Glaucomatous Optic Neuropathy & Latest Treatments
Glaucomatous optic neuropathy is characterized by progressive loss of retinal ganglion cells (RGCs) and their axons and leads to measureable structural and functional damage to the optic nerve, visual impairment, and blindness.
The primary site of injury is thought to be at the lamina cribrosa (LC), where the initial damage appears to be an interruption of normal axoplasmic flow. This is accompanied by progressive laminopathy and transsynaptic degeneration.
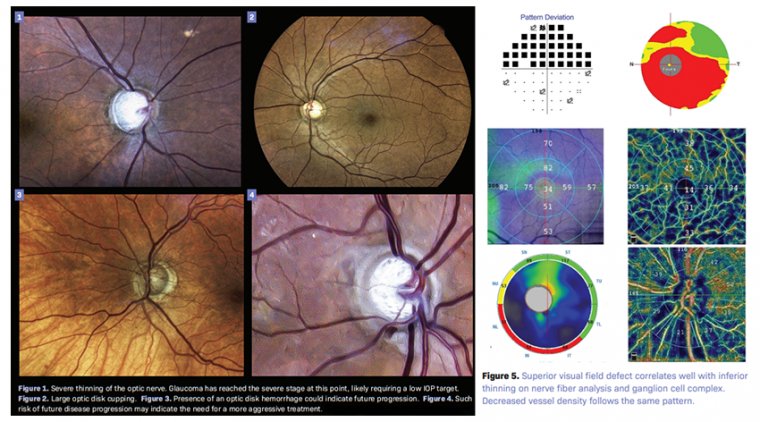
Structural changes to the RGCs and their axons can be observed clinically as alterations in the retinal nerve fiber layer (RNFL) and optic nerve topography and can be imaged by computerized devices such as spectral-domain optical coherence tomography (OCT) in the macula, RNFL, optic disc, and lamina, which facilitate diagnosis, monitoring, and treatment. RGC loss has functional correlates.
Risk factors for the onset and progression of open-angle glaucoma include systemic and ocular factors such as older age, lower ocular perfusion pressure, African or Latino ancestry, intraocular pressure (IOP), splinter hemorrhage at the optic nerve head (ONH), thinner central cornea, beta-zone parapapillary atrophy (PPA), and exfoliation syndrome.
The purpose of this chapter is to review these and novel risk factors and the evolving paradigms that incorporate them into diagnosis and management.
As the most common cause of irreversible blindness worldwide, glaucomatous optic neuropathy is well known to optometrists, and clinicians are comfortable diagnosing and managing it.
For years, the standard algorithm has changed little: treat patients with topical medications until the disease becomes severe enough to consider incisional surgery.
In the past decade, however, this strategy has been dramatically upended by the introduction of several new medications, a new understanding of the role of lasers, and the rapid growth of low-risk microsurgeries.
Although the diagnosis of glaucoma has only advanced modestly in recent years, the management of the disease has undergone a transformation. In particular, management has shifted toward intervention that is earlier, safer, and often more surgical.
This 2-part series will review the new landscape of glaucoma management: part 1 will cover new medications and the use of lasers, and part 2 will focus on the minimally invasive glaucoma surgery (MIGS).
Approach to Management
Glaucoma is a chronic progressive optic neuropathy that causes irreversible peripheral and/or central vision loss and may ultimately lead to blindness.
Approximately 76 million individuals have glaucoma worldwide, a number that will increase over the next 2 decades. Risk factors for glaucoma include older age, a family history of glaucoma, non-White race, thinner corneas, and elevated intraocular pressure (IOP).
There are many subtypes of glaucoma, a topic beyond the scope of this article. The only modifiable risk factor for most subtypes is elevated IOP, and almost all existing treatments are aimed at lowering IOP.
Glaucoma management is notoriously difficult to standardize, and treatment decisions are highly personal to each patient. Many factors must be considered, including pretreatment IOP, the severity of glaucomatous damage, the rate of progression, and the patient’s life expectancy.
Generally, a more aggressive treatment is recommended for younger individuals, those with severe disease or a fast rate of progression, those with low unmanaged IOP, and those with additional risk factors.
