Steroid Treatment For Dry Eye Disease
Dry eye is related to the inflammation of ocular surface, and immune-mediated inflammation plays an important pathogenic role. Corticosteroid is an effective anti-inflammatory drug, which can rapidly and effectively relieve the symptoms and signs of moderate or severe dry eye.
Dry eye disease (DED) is a multifactorial disease of the ocular surface, characterized by a loss of homeostasis of the tear film that is accompanied by ocular symptoms.
DED is frequently associated with the instability and hyperosmolarity of tear films, inflammation of the ocular surface, and neurosensory abnormalities. DED is one of the most prevalent ocular diseases worldwide, and significantly reduces the quality of life.
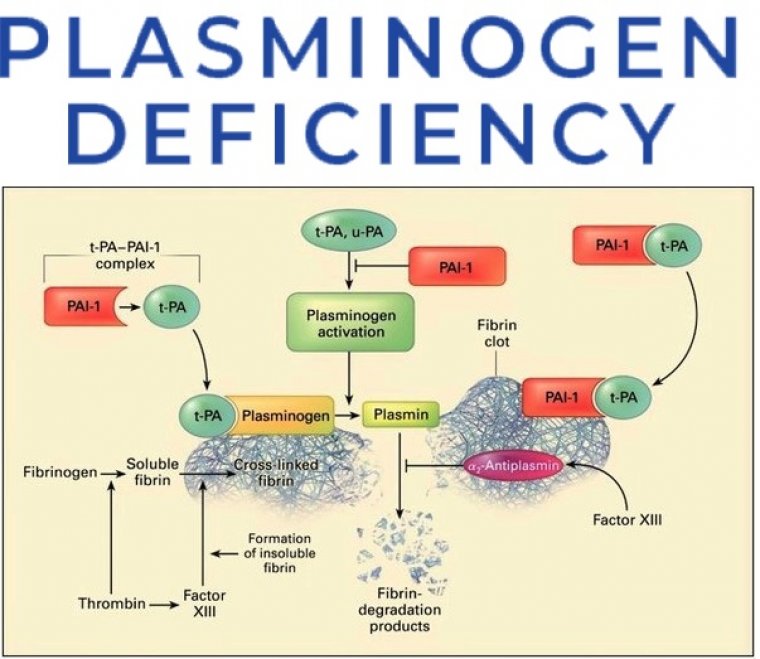
The inflammation of the ocular surface is a key component of the pathophysiology of DED. Owing to the role of inflammation in DED, numerous novel therapeutic agents have been investigated for inhibiting various inflammatory cascades.
To date, the most well-known anti-inflammatory agents approved by the US Food and Drug Administration (FDA) for the management of DED include cyclosporin A (CsA), lifitegrast (LG), corticosteroid.
Corticosteroids are widely used for the treatment of both acute and chronic inflammation, and topical corticosteroids are generally indicated for the treatment of ocular inflammatory diseases.
Corticosteroids inhibit pro-inflammatory cytokines and chemokines, stabilize macrophages and neutrophils, and repress the key enzymes involved in the initiation or maintenance of the inflammatory response.
Therefore, corticosteroids are generally thought to be more potent than other therapeutic agents for DED, including CsA, LG, and diquafosol, owing to acting on the multiple mechanisms by which corticosteroids inhibit inflammation.
Topical corticosteroids are also effective in controlling the signs and symptoms of chronic, severe DED associated with the Sjogren syndrome, and in the treatment of moderate and severe meibomian gland dysfunction (MGD).
Additionally, short-term induction therapy before long-term treatment with CsA, or combined therapy with corticosteroids and CsA, shows greater symptomatic relief and faster recovery from the signs of DED, compared to monotherapy with CsA.
Ophthalmologists can now prescribe a corticosteroid for the treatment of dry eye disease (DED) with the confidence that they are doing so on-label, following the recent United States Food and Drug Administration (FDA) approval of a topical corticosteroid for short-term (up to 2 weeks’) use.
Loteprednol etabonate ophthalmic suspension 0.25% (Eysuvis, Kala Pharmaceuticals) has a favourable adverse effect profile and a unique mechanism of action that is worth a closer look.
The drug product was studied in the largest clinical programme in DED to date, including more than 2,800 patients.
In results from the STRIDE 1 and STRIDE 2 trials conducted by Kala Pharmaceuticals, it illustrated a beneficial safety profile, demonstrating similar intraocular pressure (IOP) levels to the vehicle arm.
In treatment and vehicle groups, respectively, 0.2% and 0% of participants experienced a 10 mm Hg or greater increase from baseline, resulting in an IOP measurement of 21 mm Hg or greater at any post-baseline visit up to 29 days.
In the STRIDE trials, investigators observed statistically significant improvement in the measures of conjunctival hyperaemia and patient-reported ocular discomfort severity scores.
Participants assigned to treatment with the loteprednol etabonate suspension product experienced rapid relief, with improvement in symptoms as early as Day
The ophthalmic suspension has a novel formulation which utlises Kala Pharmaceuticals’ proprietary mucus-penetrating particle technology. These nanoparticles of approximately 300 nm in diameter are coated to facilitate their penetration through the mucus barrier.
