Parinaud Oculoglandular Syndrome: A Unique Blend of Ocular and Glandular Symptoms
Parinaud oculoglandular syndrome is a relatively rare yet intriguing medical condition that intertwines ocular and glandular manifestations. Characterized by its distinct combination of eye-related symptoms and glandular involvement, this syndrome presents a unique challenge for both patients and medical professionals.
In this article, we delve into the nuances of parinaud oculoglandular syndrome, shedding light on its symptoms, causes, and treatment options.
What Causes Parinaud Oculoglandular Syndrome?
Parinaud oculoglandular syndrome, an intricate interplay of ocular and glandular symptoms, finds its roots in specific causes and risk factors that contribute to its emergence.
1. Bacterial and Viral Infections
Bacterial and viral infections serve as key precipitating factors in the development of parinaud oculoglandular syndrome. These infectious agents infiltrate ocular and glandular tissues, triggering an immune response that subsequently manifests as the syndrome's distinctive symptoms. While various pathogens can be implicated, two specific ones stand out:
● Bartonella henselae: This bacterial pathogen, primarily transmitted through cat scratches or bites, is a significant causative agent of parinaud oculoglandular syndrome. Commonly associated with cat-scratch disease, Bartonella henselae invades the body, leading to ocular inflammation and tender lymph nodes near the ear.
● Francisella tularensis: This bacterium is responsible for tularemia, a disease often contracted through contact with infected animals or contaminated environments. Francisella tularensis can instigate both ocular and glandular symptoms, contributing to the manifestation of parinaud oculoglandular syndrome.
Risk Factors for Parinaud Oculoglandular Syndrome
Several risk factors amplify the likelihood of developing parinaud oculoglandular syndrome. These factors increase susceptibility to the causative pathogens and play a pivotal role in initiating the cascade of symptoms. Two prominent risk factors include: exposure to animals and contaminated environments.
Exposure to Animals: Close contact with animals, especially cats, increases the risk of encountering Bartonella henselae. Scratches, bites, or even simple interactions with infected animals can serve as pathways for the transmission of this bacterium. Thus, individuals who frequently interact with cats or other potentially infected animals face a higher risk of developing the syndrome.
Contaminated Environments: Francisella tularensis, the bacterial agent behind tularemia, can be found in various environments, including soil, water, and even certain animals like rabbits and rodents. Individuals who engage in outdoor activities, such as gardening or hunting, or those inhabiting regions with a higher prevalence of tularemia-carrying vectors, are at an elevated risk of exposure.
Symptoms of Parinaud Oculoglandular Syndrome
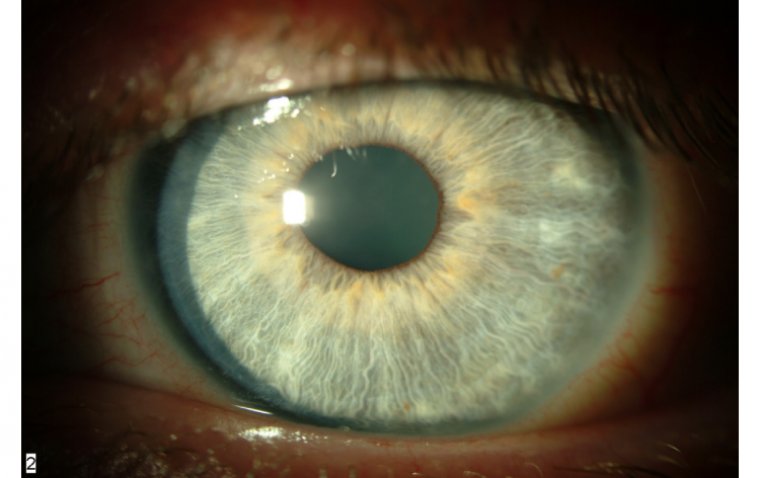
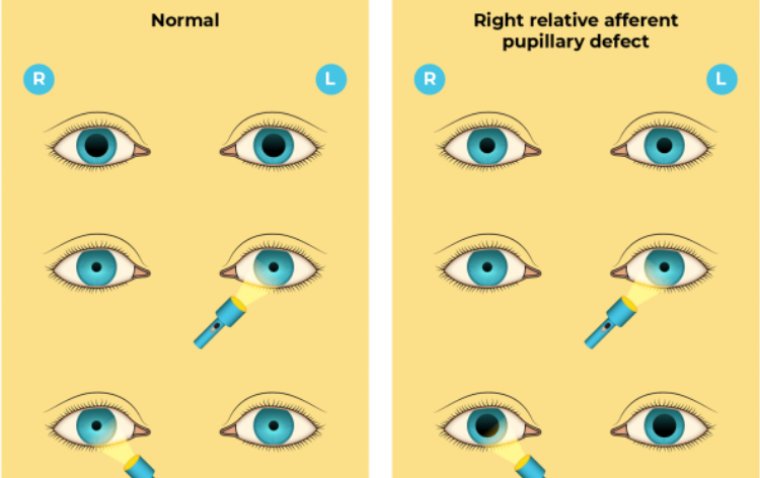
1. Ocular Symptoms: One of the hallmark features of parinaud oculoglandular syndrome is the presence of various ocular symptoms that affect the eye's surface and appearance. These symptoms include:
● Conjunctivitis: The inflammation of the conjunctiva, the thin tissue covering the front of the eye and inner eyelids, often leading to redness and discomfort.