Many doctors choose to set a target IOP for each eye; this number can then guide treatment, as it is considered to be the highest acceptable IOP that is still likely to prevent or slow further vision loss.
Target IOP can be determined based on a percentage reduction from pretreatment IOP or on the stage of glaucoma (Sidebar: How to set a target IOP).
Selective Laser Trabeculoplasty
As the glaucoma armamentarium becomes more varied and powerful, many doctors are realizing that improving patient care means managing glaucoma sooner and more safely but also more aggressively.
Selective laser trabeculoplasty (SLT) illustrates this point. SLT is a 532-nm Q-switched, frequency-doubled neodymium:yttrium-aluminum-garnet (Nd:YAG) laser that delivers very short pulses of energy to pigmented trabecular meshwork (TM) cells.
No structural or coagulative damage has been found in the TM after treatment, the procedure is painless, and it results on average in a decline in IOP of 17% to 30%. SLT is indicated for mild to moderate cases of open angle, pigment dispersion, or pseudoexfoliative glaucoma.
Since the introduction of SLT in 2001, doctors in the US have tended to regard the use of SLT as a secondary attempt after maximum drop therapy has failed, usually just before incisional surgery becomes necessary.
This changed recently with the publication of the LiGHT study (NCT03395535) in 2019, in which investigators showed defi nitively that SLT was superior to topical medications in effi cacy, safety, and cost, and strongly recommended considering SLT before starting any drops.
As the conclusions of this landmark study reverberate through the profession, optometrists and ophthalmologists have adjusted their treatment algorithm. A diagnosis of glaucoma now frequently triggers using SLT first, instead of topical medications.
Patient satisfaction with SLT is higher than with drops, and adherence is no longer an issue. SLT can be repeated as frequently as needed, and repeated SLT often results in greater effectiveness.
Interestingly, investigators have uncovered suggestions that the current protocol of maximum-power SLT performed as needed might be inferior to low-power SLT performed annually.
This inquiry has given rise to a large clinical trial whose results, once released, might change once again the use of this therapy.
Topical Medications
Historically, topical medications have been considered the fi rst-line treatment for patients with glaucoma. There are now 5 major categories of IOP-lowering eye drops: prostaglandin analogues, ρ-kinase inhibitors, β-blockers, α-agonists, and carbonic anhydrase inhibitors.
Prostaglandin analogues (PGAs) reduce IOP by decreasing outflow resistance within the uveoscleral pathway.
PGAs have been the firstline drops for many years, and despite the recent introduction of several more potent medications, they maintain that status due to their effectiveness, once-daily dosing, affordability, and low risk of adverse effects.
The use of PGAs has been correlated with a decrease in the number of trabeculectomies performed. PGAs commonly produce a 25% to 33% reduction in IOP, although the effect is more pronounced in patients with higher baseline IOPs.
The PGAs can produce adverse effects of hyperemia, hypertrichosis, and periorbital fat atrophy.
The New Hypotensives
The FDA recently approved 3 new glaucoma topical medications that have had a large impact on prescribing patterns.
The first of these, latanoprostene bunod (Vyzulta, Bausch + Lomb), was released in 2017. Latanoprostene bunod combines the known agent latanoprost with nitric oxide. Nitric oxide increases aqueous outfl ow by relaxing chronic TM contraction.
This provides an IOP reduction of 1 to 2 mmHg more than a PGA alone while maintaining the same dosing schedule. Netarsudil 0.2% (Rhopressa, Aerie Pharmaceuticals), a ρ-kinase (ROCK) inhibitor, also was introduced in 2017.
The ρ-kinase enzyme promotes contraction of TM cells and matrix, so inhibition of the enzyme by this drug increases the outflow of aqueous fluid through the TM. The use of netarsudil produces conjunctival hyperemia in 50% of patients—a signifi cant adverse effect.
Like the PGAs, Netarsudil is dosed once daily at bedtime. On average, it results in a 25% to 30% drop from baseline IOP. Netarsudil has been combined with latanoprost to create Rocklatan (Aerie), an effective combination medication.
