Irvine-Gass Syndrome: A Comprehensive Guide to Retinal Swelling
What Is Irvine–Gass Syndrome?
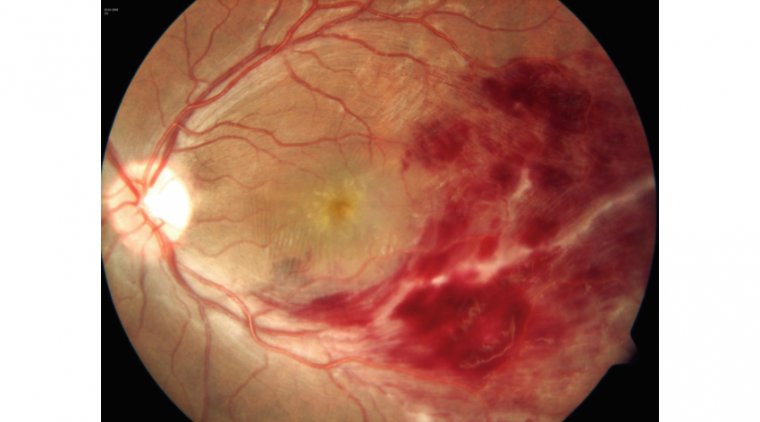
Irvine–Gass Syndrome, also known as cystoid macular edema (CME), is a notable complication that can occur after cataract surgery. It is characterized by the accumulation of fluid in the macula, the central region of the retina responsible for sharp, central vision. This accumulation can lead to blurred vision, distortion, and even a reduction in visual acuity, hampering an individual's ability to carry out daily tasks that require focused vision, such as reading or driving.
Given that cataract surgery is one of the most commonly performed surgical procedures worldwide, understanding the risks associated with Irvine–Gass Syndrome is crucial. While the syndrome is generally rare, occurring in a small percentage of cataract surgeries, its impact on vision can be significant. Therefore, awareness and understanding of this condition are essential for both healthcare providers and patients alike, ensuring that early diagnosis and intervention can take place to mitigate its effects.
What Causes Irvine–Gass Syndrome?
The primary cause of Irvine–Gass Syndrome is usually linked to surgical trauma incurred during cataract surgery. The procedure, although generally considered safe, involves making incisions in the eye and replacing the natural lens with an artificial one. This can inadvertently lead to the disruption of the blood-retinal barrier, increasing the permeability of capillaries in the macula, and subsequently causing fluid accumulation.
Role of Inflammation
Inflammation plays a crucial role in the development of this syndrome. The surgical trauma triggers an inflammatory response as part of the body's natural healing process. While inflammation is generally beneficial for warding off infections and facilitating tissue repair, it can also have detrimental effects. In the case of Irvine–Gass Syndrome, pro-inflammatory mediators like cytokines are released, leading to vasodilation and increased vascular permeability in the retina. This, in turn, allows fluid to accumulate in the macular region, causing the characteristic symptoms of the syndrome.
Additional risk factors that could contribute to the onset of Irvine–Gass Syndrome include:
● Previous Eye Diseases: Individuals with a history of retinal conditions, uveitis, or diabetic retinopathy may be at higher risk.
● Complex Surgeries: Surgeries that are complicated or lengthy can cause more trauma to the eye, increasing the risk of developing the syndrome.
● Medication: The use of certain medications, like prostaglandin analogs, may exacerbate the condition.
Symptoms and Clinical Presentation of Irvine–Gass Syndrom
Irvine–Gass Syndrome primarily manifests as decreased visual acuity, often described as blurriness or haziness. Patients may also experience distortion of vision, where straight lines appear wavy. Another common symptom is metamorphopsia, which is the perception of a grid of straight lines as wavy and sometimes separated with dark areas. Additionally, there may be central scotoma, an area of decreased or lost vision in the visual field.
Other associated symptoms can include:
● Photophobia: Sensitivity to light
● Pain or Discomfort: Usually mild, this can vary from patient to patient.
● Fluctuating Vision: Visual symptoms may improve and worsen over the course of the day.
Acute vs. Chronic Presentation
1. Acute Presentation: In acute cases, symptoms usually appear soon after cataract surgery—often within a period of weeks. These symptoms can be more severe but are usually responsive to treatment, which typically includes corticosteroids to reduce inflammation.
