Toddler Vision Test Enhances Early Detection of Eye Disorders
Standard vision assessments used for older children and adults are unsuitable for toddlers, especially those under three years of age, due to the cognitive and verbal skills required. To address this critical gap, researchers at the School of Optometry & Vision Science at the University of Waterloo have developed the Waterloo Differential Acuity Test (WatDAT), a novel approach that allows precise visual acuity measurement in very young children.
Prevalence and Impact of Early Childhood Eye Disorders
Approximately 14% of children aged two to four are affected by vision conditions such as amblyopia (lazy eye), clinically significant hyperopia (farsightedness), or astigmatism. In some cases, rarer issues such as pediatric cataracts may disrupt normal visual development. Because children at this age cannot articulate vision problems, and symptoms may not be outwardly visible, many cases go undiagnosed during crucial developmental windows.
“These vision problems are not always noticeable by observing a child. Also, children will not complain about poor vision because they don't know what good vision is,” said Dr. Susan Leat, professor emeritus and lead researcher.
Dr. Leat emphasized that earlier and more accurate detection could lead to more effective treatment outcomes.
Limitations of Existing Pediatric Vision Tests
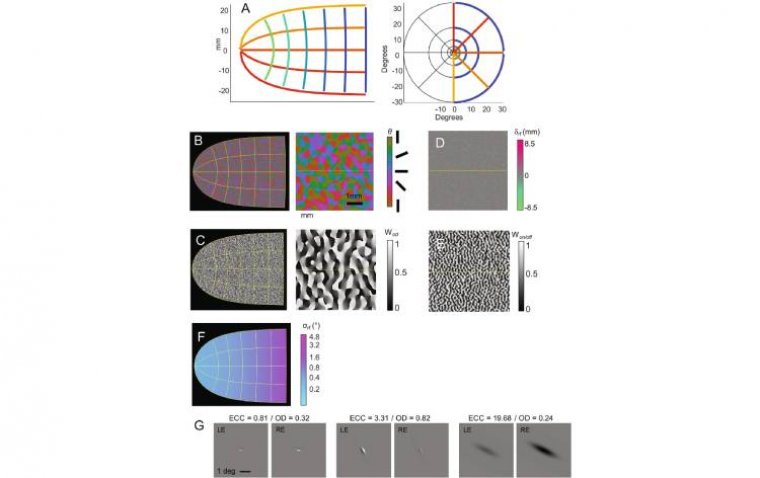
Current methods for testing babies and toddlers rely on eye movement tracking, such as measuring preference for striped versus blank patterns. However, this approach only determines if a child can see a pattern, not whether they can distinguish fine detail, which is vital for diagnosing specific visual impairments.
For children over three, optometrists often use picture-naming or matching tasks to determine visual acuity. These require verbal or cognitive engagement that younger toddlers may not be capable of, limiting their effectiveness.
How WatDAT Works
WatDAT introduces a simplified, recognition-based task suitable for children as young as 18 months. The test displays four shapes, three of which are identical (e.g., three circles and one house). The child is asked to point out the shape that is different, and the task is repeated with progressively smaller images until the child can no longer identify the odd one.
This structure requires less cognitive demand than standard tests, allowing for broader accessibility. In the study, all children aged 24 months and older who were meeting typical developmental milestones successfully completed the test with both eyes.
Comparison with Existing Pediatric Tests
Researchers found that WatDAT outperformed two commonly used pediatric vision tests in terms of age accessibility, with more children able to complete the assessment at younger ages. All three tests required similar testing time, making WatDAT both efficient and effective.
Even among a subset of participants with vision or health impairments or those born preterm, most were able to complete the WatDAT protocol successfully.
Broader Potential in Vision Testing
“We believe WatDAT could be a useful tool in testing the vision of people of all ages who have intellectual and developmental disabilities,” said Dr. Supriya Aryal, a recent optometry graduate and research contributor.
Dr. Aryal also noted that WatDAT may have future applications in low vision assessment across age groups, although further research is needed to confirm this use.
Digital and Printed Formats in Beta Testing
WatDAT is currently in beta testing in Canada, the United States, and the United Kingdom. Optometrists report that children enjoy the test because it resembles a game. The digital version includes animated rewards for correct answers, while the print version is optimized for use in traditional clinic settings.
Researchers plan to commercialize WatDAT following the completion of beta testing.
Reference:
S. Aryal et al, The Waterloo Differential Acuity Test (WatDAT)—Testability and normative data, Ophthalmic and Physiological Optics (2025). DOI: 10.1111/opo.13565
(1).jpg)