Keratoconjunctivitis: Symptoms, Causes, and Treatment Options
Picture this: You're enjoying a beautiful sunny day when suddenly, your eyes start to itch, turn red, and feel like there's a tiny grain of sand stuck in them. If this scenario sounds all too familiar, you might be one of the many people affected by keratoconjunctivitis, a prevalent eye condition that can put a damper on even the brightest of days.
In this comprehensive article we'll delve deep into the world of this common yet often misunderstood eye condition that affects both the cornea and conjunctiva. With its far-reaching implications on our daily lives, understanding keratoconjunctivitis is essential not just for eye care professionals but for anyone who values clear, comfortable vision.
From identifying tell-tale symptoms to exploring the various causes and risk factors, this article will provide you with the knowledge you need to recognize and manage keratoconjunctivitis effectively. We'll also shed light on the latest treatment options, offering hope for a brighter, irritation-free future.
So, join us as we embark on an enlightening journey to unravel the mysteries of keratoconjunctivitis, a condition that has a significant impact on the quality of life for millions worldwide. It's time to open our eyes to the reality of this pervasive eye problem and learn how we can fight back for the sake of our precious vision.
What Is Keratoconjunctivitis?
Keratoconjunctivitis is an eye condition characterized by the simultaneous inflammation of the cornea (keratitis) and the conjunctiva (conjunctivitis). This inflammation can lead to a range of uncomfortable symptoms and, in some cases, may cause damage to the eye if left untreated. To fully grasp the nature of this condition, let's take a closer look at its key components and risk factors.
The cornea is the clear, dome-shaped outer layer of the eye that plays a crucial role in focusing light onto the retina. The conjunctiva, on the other hand, is a thin, transparent membrane that covers the white part of the eye (the sclera) and lines the inside of the eyelids. Both of these structures are essential for maintaining the health and function of the eye.
Keratoconjunctivitis occurs when irritants, allergens, infections, or other factors cause both the cornea and conjunctiva to become inflamed. This dual inflammation can result in symptoms such as redness, itching, tearing, blurred vision, and a gritty or burning sensation in the eyes.
The risk of developing keratoconjunctivitis can vary depending on factors such as age, immune system function, exposure to irritants or allergens, and contact lens use. Individuals with a history of allergies or those who frequently work in environments with high levels of dust, chemicals, or other irritants may be more susceptible to this condition. Additionally, people with compromised immune systems, dry eye syndrome, or a history of eye trauma or surgery may also be at an increased risk.
Types of Keratoconjunctivitis
Symptoms of Keratoconjunctivitis
1. Eye redness: Inflammation of the cornea and conjunctiva can cause the eyes to appear red or bloodshot.
2. Itching: Irritation caused by keratoconjunctivitis often leads to an uncomfortable itching sensation.
3. Tearing: Excessive tearing or watery discharge is a common symptom, particularly in viral and allergic keratoconjunctivitis.
