Revolutionizing Eye Care: The Role of 3D Printing Today and Tomorrow
In the realm of medical innovation, 3D bioprinting technology marks a revolutionary stride, particularly in ophthalmology. This advancement addresses the global challenge of corneal blindness, exacerbated by a critical shortage of donors, by offering groundbreaking solutions that could redefine eye care and surgery. The ability of 3D bioprinting to fabricate complex tissue constructs holds the promise of overcoming limitations in current treatments and enhancing patient outcomes.
What is 3D Bioprinting in Ophthalmology?
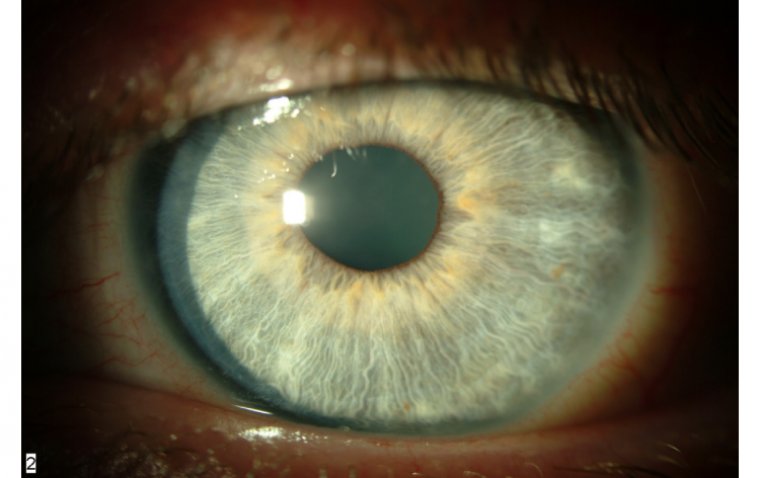
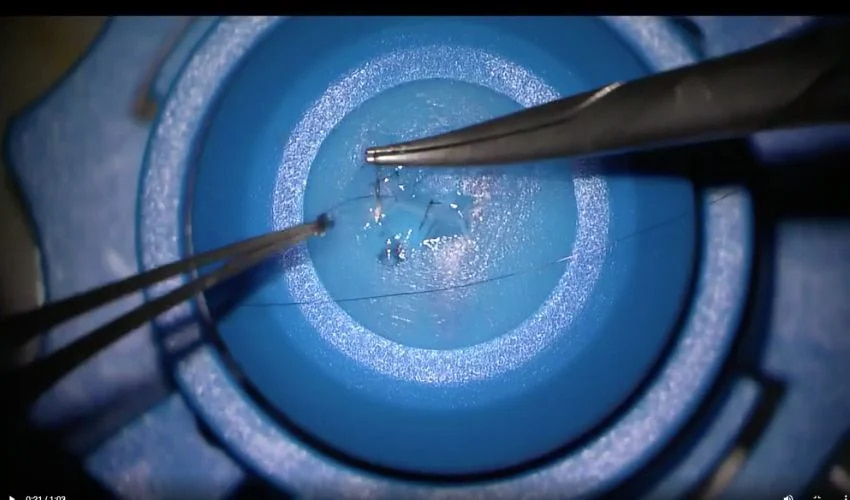
3D bioprinting has emerged as a significant innovation, particularly in creating tissue constructs that mimic the intricacies of human organs. In ophthalmology, this technology presents a novel solution to the perennial issue of corneal donor shortages. By utilizing cells combined with suitable biomaterials, 3D bioprinting can generate corneal tissues layer by layer with micrometre precision, potentially restoring vision to millions worldwide without the need for traditional donor tissues.