2. Chronic Presentation: Chronic cases may take a longer time to manifest and can be more challenging to manage. In chronic presentations, symptoms might be milder but are persistent, sometimes lasting for several months. Chronic forms might require prolonged treatment and close monitoring, and they may not respond as well to standard therapies.
How to Diagnose Irvine–Gass Syndrome
Diagnosis of Irvine–Gass Syndrome is largely clinical, often beginning with a detailed medical history and a comprehensive ophthalmologic examination. This includes checking for symptoms like decreased visual acuity, distorted vision, and other symptoms that patients might report post-cataract surgery.
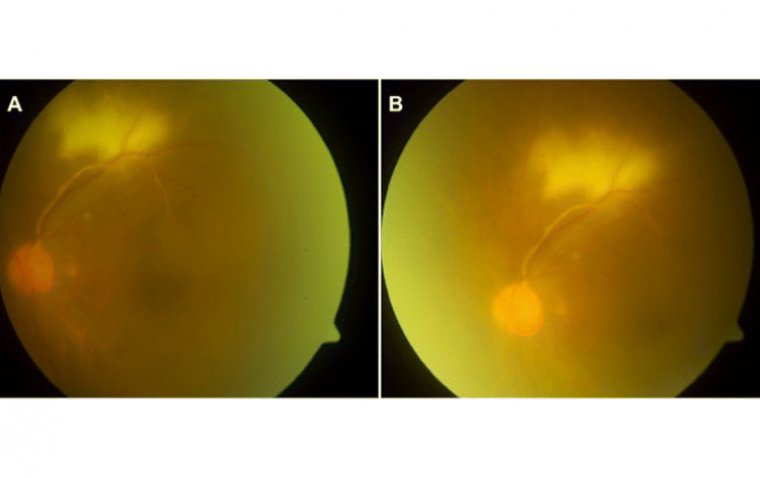
1. Optical Coherence Tomography (OCT): This non-invasive imaging test allows healthcare providers to see cross-sectional images of the retina, helping them to detect any swelling or changes in the macula, which are typical of Irvine–Gass Syndrome.
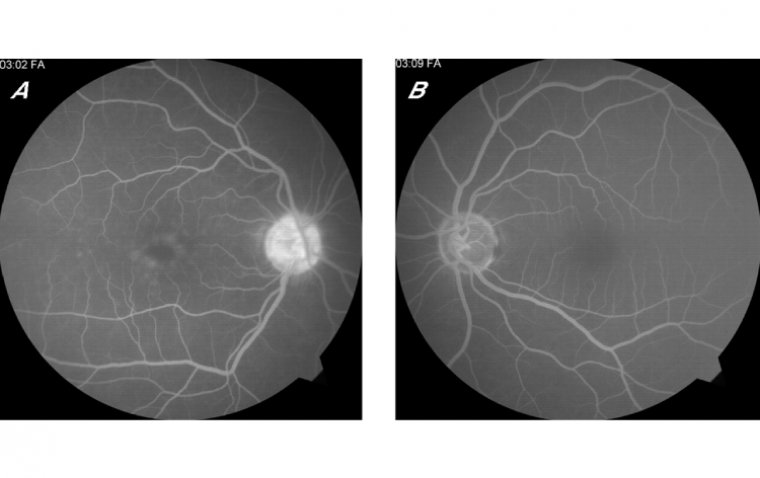
2. Fluorescein Angiography: In this procedure, a fluorescent dye is injected into the bloodstream. The dye highlights the blood vessels in the back of the eye so they can be photographed. This test helps to rule out other potential causes of vision loss and can provide important details about blood flow in the retina and choroid, further aiding the diagnosis.
