Intraocular Corticosteroids Proven as the Best Treatment for Uveitic Macular Edema
Repeat corticosteroid injections were found to be more effective in improving vision for individuals with persistent or recurrent uveitis-related macular edema compared to methotrexate or ranibizumab intravitreal injections, according to a recent clinical trial. The corticosteroid treatment exhibited superior results in reducing retinal swelling and was the sole therapy in the study to enhance vision. The findings were published in the journal Ophthalmology.
"Prior to this study, we didn't know the best treatment for persistent or recurrent macular edema, a major cause of vision loss in people with uveitis," said Douglas A. Jabs, M.D., Johns Hopkins Bloomberg School of Public Health, Baltimore, chair of the study. "This trial strongly indicates that repeat intraocular corticosteroid injections are superior to either intravitreal injections of methotrexate or ranibizumab."
Uveitis encompasses various inflammatory conditions that affect different parts of the eye, including the front (anterior uveitis), middle (intermediate uveitis), back (posterior uveitis), or the entire eye (panuveitis).
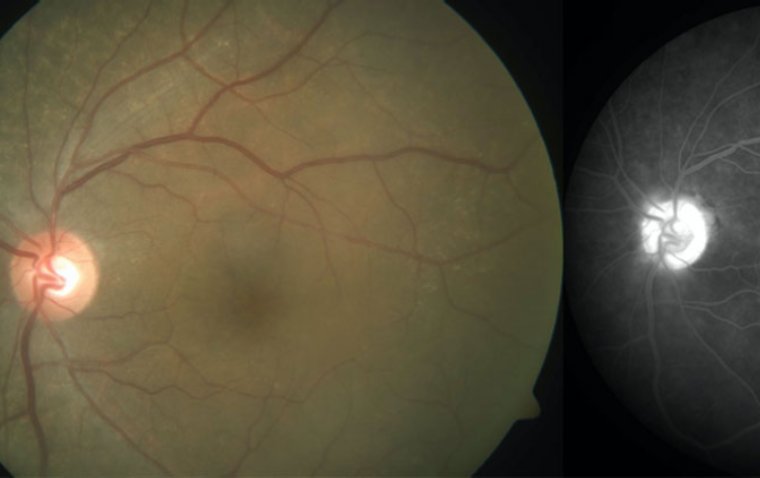
Inflammation within the eye can result in the accumulation of fluid in the central area of the retina, called the macula, leading to vision impairment. This condition, known as macular edema, is a common complication of uveitis that tends to persist or recur despite treatment for uveitis.
The primary aim of initial treatment for uveitis-related macular edema is to manage inflammation and reduce fluid accumulation beneath the retina. While oral corticosteroids may be effective for some patients, intraocular corticosteroid injections are often necessary for those with macular edema. One such treatment option is the dexamethasone intraocular implant.
However, it's important to note that intraocular corticosteroids can elevate intraocular pressure, which is a significant risk factor for glaucoma. Glaucoma can cause damage to the optic nerve and result in vision loss. Additionally, the use of intraocular corticosteroids may contribute to the development of cataracts, a condition characterized by the clouding of the eye's lens and subsequent visual impairment.
In this study, researchers compared three treatments for uveitis-related macular edema: an additional intraocular corticosteroid injection, an injection of the anti-vascular endothelial growth factor (anti-VEGF) drug ranibizumab, or an injection of the anti-inflammatory drug methotrexate.
Anti-VEGF injections are commonly used to treat age-related macular degeneration and macular edema associated with various causes, including diabetic retinopathy. Previous small-scale studies indicated that ranibizumab injections and the anti-inflammatory properties of methotrexate might have potential in reducing uveitis-related macular edema.
About the Study
The clinical trial enrolled 194 participants (225 study eyes) who had well-controlled uveitis but persistent or recurrent macular edema. Among them, 65 participants received dexamethasone corticosteroid, 65 participants received methotrexate, and 64 participants received ranibizumab. The study was conducted across 33 clinical centers in the United States, the United Kingdom, Australia, and India. All participants had previously undergone at least one intravitreal corticosteroid injection for uveitis-related macular edema.
The injection schedules for each group were based on typical clinical practice. The corticosteroid group received one dexamethasone implant injection at the start, and if the macular edema persisted, another injection was administered at eight weeks. The methotrexate group received one injection at the beginning, followed by repeat injections at four and eight weeks if the macular edema did not resolve. The ranibizumab group received injections at the start, four weeks, and eight weeks, regardless of whether their macular edema resolved.
At the end of the 12-week period, all three groups exhibited reductions in retinal swelling. The dexamethasone group demonstrated the greatest reduction compared to the other two groups (35% reduction for corticosteroid; 20% for ranibizumab; 11% for methotrexate). Furthermore, only the corticosteroid group showed improvement in vision, with an increase of nearly five letters, equivalent to approximately one row on an eye chart. Although the corticosteroid group experienced more instances of mild increases in intraocular pressure, occurrences of elevated levels were rare (<10%) in all three groups.
"Intraocular corticosteroid treatment remains the most effective therapy for uveitis-related macular edema," said Nisha Acharya, M.D., University of California San Francisco, the lead author of the study. "The vision gains in participants who received the corticosteroid treatment were very promising."
Reference
Nisha R. Acharya et al, Intravitreal Therapy for Uveitic Macular Edema—Ranibizumab versus Methotrexate versus the Dexamethasone Implant, Ophthalmology (2023). DOI: 10.1016/j.ophtha.2023.04.011
(1).jpg)