Genetic Research Offers New Hope for Patients with Inherited Retinal Diseases
Researchers at the University of Oklahoma are advancing the understanding of inherited retinal diseases (IRDs) through genetic mapping that may lead to more accurate diagnoses and lay the groundwork for future treatments. A study, published in the journal Genes, is led by Lea D. Bennett, PhD, Assistant Professor of Ophthalmology at the University of Oklahoma College of Medicine.
The Diagnostic Challenge of IRDs
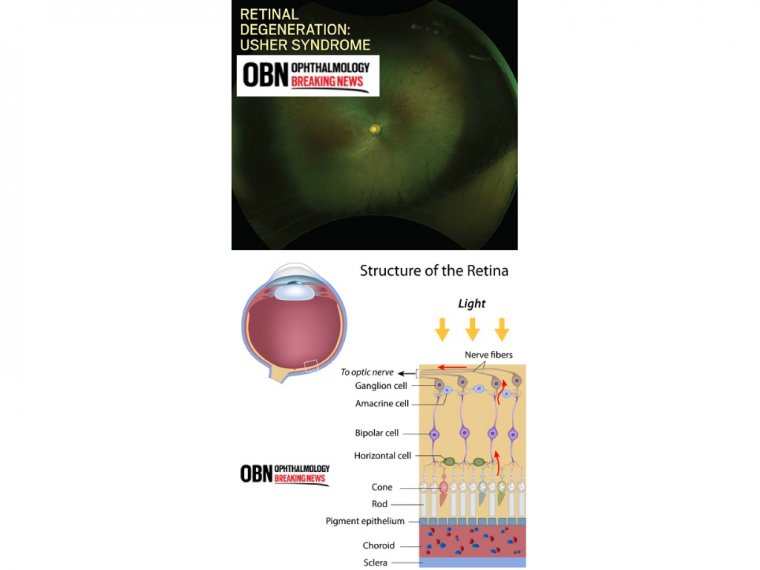
Inherited retinal diseases are a diverse group of genetic disorders that affect the light-sensitive tissue in the retina, causing progressive vision loss and retinal degeneration. Despite impacting approximately 1 in 3,000 people worldwide, clinical diagnosis of IRDs remains difficult due to the overlapping symptoms across different genetic conditions.
“These results clarify and confirm clinical diagnoses, aid in counseling patients on prognosis and family planning, and guide treatment options,” said Dr. Bennett.
“This study not only holds promise for affected individuals but also expands the mutation spectrum to guide understanding of IRDs.”
Mapping the Genetics Behind Vision Loss
Bennett’s research team at the Dean McGee Eye Institute analyzed genetic samples from 103 unrelated IRD patients, with testing supported by the Foundation Fighting Blindness, a Maryland-based nonprofit. The goal was to identify mutations that could explain the patients' clinical symptoms and improve diagnostic certainty.
Key Findings:
• Mutations identified in 70 out of 103 samples
• 20 previously unreported genetic variants discovered
• Conditions linked to these findings included:
• Retinitis pigmentosa
• Cone-rod dystrophy
• Macular diseases
• Third-branch disorders
• The most frequently mutated gene was ABCA4
• New mutations were confirmed in ALMS1, GNAT1, RAX2, and RDH5
The Genetic Mystery in Negative Cases
Despite clinical diagnoses, 33 of the 103 patients showed no detectable genetic mutations. Researchers examined variables such as family history and age of disease onset to explain these discrepancies. Notably, 28 of these 33 patients reported no known family history of IRDs.
Dr. Bennett explained that undiagnosed genetic factors or mimicking conditions might be responsible:
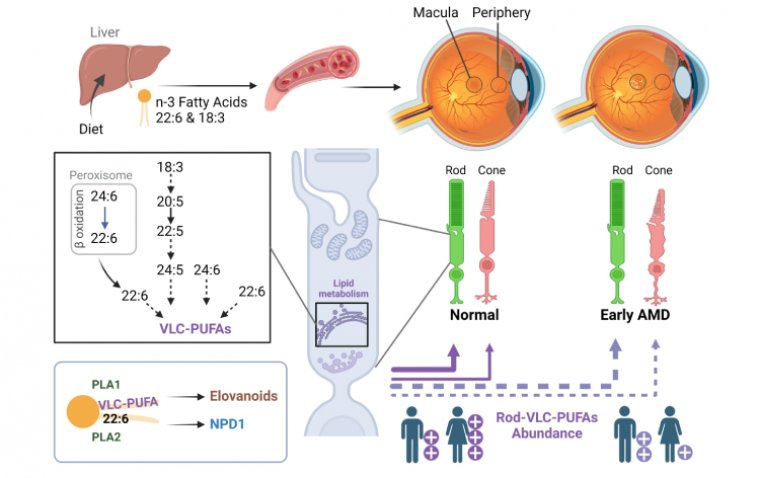
“There’s so much about hereditary retinal diseases that we don’t know. The first step in developing new therapies for IRDs is to map the genetic mutations that trigger them.”
Clinical Relevance and Broader Impact
Currently, Luxturna is the only FDA-approved gene therapy for IRDs. Dr. Bennett hopes her research will support the discovery of additional therapies and help identify patients for future clinical trials.
Bennett’s work has already led to significant findings. In 2018 and 2019, she uncovered a cluster of macular degeneration patients who tested negative for genetic mutations. All were taking Elmiron, a medication for interstitial cystitis, which has since been associated with retinal toxicity. Early intervention, including changing medications, prevented further vision damage in these cases.
This discovery further motivated Bennett to pursue comprehensive genetic studies and expand her IRD research portfolio.
Looking Ahead: From Diagnosis to Therapy
At the Dean McGee Eye Institute, Bennett is also coordinating participation in an international Phase 3 clinical trial for retinitis pigmentosa, further contributing to the search for viable treatments.
“I do this for my patients—to give them information, to give them an accurate diagnosis, and to give them hope,” Bennett said.
“That’s my entire purpose.”
Reference:
Jacob Lynn et al, Expanding the Mutation Spectrum for Inherited Retinal Diseases, Genes (2024). DOI: 10.3390/genes16010032
(1).jpg)