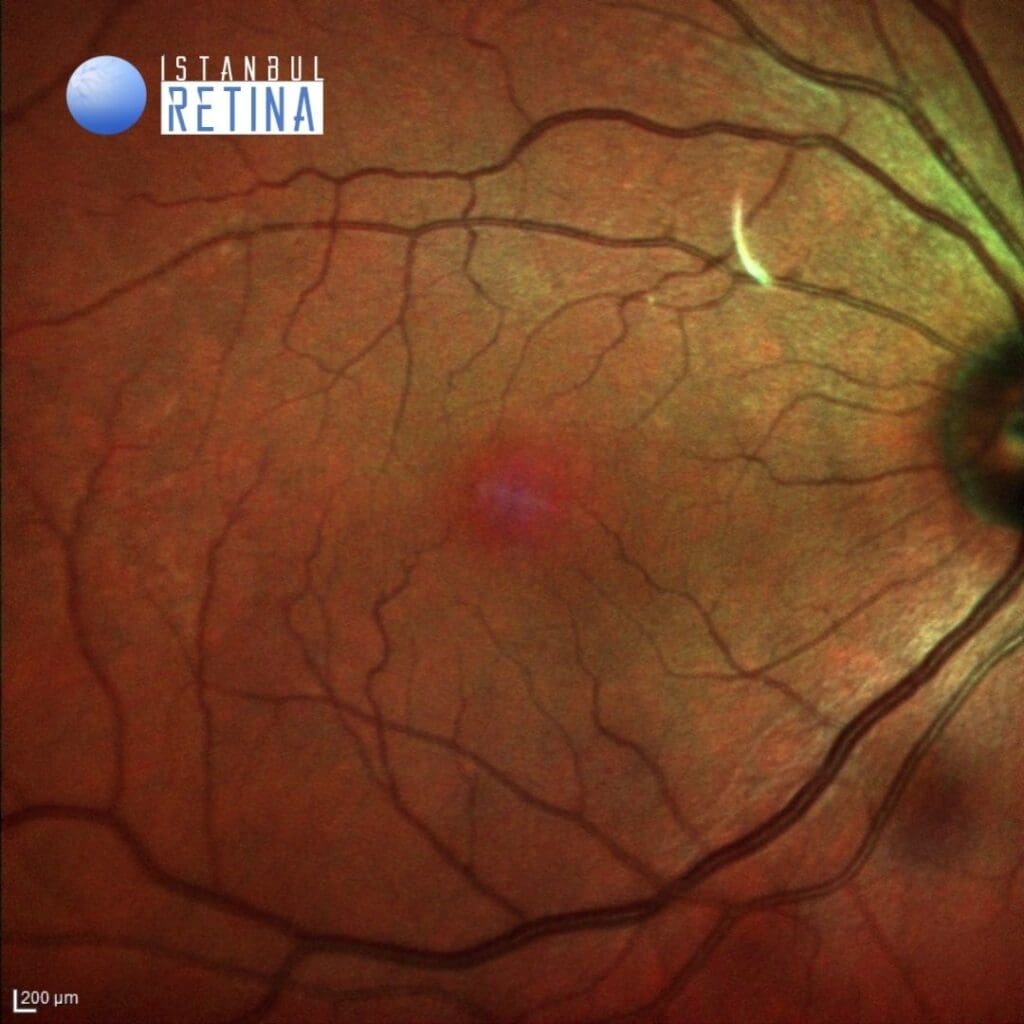
3. Fundus Examination: Examination of the interior surface of the eye, including the retina, is also performed to assess the condition of the macula and other retinal structures.
4. Visual Acuity Test: Measuring the sharpness of vision can indicate changes in visual acuity, which is often a symptom of Irvine–Gass Syndrome.
5. Visual Field Testing: This may be performed in some cases to evaluate if there is any loss in peripheral vision.
6. Additional Blood Tests: While not always necessary, blood tests may sometimes be conducted to rule out other systemic conditions that could contribute to the symptoms.
Treatment Options for Irvine–Gass Syndrome
Medical Interventions
● Topical Anti-Inflammatory Eye Drops: Corticosteroid eye drops are commonly used to treat inflammation and may help to reduce macular edema in Irvine–Gass Syndrome.
● Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Topical NSAID eye drops are another option for reducing inflammation and can sometimes be used in conjunction with corticosteroids.
● Intravitreal Injections: In more severe cases, anti-VEGF (Vascular Endothelial Growth Factor) injections or corticosteroid injections may be given directly into the eye to reduce macular edema.