Rocklatan offers the highest average IOP reduction of any single glaucoma medication: 30% to 36% from baseline. The instillation regimen is identical to the PGAs, latanoprostene bunod, and netarsudil: once daily at bedtime.
It is important to discuss the significant adverse effects of conjunctival hyperemia and corneal verticillata prior to starting this drop, in addition to the adverse effects linked to the latanoprost moiety.
The introduction of netarsudil and nitric oxide has affected the treatment algorithm significantly. Whereas many doctors continue to start any topical therapy with a PGA, if this drug proves insuffi ciently potent, they may consider switching to Vyzulta or Rocklatan.
The instillation burden for these medications is no greater than that of the original PGA, and most patients will see a further reduction in their IOPs.
The Traditional Hypotensives
Older topical medications can still play a helpful role in the reduction of IOP. These include β-blockers, α-agonists, and carbonic anhydrase inhibitors.
By decreasing aqueous production, β-blockers reduce IOP. They are less likely to cause ocular surface issues; however, cardiac or respiratory adverse effects may occur.
These should be avoided in patients with bradycardia, hypotension, asthma, and obstructive pulmonary disease. Patients who are already using systemic β-blockers should be carefully monitored when taking topical β-blockers.
Carbonic anhydrase inhibitors and α-agonists are commonly used second-line agents. These can be added to a patient’s regimen when a monotherapy is not sufficient. The α-agonists frequently cause conjunctival hyperemia.
Unfortunately, increasing the number of drops used daily negatively affects patient adherence to therapy. According to some studies, fewer than 50% of patients continue adhering to therapy beyond the fi rst year.
Combination therapies may help patient adherence and reduce exposure to preservatives. In cases of more severe disease and when a significant decrease in IOP is needed, a combination drop is preferred, as it will simplify the administration schedule and provide greater IOP reduction.
The list of combination drops available in the US includes timolol plus brimonidine (Combigan, Allergan), timolol plus dorzolamide (Cosopt/Cosopt PF, Akorn), brimonidine plus brinzolamide (Simbrinza, Alcon), and Rocklatan.
How to Eliminate Nonadherence
The largest factor interfering with the success of medical glaucoma treatment is patient inability to adhere to topical therapy as prescribed.
Challenges with drop adherence include difficulty with drop administration, adverse effects, and the expense of medications.
Thorough patient education regarding the severity and permanence of potential vision loss might seem like a powerful way to address poor adherence but is actually surprisingly ineffective.
It may not be the lack of education that precludes patients from taking their glaucoma medication, but rather various aspects of their lifestyles, such as level of busyness, time away from home, or forgetfulness.
This is supported by the fact that younger patients have higher nonadherence rates, despite having better access to information about glaucoma. Medications with the easiest administration, such as once-daily regimens, should be strongly considered as first line treatments.
The more complex the medication regimen, the lower the rate of adherence to therapy.26 Utilizing treatment modalities that are not reliant on constant patient cooperation will result in better continuity of care.
This includes SLT, surgeries, and sustained-release implants. Sustained-release medications may soon become a highly effective option for managing glaucoma. The only device approved for use at this point is the bimatoprost intracameral implant Durysta (Allergan).
The solid, biodegradable, rod-shaped implant is placed in the anterior chamber angle and then slowly releases a prostaglandin analog as its copolymer matrix degrades. The intracameral implant is capable of delivering medication for up to 6 months but is not yet approved for repeat use.
A New Paradigm
We are in the midst of a paradigm shift in the management of glaucoma. Our management of this disease has shifted towards intervention that is earlier, safer, and often more surgical.
We now know that a large proportion of patients do not use their eye drops as prescribed, and the wave of new once-daily drops and the increased use of SLT laser as a first-line treatment are powerful strategies to produce more consistent results.
Another powerful strategy has been the increased use of MIGS, which will be treated in the second part of this 2-part series. The field of glaucoma has recently become significantly more exciting, and is evolving quickly.
As optometrists master the new options, we will be able to offer our patients a higher standard of care, which can result in signifi cantly less vision lost to this disease.
(1).jpg)