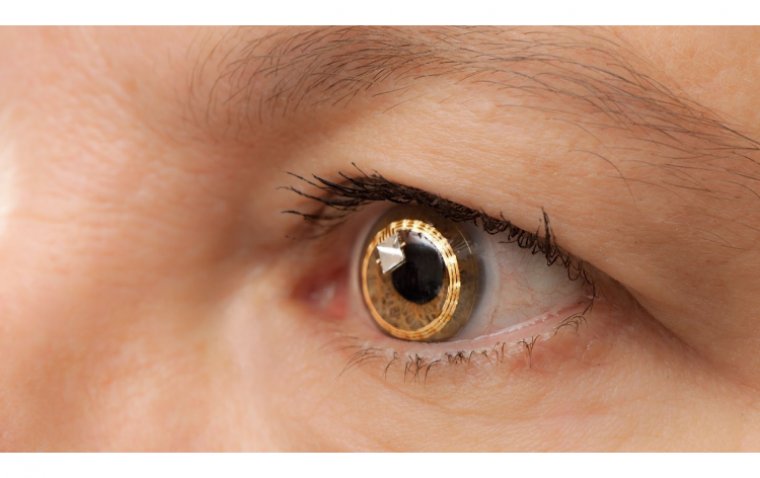
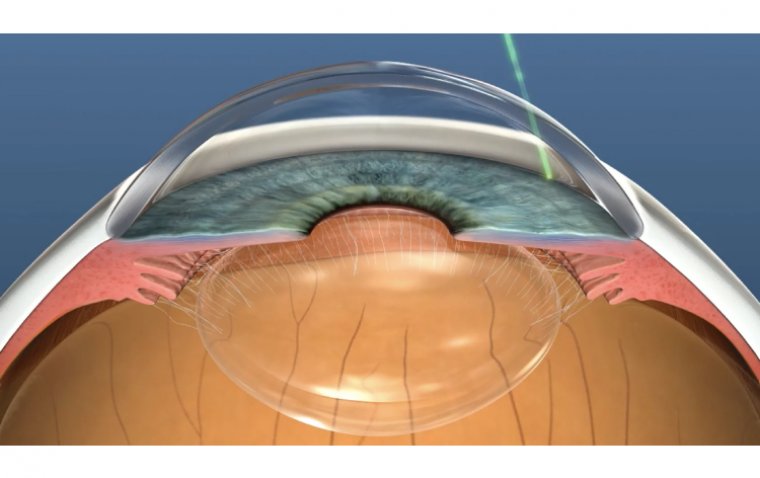
An international clinical trial known as PRIMAvera has demonstrated that a wireless retinal implant can restore central vision in patients with advanced age-related macular degeneration (AMD), specifically those with geographic atrophy (GA). The study, published in the New England Journal of Medicine and co-led by researchers from UPMC, Stanford University, and the University of Bonn, showed that 26 out of 32 participants experienced clinically meaningful improvements in visual acuity, with 81% gaining 10 or more letters on an eye chart. One participant even gained 59 letters. Most users were able to read letters, numbers, and in some cases, full pages at home using the system.
The PRIMA system includes a 2×2 mm wireless micro-implant that replaces damaged photoreceptors by converting light captured by a camera (mounted on specialized glasses) into electrical signals sent to the brain. The implant is activated by near-infrared light and allows patients to adjust visual settings like contrast and zoom. The PRIMAvera trial enrolled 38 participants across five European countries and showed the device was well-tolerated with no unresolved adverse events. Following these promising results, Science Corporation, the implant's manufacturer, has submitted the device for regulatory approval in both the U.S. and Europe, potentially ushering in a new era of vision restoration for AMD patients.
Looking Ahead: From Possibility to Progress
This year’s breakthroughs underscore the momentum in restorative and long-acting ophthalmic treatments, from regenerative biology and gene editing to device-driven and mRNA-based therapies. As these discoveries transition into clinical stages, they bring renewed hope for millions living with vision impairment and blindness.
2026 is poised to build on this momentum, with several of these innovations expected to enter human trials and expand global research efforts.
(1).jpg)