Categories of 3D Printing Technologies
1. Stereolithography (SLA)
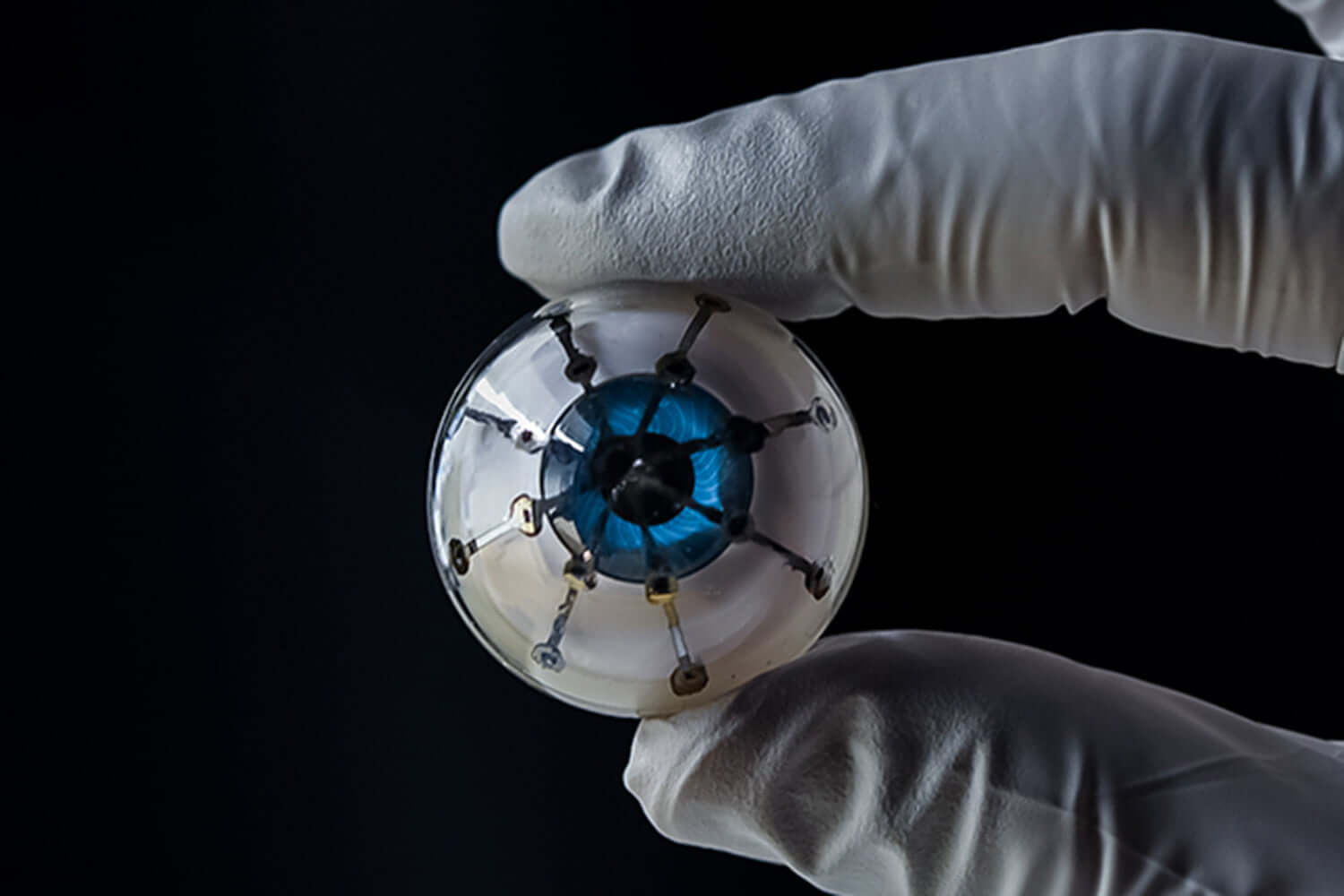
Stereolithography, or SLA, stands as a vat-polymerization technology distinguished by its use of a vat of liquid photopolymer resin. This resin is selectively exposed to curing radiation guided by a computer-aided design (CAD)-controlled process. As the build platform within the vat adjusts in height, layers are successively added atop one another. Following the printing process, the object is extracted from the drained vat. A noteworthy variant, Digital Light Processing (DLP), enhances efficiency through the use of a digital light projector to simultaneously cure entire layers, markedly accelerating the printing time compared to traditional SLA methods. Discover a faster, cheaper 3D printing technique for artificial eyeballs that further exemplifies the impact of these technologies in ophthalmology.

2. Fused Filament Fabrication (FFF)
Fused Filament Fabrication, also known as Fused Deposition Modeling (FDM), employs a material-extrusion technology. It operates by heating thermoplastic material to a semi-molten state and extruding it onto a build platform, where it solidifies upon cooling. This layer-by-layer method incrementally constructs the part until completion, with the build platform's descent facilitating the addition of successive layers.
.jpg)
3. Selective Laser Sintering (SLS)
Selective Laser Sintering utilizes a powder bed fusion (PBF) process, employing a thermal energy source to selectively sinter powder particles in a designated build area, thus solidifying them into a coherent structure. The surrounding unsintered powder acts as a support, obviating the need for additional support structures and allowing for intricate designs to be created without compromise.
