mRNA Vaccine Demonstrates Potential to Treat Age-Related Macular Degeneration in Preclinical Study
Researchers in Japan have developed a novel mRNA vaccine that, when delivered via intramuscular injection, significantly suppresses abnormal blood vessel growth in the retina, a key factor in wet age-related macular degeneration (AMD). In preclinical mouse models, the vaccine was found to be as effective as current anti-VEGF therapies, with the added benefit of avoiding repeated intravitreal injections. These findings offer promising potential for a less invasive, long-term treatment approach for AMD and other neovascular eye conditions.
AMD and Neovascularization: A Leading Cause of Vision Loss
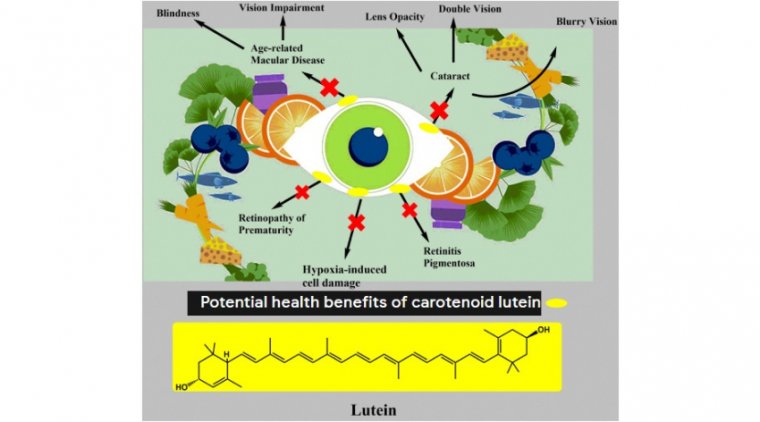
Age-related macular degeneration (AMD) is a leading cause of vision loss in people over the age of 60, affecting approximately 200 million individuals worldwide. In its wet form, the disease is characterized by neovascularization, or the growth of abnormal blood vessels beneath the retina. These vessels often leak fluid, leading to retinal damage and progressive vision loss.
Currently, the standard of care involves repeated intraocular injections of anti-angiogenic drugs, such as anti-VEGF therapies, which help slow the development of these vessels. However, frequent eye injections are burdensome, and some patients eventually become non-responsive to treatment.
A New Approach: mRNA-Based Treatment for Retinal Disease
Researchers at the Institute of Science Tokyo (Science Tokyo) and Yokohama City University have developed an mRNA vaccine that offers a systemic, intramuscular alternative to current eye injections. The team was led by Professor Satoshi Uchida (Department of Advanced Nanomedical Engineering, Science Tokyo) and Visiting Professor Yasuo Yanagi (Department of Ophthalmology and Micro-technology, Yokohama City University). Their findings were published in the journal Vaccine.
The vaccine delivers mRNA encoding leucine-rich alpha-2-glycoprotein 1 (LRG1), a protein known to promote angiogenesis and found in elevated levels in AMD patients. By stimulating the body to produce antibodies that inhibit LRG1, the vaccine prevents pathological blood vessel growth in the retina.
Preclinical Results Show Strong Efficacy in Mouse Models
The research team tested the mRNA vaccine in two mouse models of choroidal neovascularization (CNV): one induced by laser and one that naturally develops CNV. Mice received two intramuscular doses of the vaccine, administered 14 days apart.
Key results include:
• In the laser-induced CNV model, by day 21:
• 85% reduction in leakage
• 82% reduction in lesion size
• In the naturally occurring CNV model, by day 28:
• 55% reduction in lesion size
The vaccine produced a robust antibody response within one week of the first dose and was comparable in effect to standard anti-VEGF antibody therapy.
Safety Profile and Potential Advantages Over Current Treatments
The mRNA vaccine demonstrated a favorable safety profile in preclinical testing. It did not disrupt normal blood vessel formation, damage healthy retinal tissue, or cause adverse immune responses in other organs.
Importantly, unlike current anti-VEGF treatments that require frequent intravitreal injections, the mRNA vaccine could potentially offer long-lasting effects through a single intramuscular dose, reducing the treatment burden for patients.
“The effects of LRG1 mRNA vaccination on reducing endothelial and microglial cells were comparable to those of anti-VEGF antibody therapy,” noted Prof. Uchida. “Unlike conventional treatments requiring repeated intravitreal injections, this vaccine may provide long-term benefits with a single intramuscular dose.”
Expanding mRNA Applications Beyond Infectious Diseases
The development of this vaccine is inspired by the success of mRNA technologies during the COVID-19 pandemic. As Professor Uchida explained:
“The COVID-19 pandemic highlighted the remarkable potential of mRNA as a vaccine platform. Inspired by those successes, we sought to expand its use beyond infectious diseases and cancer to chronic eye conditions. To our knowledge, this is the first study to show that an mRNA vaccine can suppress pathological neovascularization in animal models.”
Reference:
Yasuo Yanagi et al, mRNA vaccination mitigates pathological retinochoroidal neovascularization in animal models, Vaccine (2025). DOI: 10.1016/j.vaccine.2025.127451
(1).jpg)