Exploring the Causes and Treatments of Anterior Uveitis
Picture this: You're an astronaut on a space mission, and you've just stepped out of your spacecraft onto the surface of a mysterious new planet. Your eyesight is crucial to your survival in this alien environment, as you must rely on it to navigate the terrain and communicate with your crew. Just as you begin to explore, you experience a sudden onslaught of redness, pain, and blurry vision in your eyes. Panic sets in as you realize that your most important tool for survival is now compromised. Fortunately, this isn't an interstellar crisis; instead, it's an imaginative introduction to a common eye condition called anterior uveitis.
Now that we've captured your attention, let's switch gears to a more formal tone and dive into the specifics of anterior uveitis.
What Is Anterior Uveitis?
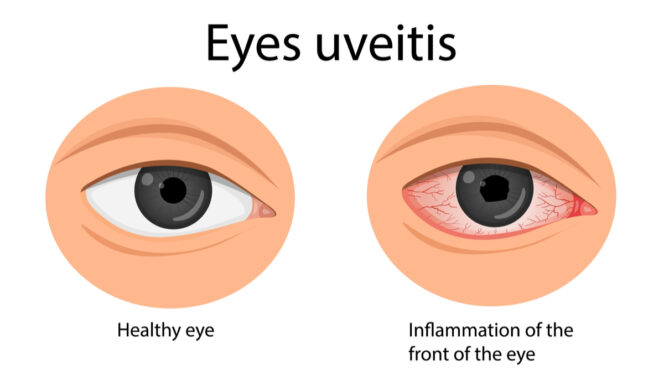
Anterior uveitis is an inflammation of the front portion of the uvea, which is a layer of tissue located between the retina and the sclera (the white of the eye). The uvea consists of three parts: the iris, the ciliary body, and the choroid. When the uvea becomes inflamed, it can lead to a host of uncomfortable symptoms and may cause vision problems if left untreated. This article will explore the causes and treatments of anterior uveitis, providing valuable information to help you better understand and manage this condition.
To fully grasp the complexities of anterior uveitis, it's essential to have a brief understanding of the anatomy of the eye. The human eye is a fascinating and intricate organ, with several components working together to provide us with clear and accurate vision. The cornea, located at the front of the eye, functions as the eye's primary lens, focusing light on the retina.
Behind the cornea lies the iris, which regulates the amount of light that enters the eye by adjusting the size of the pupil. The crystalline lens sits behind the iris, and it is responsible for refining the focus of the light onto the retina. The retina, found at the back of the eye, is a light-sensitive layer that converts light into electrical signals, which are then sent to the brain via the optic nerve. The uvea, which includes the iris, ciliary body, and choroid, provides essential nutrients and oxygen to the retina and regulates intraocular pressure.
.jpg)
Now that we have established the foundational knowledge of the eye's anatomy and the definition of anterior uveitis, we can delve into the various causes and treatments of this condition. In the following sections, we will explore the potential triggers of anterior uveitis, discuss the diagnostic process, and outline the available treatment options to manage and prevent complications.
Causes of Anterior Uveitis
Anterior uveitis can result from a wide range of causes and risk factors. In this section, we will discuss common causes, such as infections, autoimmune diseases, and trauma, as well as the risk factors that may predispose individuals to develop the condition.
1. Infections: Infections, particularly viral ones, are a common cause of anterior uveitis. Herpes simplex virus (HSV), varicella-zoster virus (VZV), and cytomegalovirus (CMV) are among the most frequent viral culprits. Bacterial infections, such as syphilis and Lyme disease, can also cause uveitis, although they are less common.
2. Autoimmune diseases: Autoimmune disorders, in which the immune system mistakenly attacks the body's healthy tissues, can also trigger anterior uveitis. Examples of autoimmune diseases that may be associated with uveitis include rheumatoid arthritis, ankylosing spondylitis, and Behçet's disease.
3. Trauma: Physical injury to the eye, such as a blow, a penetrating injury, or exposure to chemicals, can lead to the development of anterior uveitis as the body's inflammatory response is activated to repair the damaged tissue.
Risk Factors for Anterior Uveitis
1. Age: Anterior uveitis can affect people of all ages, but it is more commonly diagnosed in young adults and middle-aged individuals.
2. Gender: Although both men and women can develop anterior uveitis, some studies have suggested that women might be more susceptible to certain autoimmune-related causes of the condition.
3. Genetic factors: Some individuals may have a genetic predisposition to anterior uveitis, particularly if they have a family history of autoimmune diseases or other immune-related conditions. Certain genetic markers, such as HLA-B27, have been associated with an increased risk of developing uveitis.
4. Underlying medical conditions: People with pre-existing autoimmune diseases or immune-mediated conditions are at a higher risk of developing anterior uveitis due to the systemic nature of these disorders.