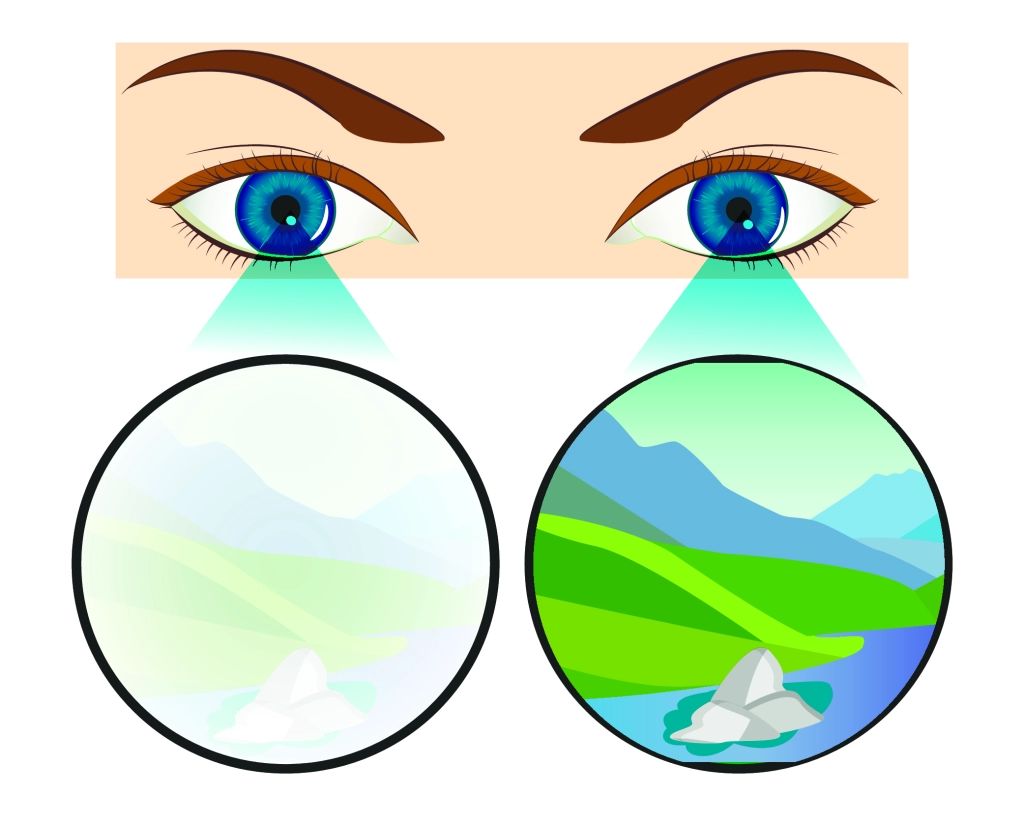
4. Blurred vision: Inflammation and discharge can cause temporary blurring of vision.
5. Swelling: In some cases, the eyelids or surrounding tissue may become swollen and puffy.
6. Pain or discomfort: Patients may experience a burning, stinging, or gritty sensation in their eyes.
7. Light sensitivity: Keratoconjunctivitis can make the eyes more sensitive to light, causing discomfort or pain in bright environments.
Severe symptoms and complications may occur if keratoconjunctivitis is left untreated, including:
● Corneal scarring or ulceration: Persistent inflammation can lead to damage to the cornea, potentially resulting in scarring or even ulceration.
● Infection spread: Untreated bacterial or viral keratoconjunctivitis can spread to other parts of the eye or to other individuals.
● Chronic conjunctivitis: Prolonged inflammation may result in long-lasting or recurring conjunctivitis, which can impact the quality of life.
● Vision loss: In extreme cases, untreated keratoconjunctivitis may lead to vision loss due to corneal damage or complications from severe infections.
Causes of Keratoconjunctivitis
1. Viral infection: Commonly caused by adenoviruses, viral keratoconjunctivitis is highly contagious and spreads through direct contact or contaminated surfaces.
2. Bacterial infection: Bacterial keratoconjunctivitis often results from infections by Staphylococcus aureus, Streptococcus pneumoniae, or other bacteria.
3. Allergens: Allergic keratoconjunctivitis is triggered by exposure to allergens, such as pollen, dust mites, or pet dander.
4. Chemical irritants: Exposure to chemicals, such as chlorine in swimming pools or airborne pollutants, can cause keratoconjunctivitis.
5. Dry eye syndrome: Insufficient tear production or poor tear quality can lead to keratoconjunctivitis due to a lack of proper eye lubrication.
6. Contact lens use: Improper hygiene, extended wear, or poorly fitting contact lenses can contribute to the development of keratoconjunctivitis.
7. Immune system disorders: Autoimmune conditions or a weakened immune system can increase the risk of developing keratoconjunctivitis.
8. Eye trauma or surgery: Damage to the eye or complications from eye surgery can cause keratoconjunctivitis in some cases.
Diagnosis of Keratoconjunctivitis
Diagnosing keratoconjunctivitis typically involves several steps to accurately identify the underlying cause and determine the most appropriate treatment. The diagnostic process may include:
● Clinical examination: An ophthalmologist or optometrist will conduct a thorough eye examination, evaluating the patient's symptoms, eye appearance, and any signs of inflammation or infection.
● Patient history: The healthcare professional will ask about the patient's medical history, including any past eye issues, recent infections, allergies, or exposure to irritants.