.jpg)
Applications of 3D Printing in Ophthalmology
1. Corneal Tissue Engineering
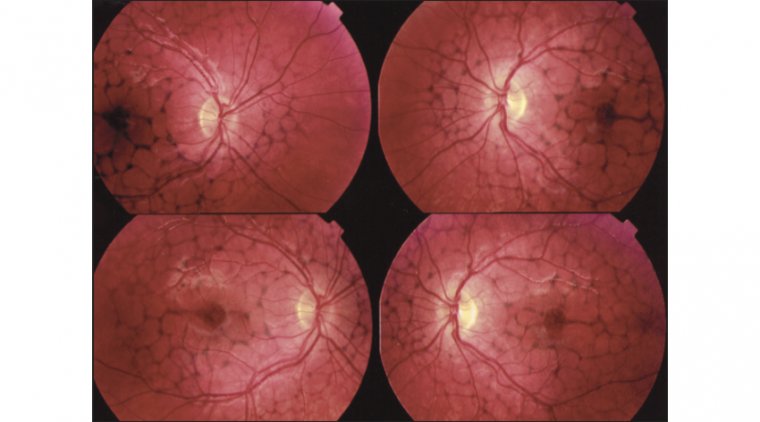
The bioprinting process for corneal tissues involves a meticulous combination of biomaterials and human proteins to create constructs that replicate the native cornea's stroma and epithelium. Recent studies have successfully demonstrated the feasibility of this approach, highlighting the technology's ability to mimic the cornea's distinct layers and functions. These advancements underscore the potential of 3D bioprinting in producing highly biocompatible and functional corneal replacements, offering a beacon of hope for those suffering from corneal blindness.
2. From Drug-Eluting Implants to MIGS Devices
Beyond corneal bioprinting, 3D printing technology is revolutionizing the development of drug-eluting implants and Minimally Invasive Glaucoma Surgery (MIGS) devices. These innovations promise more efficient drug delivery directly to the eye, reducing the need for systemic medications and their associated side effects. MIGS devices, enhanced by 3D printing, offer tailored treatments to alleviate intraocular pressure in glaucoma patients, illustrating the technology's versatility across various ophthalmic conditions. Innovations like the microscale eye implant to treat diabetes showcase the breadth of 3D printing's impact.
3. Customized Solutions for Eye Care
Personalization stands at the core of 3D bioprinting's appeal, particularly in producing customized contact lenses and spectacles. This customization not only improves the fit and comfort for patients but also optimizes the therapeutic and corrective functions of these devices. By addressing individual patient needs and anatomical variations, 3D printing fosters enhanced outcomes in eye care, setting a new standard for personalized medicine in ophthalmology. The development of a navigation function for 3D printed smart contact lenses represents a remarkable stride towards this future.
Advantages of 3D Printing in Ophthalmology
● Customization for Patient-Specific Needs: 3D printing allows for the creation of custom-designed medical devices and implants tailored to the unique anatomical requirements of individual patients. This customization is particularly beneficial in ophthalmology for producing personalized ocular prostheses and implants that perfectly match the patient's eye structure, leading to improved comfort and functionality.
● Rapid Prototyping: With 3D printing, ophthalmologists and researchers can quickly move from design to prototype, allowing for faster development and testing of new ophthalmic devices, surgical tools, and treatment methods. This rapid turnaround is crucial for advancing ophthalmic care and introducing innovations into clinical practice more swiftly.
● Complex Geometry Capabilities: The ability to produce devices with complex geometries that are difficult or impossible to achieve with traditional manufacturing methods. This advantage is significant for creating intricate ocular implants and custom surgical instruments, enhancing the precision and effectiveness of ophthalmic surgeries.
● Cost-Effectiveness for Small Batch Production: 3D printing is cost-effective for small batch production, making it an ideal solution for producing specialized ophthalmic equipment and implants that may not require mass production. This cost efficiency extends to research settings, where bespoke tools and models can be produced at a lower cost compared to traditional manufacturing.
● Educational Models for Training and Surgical Planning: 3D printing can create detailed anatomical models of the eye and orbit, which are invaluable for educational purposes, training new surgeons, and planning complex ophthalmic surgeries. These models allow for a hands-on learning experience and help surgeons visualize and practice procedures before performing them on patients.
Limitations of 3D Printing in Ophthalmology
● Limited Material Selection for Medical Use: The range of materials suitable for medical applications, especially those that can be safely implanted in the body, is relatively limited. This restricts the types of devices and implants that can be produced for ophthalmic use, potentially limiting the application of 3D printing in creating certain types of ophthalmic implants.
