Researchers at the National Institutes of Health have significantly advanced retinal imaging by inte...
read moreLenz Therapeutics announced positive topline results from its Phase 3 CLARITY study, evaluating two ...
read moreResearchers discovered that individuals vary significantly in their ability to perceive visual signa...
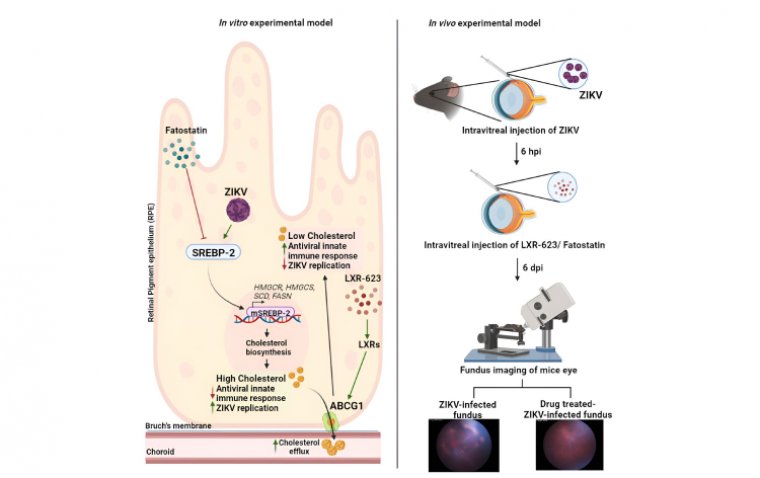
read moreResearchers at Wayne State University School of Medicine have published a study in the journal iScie...
read moreRegenxbio Inc. announced the publication of their phase 1/2a study results in The Lancet, showcasing...
read moreAurion Biotech recently administered its novel cell therapy, AURN001, to the first Canadian particip...
read moreNanoscope Therapeutics announced positive topline results from the phase 2b RESTORE trial, evaluatin...
read moreOpus Genetics recently completed the first stage of its innovative clinical trial, focusing on a new...
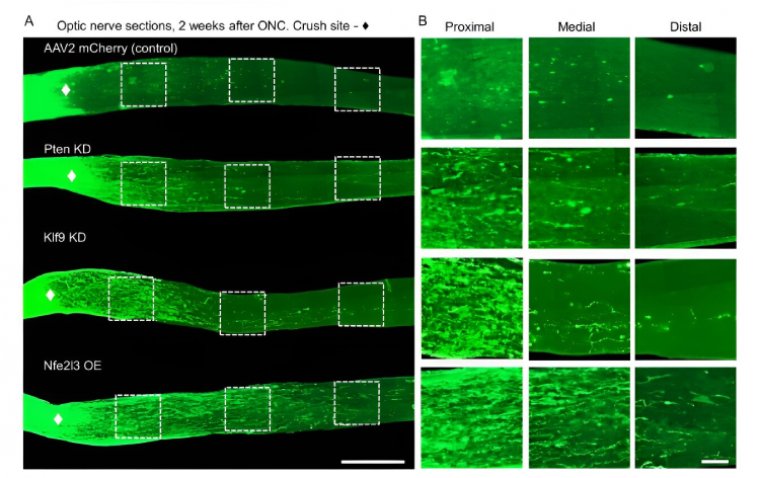
read moreResearchers at the University of Connecticut (UConn) have identified a potentially transformative fa...
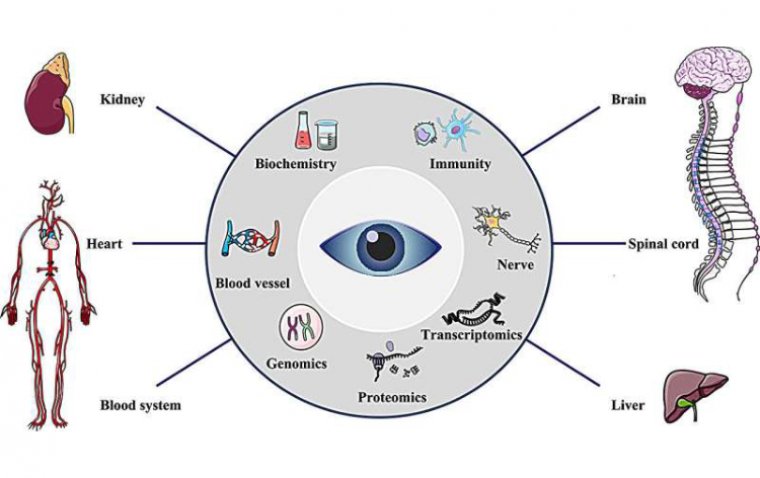
read moreResearchers from Macau University of Science and Technology sheds light on the intersection of ophth...
read more More
More