History of Cataract Surgery
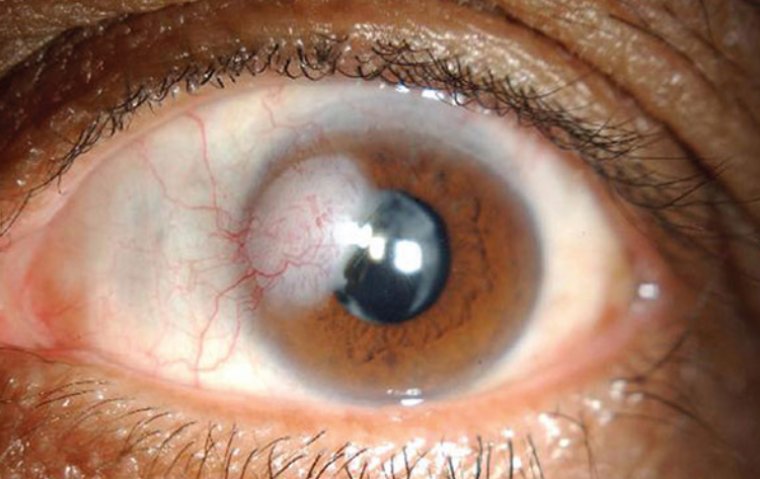
A cataract is a pathologic condition in which the eye's lens opacifies, resulting in changes to vision that can range from color changes and blurriness to halos around lights and, in the worst case scenario, blindness. A senile cataract, in which the clouding of the lens is brought on by aging, is the most prevalent cause of cataract development, however there are numerous other risk factors as well.
It is therefore not unexpected that cataracts, which affected over 20 million people globally in 2010 and are expected to continue to rise in incidence, are the primary cause of blindness globally. The name "cataract" comes from the Latin word "cataracta," which means waterfall. This may be because, until the 1700s, some people believed that cataracts were created by opaque liquid material streaming through the lens. Alternatively, it could be because a dense cataract could occasionally appear to be a waterfall to an untrained eye.
Cataract surgery has a rich history marked by continuous advancements in techniques and technologies. Alongside advancements in cataract surgical techniques have been improvements in intraocular lens replacement technology. Cataract surgery may be considered among the most successful treatments in all of medicine. When a cataract becomes visually significant, cataract surgery is the only established method of treatment. The definition of “visually significant” has evolved over time, to its current meaning of a visual acuity of 20/40 or worse.
This article delves into the evolution of cataract surgery, from its early days to the modern procedures that have revolutionized ophthalmology.
Previous Surgical Methods
In the early stages of cataract treatment, surgical interventions were rudimentary compared to today's sophisticated procedures. Exploring the historical context is crucial to understanding the leaps made in the field.
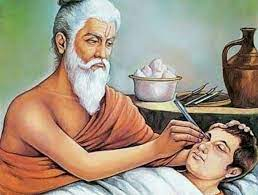
Couching
Couching stands as a historic surgical method in the annals of cataract surgery, dating back centuries. Originating in ancient civilizations, this technique involved displacing the clouded lens rather than removing it, reflecting the limited understanding and tools available at the time. During couching, a blunt instrument, often a thin needle or spatula, was used to push the cataractous lens to the bottom of the eye, away from the visual axis.
Historical accounts, including those found in the "Canon of Medicine" by Avicenna, suggest that couching was practiced as early as the 10th century. While it provided a rudimentary improvement in visual acuity for some patients, the procedure had inherent risks, such as secondary glaucoma and inflammation. As cataract surgery progressed over time, moving from couching to more refined techniques like extracapsular cataract extraction (ECCE), the field saw a marked enhancement in both safety and efficacy.
The transition from couching to modern cataract surgery represents a significant milestone, highlighting the iterative process of medical advancement and the continuous pursuit of improved patient outcomes. Today, with sophisticated surgical methods and technological innovations, cataract surgery has become a highly precise and well-tolerated procedure, vastly different from the historical practices of couching.
Extracapsular Cataract Extraction
Extracapsular cataract extraction (ECCE) played a pivotal role in the history of cataract surgery. Developed as a significant improvement over earlier methods, ECCE involved removing the cataract while leaving the lens capsule partially intact.
Extracapsular cataract extraction (ECCE) emerged as a breakthrough in cataract surgery, marking a departure from older, less precise methods. This technique allowed surgeons to carefully extract the cloudy lens, leaving the posterior capsule relatively intact. Though a significant step forward, ECCE had limitations, prompting further advancements in the quest for improved outcomes.
