The Blurred Horizon: Understanding Myopia
Have you ever wondered why some people have difficulty seeing objects in the distance while others can see them clearly? Myopia, also known as nearsightedness, is a common vision problem affecting millions worldwide. Myopia is a condition where a person can see objects clearly when they are close, but objects far away appear blurry.
The condition has become increasingly prevalent, especially among children, and there is a growing concern about the impact of myopia on people's quality of life. In this article, we will explore what myopia is, its prevalence worldwide, and some factors contributing to its development.
What Is Myopia?
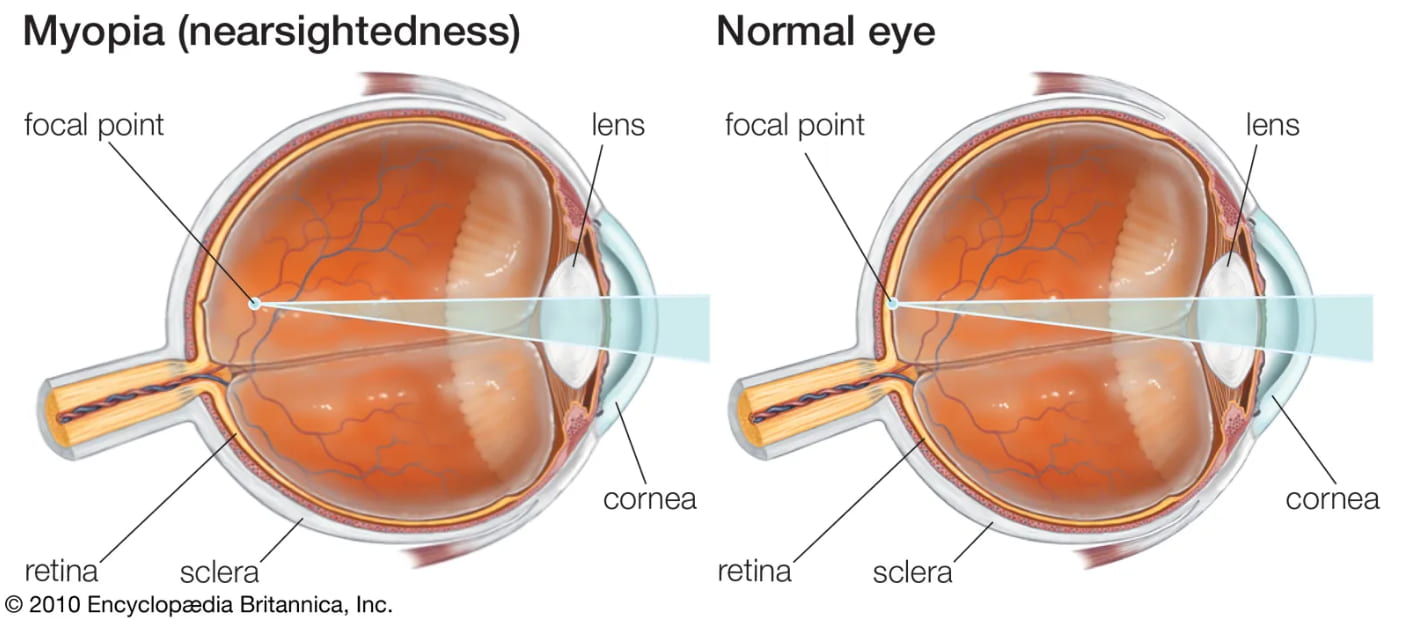
Myopia occurs when the eyeball is too long or the cornea or lens is too curved, which causes light to focus in front of the retina instead of on it. This causes distant objects to appear blurry while nearby objects appear clear. Environmental factors such as spending too much time indoors or doing close-up work, such as reading, writing, or using electronic devices, can increase the risk of developing myopia.
Prevalence of Myopia Worldwide
Myopia has become increasingly prevalent worldwide, and it is estimated that half of the world's population will be myopic by 2050. Myopia is as high as 90% among young adults in some countries. The highest rates of myopia are found in East and Southeast Asia, where up to 80% of young adults have myopia. In the United States, myopia affects about 30% of the population. The prevalence of myopia is higher in urban areas, and studies have shown that it is increasing rapidly among children in both developed and developing countries.
What Causes Myopia?
Myopia occurs when the eyeball is too long, causing light to focus in front of the retina instead of on it. This results in distant objects appearing blurry while nearby objects remain clear. However, what causes the eyeball to elongate in the first place? Genetics play a significant role in myopia development, and myopic parents' children are more likely to develop the condition.
However, environmental factors such as spending too much time indoors or doing close-up work, such as reading, writing, or using electronic devices, can also increase the risk of myopia. Understanding the factors contributing to myopia development can help us take steps to prevent or manage the condition, so let us dive deeper into this fascinating topic.