● Eye Redness: Visible redness of the eye due to inflammation and increased blood flow.
● Swollen Eyelids: Eyelid swelling, also known as blepharitis, which can cause discomfort and impact visual appearance.
● Tender Lymph Nodes: Enlarged and tender lymph nodes in the region close to the ear, reflective of the body's immune response to the underlying condition.
.jpg)
Diagnosing Parinaud Oculoglandular Syndrome
Diagnosing parinaud oculoglandular syndrome requires a comprehensive approach that considers the distinct blend of ocular and glandular symptoms. As a condition characterized by its unique interplay between eye inflammation and tender lymph nodes, a systematic evaluation becomes crucial in ensuring accurate diagnosis and effective management.
1. Medical History and Clinical Examination
A meticulous review of the patient's medical history forms the initial step in diagnosing parinaud oculoglandular syndrome. Physicians inquire about recent exposure to animals, especially cats, as well as any outdoor activities that might have led to contact with potentially contaminated environments. These insights provide valuable context for the subsequent assessment.
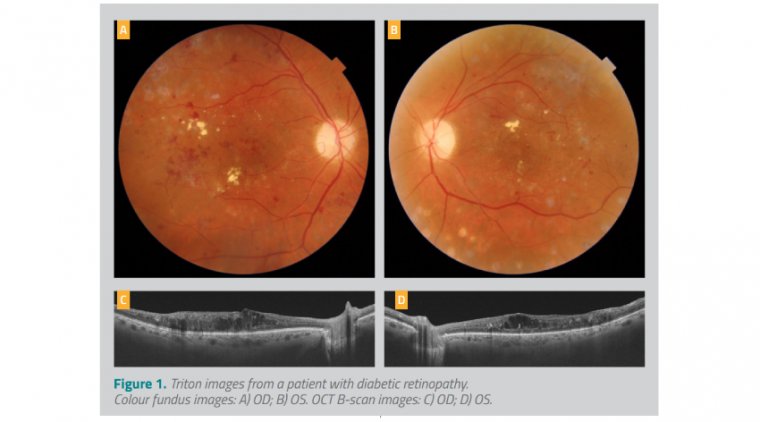
A thorough clinical examination follows, focusing on both the ocular and glandular symptoms. Ocular symptoms such as conjunctivitis, eye redness, and swollen eyelids are evaluated, along with the presence of any discharge or discomfort. Tender lymph nodes near the ear are palpated to assess the extent of glandular involvement.
2. Laboratory Tests and Imaging
Laboratory tests play a crucial role in confirming the diagnosis of parinaud oculoglandular syndrome. These tests aid in identifying the specific pathogens responsible for the condition, thus guiding treatment decisions. Key laboratory assessments include:
● Blood Tests: Serological tests can detect antibodies against pathogens like Bartonella henselae or Francisella tularensis, providing evidence of infection.
● Biopsy: In cases where diagnosis remains uncertain, a biopsy of the affected lymph nodes might be performed to identify the causative agents.
Imaging studies, such as ultrasound or computed tomography (CT) scans, can offer insights into the extent of lymph node involvement and aid in determining appropriate treatment strategies.
3. Differential Diagnosis
Parinaud oculoglandular syndrome's overlapping symptoms with other conditions necessitate a thorough process of exclusion. Differential diagnosis involves ruling out other potential causes of similar symptoms, such as:
● Conjunctivitis: Differentiating parinaud oculoglandular syndrome from isolated conjunctivitis is crucial. Conjunctivitis can arise from various causes, including allergies or other infections.
● Other Glandular Infections: Conditions like viral or bacterial infections unrelated to parinaud oculoglandular syndrome must be considered and ruled out through careful assessment.
4. Consultation with Specialists
Given the syndrome's complexity, consultation with specialists might be warranted. Ophthalmologists and infectious disease specialists can provide their expertise in confirming the diagnosis and devising an effective treatment plan.
How to Treat Parinaud Oculoglandular Syndrome
Managing parinaud oculoglandular syndrome involves a multi-pronged strategy to alleviate symptoms and target the underlying infection:
Antibiotic Therapy: Prescribed antibiotics like azithromycin or doxycycline combat bacteria like Bartonella henselae or Francisella tularensis.
Anti-Inflammatories: Topical steroids and NSAIDs reduce eye inflammation, redness, and discomfort.
Supportive Care: Warm compresses, artificial tears, rest, and hydration provide relief and aid healing.
Regular Monitoring: Ongoing appointments with specialists ensure treatment effectiveness and adjustments as needed.
Preventive Measures: Minimize animal contact, wear protective gear outdoors, and practice hygiene to prevent recurrence.
By tailoring treatments to address both ocular and glandular symptoms, individuals can achieve optimal recovery and prevent future occurrences.
(1).jpg)