Intracapsular Cataract Extraction
Intracapsular cataract extraction (ICCE) represents an earlier approach where the entire lens, including its surrounding capsule, was removed. While an important milestone, ICCE eventually gave way to more refined techniques.
Intracapsular cataract extraction (ICCE) was an early method where surgeons removed the entire lens along with the surrounding capsule. Despite being a notable advancement at the time, ICCE had drawbacks, including increased risk and complications. As technology progressed, this approach evolved, leading to the development of extracapsular cataract extraction (ECCE) and, eventually, the modern era of cataract surgery.
Intraocular Lenses
The introduction of intraocular lenses (IOLs) was a transformative moment in cataract surgery, addressing issues associated with previous methods and significantly improving patients' visual outcomes.
Intraocular lenses (IOLs) revolutionized cataract surgery by offering a permanent replacement for the removed natural lens. These artificial lenses allowed for clearer vision and reduced reliance on cumbersome post-surgery aids. Over the years, IOL technology has evolved, providing patients with a range of options, including multifocal and toric lenses, catering to individual visual needs.
The Last 70 Years
Sir Harold Ridley implanted the first IOL on February 8, 1950. Charlie Kelman’s US Patent for phacoemulsification was filed July 25, 1967. Following the introduction of these foundational elements of modern cataract surgery, myriad incremental innovations have brought about what is surely the fastest, safest, and most effective surgical procedure in the world today.
These innovations include reducing the size and therefore the morbidity related to incisions, increasing the efficiency of lens extraction by optimizing the energy required to break up and evacuate the lens, and improving the accuracy of intraocular lens power calculations to refine postoperative refractive outcomes.
The development of adjunctive tools and tricks to alleviate the negative impact of preexisting risk factors such as a small pupil or a weakened zonule has improved the safety of surgery, while the introduction of the femtosecond laser has created a new opportunity for innovation and precision in the treatment of astigmatism.
All of these advances have combined to make a big “wow” for our patients. Clinical research has also produced important advances in our knowledge of cataract surgery. One of the most significant findings of recent studies of minimally invasive glaucoma surgery is confirmation of the substantial reduction of intraocular pressure in patients with mild to moderate glaucoma from cataract surgery alone.
Investigational device exemption randomized clinical trials of both the CyPass and the Hydrus demonstrated a remarkable concordance in terms of the proportions of subject eyes in the control groups with unmedicated mean diurnal IOP reductions greater than or equal to 20% from baseline (57.8% compared with 58.0%) and the reductions in the control groups in unmedicated mean diurnal IOP from baseline (both -5.3 mmHg).
These clinically significant reductions in IOP in glaucoma patients having cataract surgery alone have now been demonstrated by randomized, controlled clinical trials which provide the highest standard of evidence for this phenomenon.
Nevertheless, challenges remain to provoke the imagination of scientists and entrepreneurs as global demographics predict an increasing demand for cataract surgery. For example, cystoid macular edema, or Irvine-Gass Syndrome, remains the most common complication associated with routine cataract surgery and can occur in patients with or without risk factors, such as diabetes or pre-existing macular disease.
While topical anti-inflammatory agents are considered prophylactic in the perioperative period, the use of intravitreal anti-VEGF agents as treatment has garnered support. This unpredictable and potentially sight-threatening complication deserves attention.
Another example of an unpredictable complication, capsule contraction syndrome, is related to fibrous metaplasia of lens epithelial cells similar to the pathogenesis of posterior capsular opacification and usually occurs within the first 3 months following surgery.
Changes in refraction may occur due to axial displacement or tilting of the IOL due to the capsular contraction. Capsule contraction syndrome “has occurred in eyes with and without risk factors after the implantation of every IOL type (PMMA, silicone and acrylic).”
Identified risk factors include small capsulorhexis diameter, postoperative inflammation, pseudoexfoliation syndrome, uveitis, retinitis pigmentosa, history of retinal surgery, myotonic dystrophy and diabetes.
Treatment of capsular contraction syndrome has relied primarily on Nd:YAG laser relaxing anterior capsulotomies to eliminate constriction. Radial capsulotomies “can significantly enlarge the anterior capsule opening” but “the IOL can remain decentered and folded within the capsular bag, especially in case of shrinkage or thick fibrous anterior membrane. ”
Femtosecond laser capsulotomies have advantages in terms of precision, and, despite difficulty cutting thickened capsular tissue, are easier and safer than previous techniques.