Symptoms of Myopia
Myopia can have a significant impact on a person's daily life. Left uncorrected can lead to eye strain, headaches, and difficulty performing daily tasks such as driving or reading.
Here are some common symptoms of myopia:
1. Difficulty seeing objects at a distance: One of the primary symptoms of myopia is difficulty seeing objects far away. For example, you may need help reading road signs or seeing the chalkboard in a classroom.
2. Eye strain and headaches: When you have myopia, your eyes work harder to focus on objects in the distance. This can lead to eye strain and headaches, especially after extended periods of reading, writing, or using electronic devices.
3. Squinting or blinking to see more clearly: When you have myopia, you may squint or blink frequently to see objects in the distance more clearly. This is because squinting reduces the amount of light entering the eye, making it easier to focus.
Myopia vs Hyperopia
Treatment Options for Myopia
Myopia, or nearsightedness, can be treated in various ways depending on the severity of the condition. Here are some standard treatment options for myopia:
1. Corrective lenses: Eyeglasses or contact lenses can be prescribed to correct myopia. The lenses help bend the light entering the eye to focus on the retina, allowing clear vision.
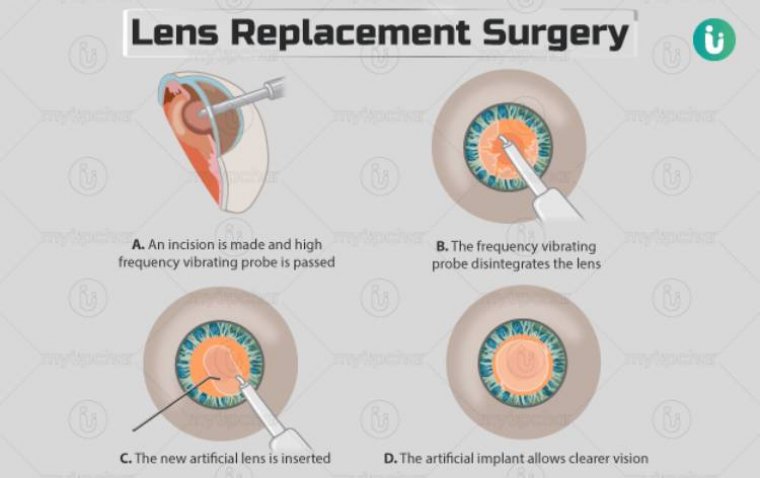
2. Refractive surgery: Refractive surgery is an option for those who want a permanent solution. Two common types of refractive surgery are LASIK (Laser-Assisted In Situ Keratomileusis) and PRK (Photorefractive Keratectomy). Both surgeries reshape the cornea to correct myopia.
3. Lifestyle changes: Certain lifestyle changes can help prevent myopia from worsening or slowing its progression. Spending more time outdoors and taking frequent breaks from close-up work, such as reading or using electronic devices, can help prevent myopia from developing or progressing.
Managing Myopia
Myopia can significantly impact a person's quality of life if left untreated. Fortunately, there are various ways to manage myopia and prevent its progression. Here are some tips for managing myopia:
● Regular eye and vision screenings: These exams can help detect myopia and other eye problems early. Eye doctors can also monitor the progression of myopia and recommend appropriate treatment options.
● Importance of early detection and treatment: Early detection and treatment of myopia are crucial in preventing complications and improving quality of life. The earlier myopia is detected, the more effective the treatment will likely be.
Tips for Maintaining Eye Health and Preventing Myopia Progression
Certain lifestyle changes can help prevent myopia from worsening or slowing its progression. Spending more time outdoors, taking frequent breaks from close-up work, such as reading or using electronic devices, maintaining a healthy diet, and getting enough sleep can all help maintain eye health and prevent myopia from progressing.
Conclusion
In conclusion, myopia is a common vision problem affecting millions worldwide. Genetic and environmental factors can cause the condition, and its prevalence is increasing, especially among children. The symptoms of myopia include difficulty seeing objects in the distance, eye strain, and headaches. However, myopia can be managed through various treatment options, including corrective lenses, refractive surgery, and lifestyle changes.
Maintaining regular eye exams and vision screenings is essential to detect myopia early and managing it effectively. If you are experiencing any symptoms of myopia, it is essential to seek professional advice from an eye doctor. Early detection and treatment of myopia can help prevent complications and improve your overall quality of life.
Remember to maintain healthy eye habits and prevent myopia from worsening, such as spending more time outdoors, taking frequent breaks from close-up work, and maintaining a healthy lifestyle. Doing so can protect your vision and maintain your eye health for years.
(1).jpg)
.PNG)