Surgical Options
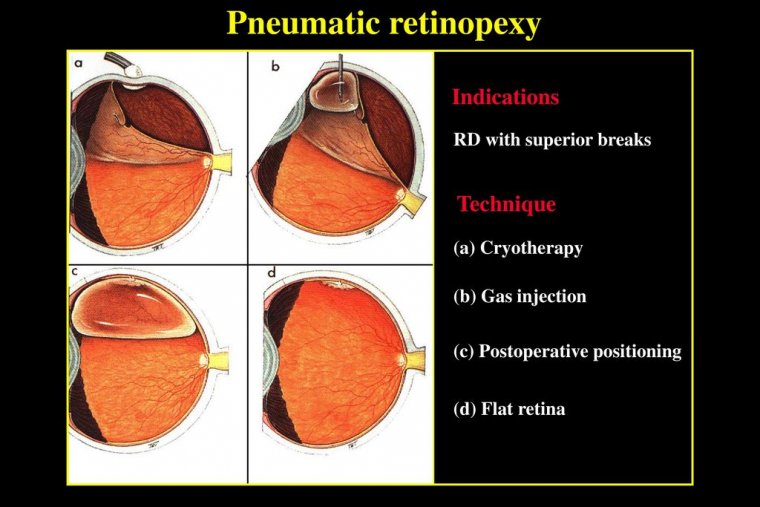
Surgical intervention is generally not the first-line treatment for Irvine–Gass Syndrome, given that it’s a post-surgical complication to begin with. However, in extreme cases where pharmacological treatments fail:
● Vitrectomy: A surgical procedure to remove the vitreous humor gel that fills the eye cavity to ease the condition may be considered. This is generally a last resort.
Pharmacological Treatments
● Oral Carbonic Anhydrase Inhibitors: Drugs such as acetazolamide can sometimes be prescribed to reduce fluid production in the eye, thereby treating macular edema. However, these are generally reserved for severe or refractory cases due to their side effect profile.
● Immunomodulatory Therapy: In cases where Irvine–Gass Syndrome is thought to be linked to systemic inflammatory or autoimmune conditions, immunomodulatory drugs like methotrexate may be considered.
Adjunctive Therapies
● Laser Therapy: Focal laser treatment has been used historically to treat macular edema, though it is generally less favored compared to intravitreal injections in the treatment of Irvine–Gass Syndrome.
● Monitoring and Follow-Up: Regular eye exams and imaging studies like OCT are crucial for monitoring the effectiveness of treatment and making necessary adjustments.
Preventing Irvine–Gass Syndrome
Preoperative Measures
1. Risk Assessment: Before undergoing cataract surgery, discuss any preexisting conditions, medications, or risk factors with your ophthalmologist. Certain systemic conditions like diabetes may increase the risk of complications.
2. Medical Optimization: Ensuring that other medical conditions are well-controlled before surgery may reduce the risk of post-surgical complications.
3. Pre-Surgery Medications: Anti-inflammatory eye drops or other medications may be prescribed before the surgery to preemptively control inflammation.
4. Choosing an Experienced Surgeon: The skill and experience of the ophthalmologist performing the surgery may influence outcomes. Be sure to choose a healthcare provider with a track record of success in cataract surgeries.
Postoperative Measures
● Follow Post-Surgery Guidelines: Adherence to post-operative care instructions, including medication schedules, can significantly reduce the risk of complications.
● Regular Follow-ups: Early post-operative follow-up visits are crucial for detecting any early signs of Irvine–Gass Syndrome. Timely intervention can mitigate the severity of symptoms and may prevent long-term issues.
● Anti-inflammatory Medications: Continuation of anti-inflammatory eye drops or other medications may be recommended post-surgery to control any inflammation.
● Monitoring: Optical coherence tomography (OCT) scans or other imaging tests may be conducted during follow-up visits to monitor for signs of macular edema.
● Immediate Reporting: Patients should be educated to report any visual changes or discomfort immediately, as this may signify the onset of complications like Irvine–Gass Syndrome.
● Lifestyle Adjustments: While not directly related to Irvine–Gass Syndrome, maintaining a healthy lifestyle can promote faster healing and reduce the risk of other complications.
Summary
Irvine–Gass Syndrome is a notable concern for those considering or having recently undergone cataract surgery. This post-surgical complication arises primarily due to surgical trauma and the subsequent inflammatory response, which leads to macular edema. Symptoms often include blurred vision and visual distortion, and these can present in both acute and chronic forms.
Therefore, it's crucial for patients to have regular post-operative check-ups to catch any potential complications early. Diagnosing this syndrome accurately usually involves specialized tests, including optical coherence tomography (OCT) and fluorescein angiography. Once diagnosed, treatment options range from medical interventions like anti-inflammatory medications to more advanced surgical or pharmacological treatments in severe cases.
Prevention is especially crucial for those at higher risk. Effective preventive measures include both preoperative and postoperative protocols, such as the use of anti-inflammatory medications and regular follow-up visits to the ophthalmologist. If you are planning a cataract surgery or have recently undergone one, being aware of the symptoms and the need for early diagnosis can make a significant difference in your treatment outcomes.
(1).jpg)