This controlled delivery system enables the drug to spread more uniformly on the ocular surface to achieve longer retention and allow enhanced penetration to the target tissues, specifically the cornea and the conjunctiva.
The formulation has demonstrated broad-spectrum anti-inflammatory action, leading to a more efficient and effective nanoparticle drug that rapidly reduces the symptoms and signs of DED, including in those patients with periodic acute exacerbations of worsening symptoms referred to as dry eye flares.
Relieving chronic disease and flares DED is an inflammatory disease in which an unstable and hyperosmolar tear film sets off a cascading sequence of inflammatory activity on the ocular surface.
As with other chronic inflammatory conditions, such as asthma and rheumatoid arthritis, most patients with DED have chronic disease with dry eye flares.
The Tear Film & Ocular Surface Society
Dry Eye Workshop II notes that patients can initially present with episodic dry eye in the absence of chronicity.
Myriad triggers with varied intensity such as wind; low humidity; air conditioning; prolonged reading/visual tasks; and exposure to increased ozone concentrations have been shown to increase the incidence of flares.
These inflammatory spikes occur in approximately eight out of 10 patients with dry eyes, and approximately half of patients with DED experience fl ares without continuous symptoms fourto-six times per year.
Particularly in relation to the COVID-19 pandemic, I have seen more patients presenting with acute dry eye symptoms who have never before been symptomatic. Many are spending 10–12 hours a day staring at computer screens.
Additionally, the data show that there is an under-diagnosis and under-recognition of DED overall. In general, we prescribe loteprednol etabonate ophthalmic suspension 0.25% for patients who have periodic exacerbations of dry eye, including those who are self-medicating with artifi cial tears, those with ocular allergies, or those with contact lens-associated issues; patients with chronic DED who need induction therapy to quell surface inflammation quickly in order to initiate chronic therapy; and patients with breakthrough dry eye fl ares who are on chronic therapy.
Recent Cases
Two recent examples from our practice are discussed as follows. Case 1 - A 42-year-old female contact lens wearer was referred to us for consultation for dry eye due to irritation from dust created by construction work on a nearby office.
She had swelling in the left eye, with severe discomfort and complaints of dryness in both eyes for 5 weeks, and it was getting progressively worse.
The patient had initially been placed on tobramycin-dexamethasone 0.3%/0.1% twice a day and had a 95% improvement within the fi rst week; however, on re-examination, her IOP had gone up to 35 mm Hg.
She was then prescribed brimonidine-timolol 0.2%/0.5% (Combigan, Allergan) to decrease the pressure. However, her symptoms worsened when she had an allergic reaction to the brimonidine-timolol 0.2%/0.5%.
Although the drops were discontinued, her symptoms continued to worsen, with significant discomfort and redness, and she needed artificial tears every hour. By the time she saw us, it was her 11th visit to a doctor in 5 weeks and she was desperate for relief.
We gave her a diagnosis of allergic conjunctivitis, contact lens overwear and dry eyes. We discontinued all previous drops and put her on loteprednol etabonate ophthalmic suspension 0.25% every other day, four times a day, for 2 weeks; preservative-free tears four times a day; and extra-strength over-thecounter olopatadine 0.7% (Pataday, Alcon) twice a day.
Within 1 week, she had great improvement in all her symptoms and felt that her eyes were back to normal. She completed the treatment course with full resolution of her symptoms and, much to her relief (and that of her referring provider), no increase in IOP.
Case 2 - A 78-year-old woman with a variety of medical problems including multiple myeloma and colon cancer was referred for evaluation of severe dryness in both eyes.
In particular, she was experiencing copious tearing from her right eye for the past several weeks, stating that her eye watered so much it felt as though she was looking through a “puddle”.
The patient had been taking cyclosporine ophthalmic emulsion 0.05% (Restasis, Allergan) for years, which she felt helped her, and recently had been given lifitegrast ophthalmic solution 5% (Xiidra, Novartis) to use in addition to Restasis, but she was still experiencing tearing.
She was also using artificial tears, warm compresses and over-the-counter olopatadine 0.1% for allergic conjunctivitis. On examination, the patient had evidence of chronic inflammation including conjunctivochalasis and corneal staining.
We kept her on cyclosporine ophthalmic emulsion 0.05% and added loteprednol etabonate ophthalmic suspension 0.25% in both eyes four times a day for 2 weeks. Within days, her tearing resolved and her vision improved from 20/40 to 20/25.
The patient was very happy that she was no longer tearing and was thrilled with the improvement in vision.
When it comes to prescribing corticosteroids for DED, we are much more proactive and confident prescribing loteprednol etabonate ophthalmic suspension 0.25% for our patients because of its rapid onset and strong safety profile.
We have had great success with the drop in many straightforward to complex cases, including patients with glaucoma, and have had no pressure increases measured at follow-up examination in our clinical experience so far.
The patients are impressed by how quickly the ophthalmic suspension works to quieten symptoms. Having an on-label enhanced loteprednol formulation for shortterm use in treating the signs and symptoms of DED is a welcome addition to our armamentarium.
Dry eye can have a significant impact on patient quality of life and daily activities. Patients are extremely grateful and relieved to feel rapid relief from their DED symptoms, especially when they experience dry eye flares.
(1).jpg)