Symptoms and Diagnosis
Recognizing the symptoms of anterior uveitis and understanding the diagnostic process are crucial for timely intervention and effective treatment. In this section, we will discuss the common symptoms of anterior uveitis and the various diagnostic methods employed by eye care professionals.
Symptoms of Anterior Uveitis:
● Eye pain: Aching, throbbing, or stabbing pain in the affected eye is a common symptom of anterior uveitis. The pain may worsen when trying to focus on close objects or when adjusting to changes in light.
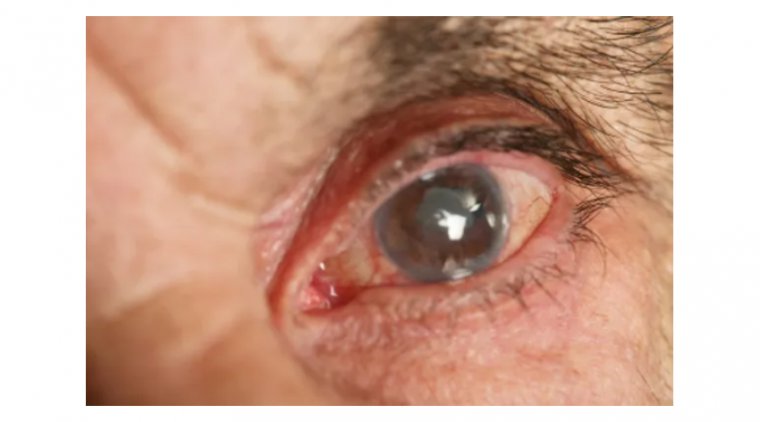
● Redness: The affected eye may appear red or bloodshot due to the inflammation of the blood vessels in the uvea.
●Sensitivity to light (photophobia): Individuals with anterior uveitis may find bright light uncomfortable and may experience increased tearing or squinting in response to it.
● Blurry vision: Inflammation can cause swelling of the eye structures, leading to blurry or hazy vision in the affected eye.
● Floaters: Some individuals may experience the presence of small specks or "floaters" in their field of vision, caused by the accumulation of inflammatory cells in the vitreous humor.
Diagnosis of Anterior Uveitis
A comprehensive evaluation by an ophthalmologist or optometrist is required to diagnose anterior uveitis. The diagnostic process typically involves the following steps:
● Physical examination: The eye care professional will conduct a thorough examination of both eyes, focusing on the affected eye. They will look for signs of inflammation, such as redness, swelling, and irregularities in the iris and pupil.
● Eye tests: A series of tests may be performed to assess the overall health of the eye and its structures. These may include measuring intraocular pressure, assessing visual acuity, and conducting a slit-lamp examination to visualize the front structures of the eye in detail.
● Laboratory tests: In some cases, blood tests, skin tests, or imaging studies may be ordered to help identify the underlying cause of the uveitis. These tests can be particularly helpful when an infectious or autoimmune etiology is suspected.
● Referral to a specialist: If the cause of anterior uveitis remains unclear or if the condition is severe, the eye care professional may refer the patient to a specialist, such as a uveitis specialist or a rheumatologist, for further evaluation and management.
Treatment and Management of Anterior Uveitis
Managing anterior uveitis effectively is essential to alleviate symptoms, control inflammation, and prevent complications. In this section, we will discuss the various treatment options available for anterior uveitis, the importance of treating its underlying cause, and the management of uveitis-related complications.
Treatment Options for Anterior Uveitis:
1. Medications: The primary treatment for anterior uveitis involves the use of medications to reduce inflammation and relieve symptoms. Eye drops containing corticosteroids are commonly prescribed to control inflammation. In some cases, oral corticosteroids or steroid injections may be necessary for more severe inflammation. Additional medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or cycloplegic agents, may be prescribed to manage pain and prevent complications.
2. Treating the underlying cause: If the uveitis is caused by an underlying infection or autoimmune disease, it is crucial to address the root cause in conjunction with treating the eye inflammation. This may involve the use of antibiotics or antiviral medications for infections or immunosuppressive drugs for autoimmune conditions.