● Printing Resolution and Surface Finish: While 3D printing can produce detailed structures, the resolution and surface finish of printed objects may not always meet the extremely high standards required for some ophthalmic applications. Post-processing to improve the surface quality of printed items can be time-consuming and may not always achieve the desired results.
● Regulatory and Safety Concerns: The use of 3D-printed medical devices in ophthalmology faces regulatory hurdles, as each new device or implant must undergo stringent testing and approval processes to ensure its safety and efficacy. The evolving nature of 3D printing technology can make regulatory compliance challenging.
● Cost and Accessibility of High-Quality Printers: While 3D printing offers cost advantages in certain areas, the initial investment in high-quality printers capable of producing medical-grade devices can be significant. Accessibility to this technology may be limited in some regions or institutions, restricting its benefits to a wider audience in the field of ophthalmology.
● Technical Expertise Required: Successfully implementing 3D printing in ophthalmology requires technical expertise not only in the use of printers but also in design and material science. The need for specialized skills can be a barrier to adopting 3D printing technology more widely within the field.
What the Future Holds for 3D Printing in Ophthalmology?
1. Customized Solutions for Complex Problems
One of the most exciting prospects for 3D printing in ophthalmology lies in its ability to produce tailor-made solutions for patients. Custom ocular prosthetics and patient-specific implants, designed to match the unique anatomical features of an individual’s eye, are set to enhance the effectiveness of treatments and patient satisfaction. This personalization could extend to creating bespoke contact lenses that not only correct vision but also address conditions like keratoconus with unprecedented comfort and efficacy.
2. Advancing Surgical Precision and Possibilities
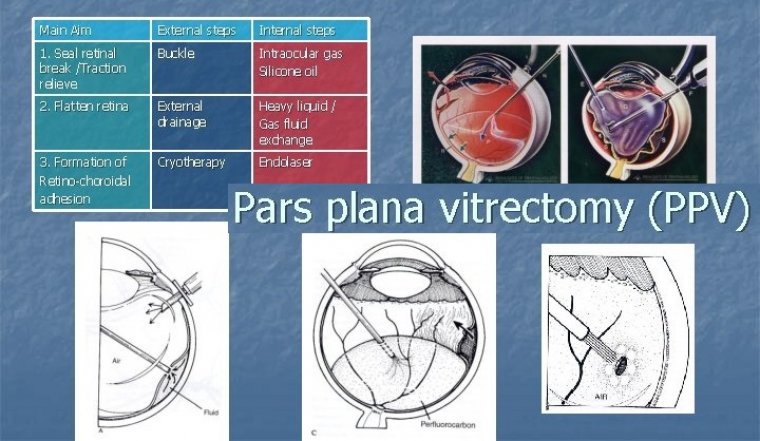
3D printing is poised to revolutionize surgical planning and execution. Detailed models of patients’ eyes, printed based on imaging data, will allow surgeons to practice and plan complex procedures, reducing risks and improving outcomes. Furthermore, the development of 3D-printed surgical instruments customized to both the procedure and the surgeon’s preferences could refine surgical techniques, potentially making surgeries safer and more successful.
3. Innovations in Drug Delivery Systems
The future may see 3D-printed devices playing a crucial role in drug delivery, offering new methods to treat conditions like glaucoma and macular degeneration. Biodegradable implants that release medication over specified periods could provide more consistent and controlled treatment regimens, reducing the need for frequent eye drops or invasive procedures.
4. Bioinks and Bioprinting: Towards Tissue Regeneration
Perhaps the most groundbreaking frontier is 3D bioprinting, which combines biological materials with printing technology to create tissue structures. The prospect of printing corneal tissue or even entire corneas could address the dire shortage of donors. Furthermore, bioprinting retinal cells offers a potential avenue for treating degenerative diseases that lead to blindness, heralding a new era of regenerative medicine in ophthalmology.
Conclusion
The future of ophthalmology is on the cusp of transformation, thanks to 3D bioprinting. As research progresses and collaborations continue to flourish, the potential to overcome existing challenges and redefine eye care is immense. The journey of 3D bioprinting from innovative concept to clinical reality illustrates the dynamic intersection of technology and medicine, heralding a new era in ophthalmology that promises restored sight and improved lives for millions around the globe. Explore more about the top eye care trends that are shaping the future of this field.
References:
https://pmc.ncbi.nlm.nih.gov/articles/PMC9247992/
https://www.sciencedirect.com/science/article/abs/pii/S1773224722007092
(1).jpg)