The lesson of IOL development is that innovation is not for the weak of heart. Early phaco, just as much as early IOLs, did damage many eyes. Nevertheless, perseverance had great rewards, and it will no doubt continue to do so as we invent the next generation of cataract surgery innovations. Early phaco, just as much as early IOLs, did damage many eyes. Nevertheless, perseverance had great rewards.
Modern Cataract Surgery
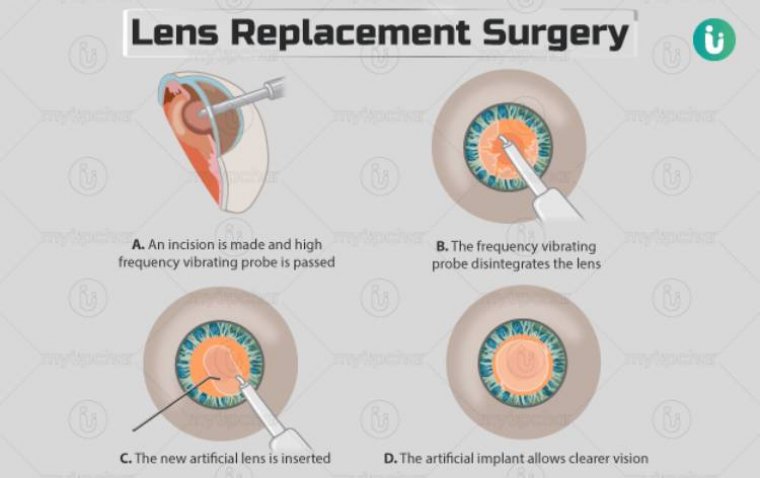
Modern cataract surgery has witnessed remarkable advancements, with phacoemulsification taking center stage. This technique employs ultrasonic energy to emulsify and remove the cataract through a tiny incision, promoting quicker recovery and reduced complications. The use of phacoemulsification has significantly minimized the need for large incisions, leading to quicker healing times and reduced induced astigmatism. Patients undergoing modern cataract surgery can often experience improved visual outcomes sooner after the procedure.
(1).jpg)
In addition to phacoemulsification, the integration of femtosecond laser technology has further elevated the precision of modern cataract surgery. Femtosecond lasers allow for accurate corneal incisions and efficient lens fragmentation, enhancing the predictability and safety of the surgery. This technology enables surgeons to customize incisions based on the unique characteristics of each patient's eye, leading to optimized outcomes. As these technological innovations continue to evolve, the landscape of cataract surgery is continually reshaped, offering patients safer, more tailored, and efficient procedures.
Here's a complete guide to cataract surgery.
Future of Cataract Surgery
The future of cataract surgery holds exciting prospects, driven by ongoing research and technological advancements. As we explore what lies ahead, it's clear that the field is poised for further breakthroughs.
The future of cataract surgery is set to be shaped by cutting-edge technologies and refined surgical techniques. Advancements in artificial intelligence and robotics are likely to play a significant role in enhancing surgical precision and outcomes. Additionally, the development of next-generation intraocular lenses with adjustable focus and enhanced durability promises to provide patients with even more personalized solutions. Stay tuned as the world of ophthalmology continues its forward march, offering new horizons for cataract patients.
A research in the field of cataract surgery has focused on enhancing intraocular lens technology. A study published in the Journal of Cataract & Refractive Surgery introduced a novel adjustable-focus intraocular lens. This innovative lens design allows for postoperative adjustments to optimize visual outcomes, addressing issues such as residual refractive errors. The preliminary results indicate promising potential for this customizable approach, opening new avenues for personalized cataract surgery tailored to individual patient needs.
Another area of active exploration involves the integration of artificial intelligence (AI) in surgical planning and execution. Ongoing trials are assessing the feasibility of AI-assisted cataract surgery, aiming to enhance surgical precision and reduce complications. By leveraging machine learning algorithms, surgeons can receive real-time insights, contributing to more accurate incisions and improved overall outcomes. As these research endeavors progress, the future of cataract surgery appears increasingly dynamic, with advancements poised to elevate the standard of care for patients.
Conclusion
In conclusion, the history of cataract surgery reflects a fascinating journey of innovation and continuous improvement. From early, rudimentary methods to the highly sophisticated procedures of today, the field has come a long way. As we stand at the crossroads of the past and the future, it's evident that cataract surgery will continue to evolve, offering enhanced vision and quality of life for patients worldwide.
(1).jpg)