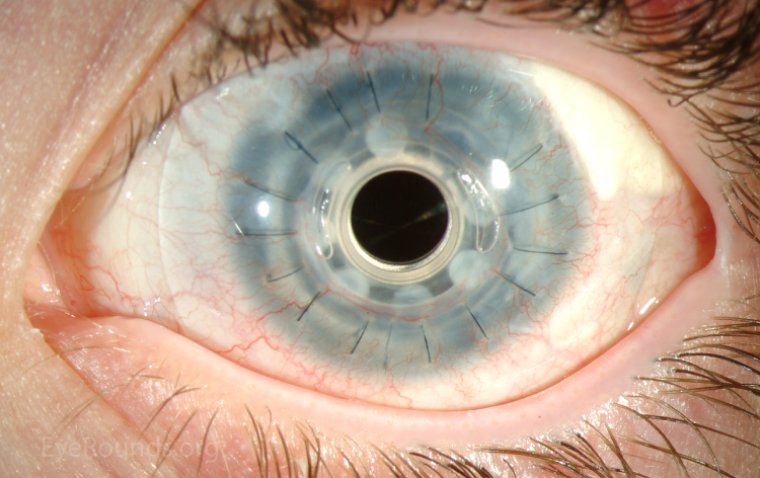
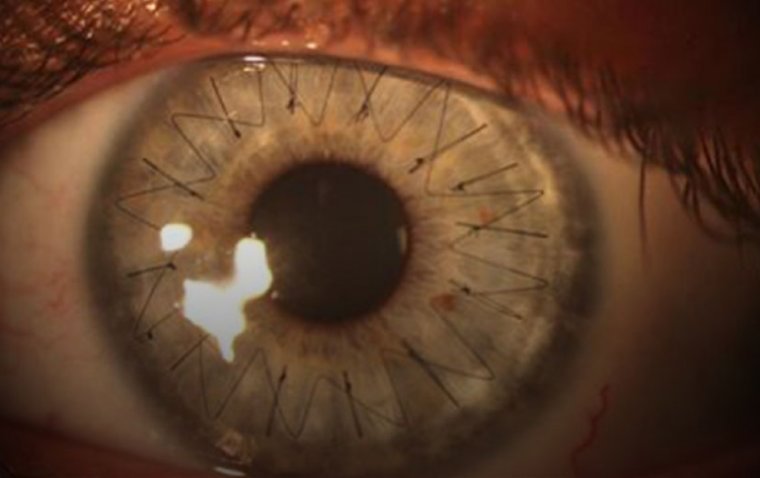
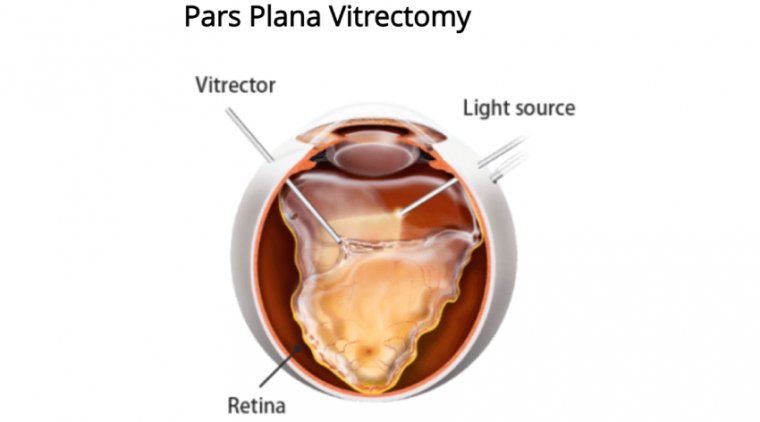
3. Surgery: In rare cases, when medications are not effective in controlling inflammation or complications arise, surgical intervention may be necessary. Procedures such as a vitrectomy, which involves the removal of the vitreous humor, or an implantation of a corticosteroid-releasing device may be considered.
Management of Uveitis-Related Complications:
1. Glaucoma: Uveitis can cause increased intraocular pressure, leading to glaucoma, a condition that can damage the optic nerve and cause vision loss. If glaucoma is detected, eye drops or other medications may be prescribed to lower intraocular pressure. In some cases, surgery may be necessary to manage glaucoma.
2. Cataracts: Prolonged inflammation or the use of corticosteroids can cause cataract formation, a clouding of the eye's natural lens. If cataracts significantly impact vision, cataract surgery may be recommended to replace the affected lens with an artificial one.
3. Posterior segment complications: In some cases, uveitis can lead to complications involving the retina or the choroid, such as retinal detachment, macular edema, or choroidal neovascularization. These complications may require specialized treatment, including laser therapy, anti-vascular endothelial growth factor (VEGF) injections, or surgery.
Conclusion
As we bring this eye-opening journey to a close, let's not lose sight of the crucial points we've covered on anterior uveitis. Whether it's caused by infections, autoimmune diseases, or trauma, it's clear that this condition can be a real eye-sore. Identifying the symptoms, seeking timely diagnosis, and adhering to appropriate treatment plans are the keys to keeping our vision as sharp as a hawk's.
Let's not blink away from the responsibility of raising awareness about anterior uveitis. After all, knowledge is power, and being well-informed about this condition can help us "see" it coming. Early detection and treatment are vital to prevent complications and preserve our precious gift of sight. So, let's keep our eyes peeled for the signs of uveitis and encourage those around us to do the same. Together, we can focus on a future where uveitis won't cloud our horizons, and our eyes can continue exploring the world around us, free from the grip of inflammation.
FAQ
In rare cases, anterior uveitis can cause blindness if left untreated or if it is not properly managed.
(1).jpg)