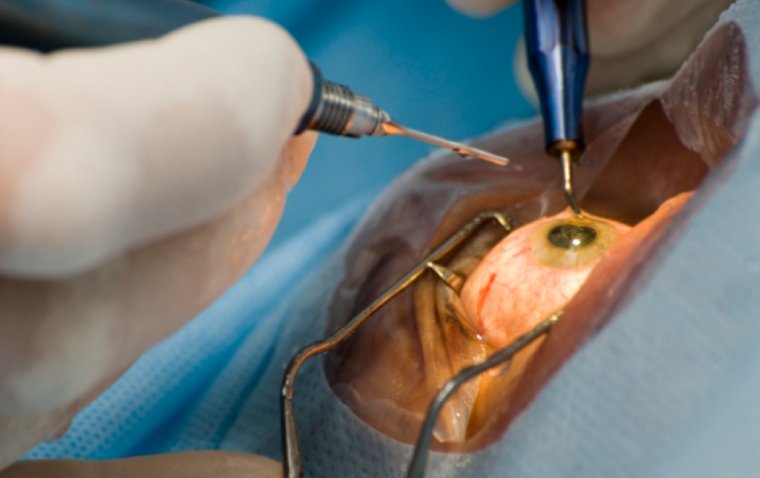
● Slit-lamp examination: Using a specialized microscope called a slit lamp, the eye care professional will closely examine the cornea, conjunctiva, and other eye structures to evaluate the extent of inflammation and identify any damage.
● Fluorescein staining: In some cases, a doctor may use a dye called fluorescein to help visualize any corneal damage or abrasions more clearly.
● Eye swab or culture: If a bacterial or viral infection is suspected, an eye swab may be taken to collect a sample for laboratory analysis and culture. This can help identify the specific organism responsible for the infection.
● Allergy testing: For patients with suspected allergic keratoconjunctivitis, skin or blood tests may be performed to identify the specific allergens responsible for the symptoms.
Once the underlying cause of keratoconjunctivitis has been identified, the eye care professional can recommend the most appropriate treatment options to manage the condition and alleviate symptoms.
Treatment Options for Keratoconjunctivitis
The treatment of keratoconjunctivitis depends on the underlying cause and severity of the condition. Some common treatment options include:
1. Artificial tears: Over-the-counter lubricating eye drops can help soothe irritation and provide relief from dryness, particularly for mild cases or dry eye-related keratoconjunctivitis.
2. Antihistamines and mast cell stabilizers: For allergic keratoconjunctivitis, antihistamine eye drops or mast cell stabilizer drops can help reduce itching, redness, and inflammation.
3. Topical corticosteroids: In more severe cases of allergic or inflammatory keratoconjunctivitis, a healthcare professional may prescribe corticosteroid eye drops to alleviate symptoms and reduce inflammation.
4. Antibiotics: For bacterial keratoconjunctivitis, a doctor may prescribe antibiotic eye drops or ointments to target the specific bacteria causing the infection.
5. Antiviral medications: In some cases of viral keratoconjunctivitis, antiviral eye drops or oral medications may be prescribed to help control the infection, particularly for more severe infections like those caused by the herpes simplex virus.
6. Proper hygiene: Maintaining good eye hygiene, such as avoiding touching the eyes, washing hands frequently, and changing pillowcases regularly, can help prevent the spread of infection and support the healing process.
7. Discontinuing contact lens use: For keratoconjunctivitis related to contact lens use, it is crucial to discontinue wearing lenses until the condition has resolved. The eye care professional may also recommend changing to a different type of lens or adjusting the lens care regimen.
Medications for Keratoconjunctivitis
1. Antiviral medications:
Used for: Treating viral keratoconjunctivitis caused by viruses such as herpes simplex or adenoviruses.
How they work: These drugs inhibit the replication of the virus, helping to control the infection and reduce symptoms.
Examples: Acyclovir, ganciclovir, or trifluridine eye drops or oral medications.
Potential side effects: Eye irritation, burning, or stinging. Oral antivirals may cause gastrointestinal issues, headache, or dizziness.
2. Antibacterial medications:
Used for: Treating bacterial keratoconjunctivitis caused by bacteria such as Staphylococcus aureus or Streptococcus pneumoniae.
How they work: These medications target and kill bacteria, helping to clear the infection and alleviate symptoms.
Examples: Erythromycin, azithromycin, or gentamicin eye drops or ointments.
Potential side effects: Eye irritation, burning, or stinging. In rare cases, an allergic reaction to the medication may occur.
3. Anti-inflammatory drugs:
Used for: Reducing inflammation and alleviating symptoms in allergic or inflammatory keratoconjunctivitis.
How they work: These medications suppress the body's immune response, decreasing inflammation and providing relief from symptoms.
Examples: Corticosteroid eye drops (e.g., prednisolone, loteprednol) or nonsteroidal anti-inflammatory drugs (NSAIDs) like ketorolac eye drops.
Potential side effects: Corticosteroids may cause increased intraocular pressure, cataract formation, or increased risk of infection with prolonged use. NSAIDs may cause eye irritation, burning, or stinging.
4. Antihistamines and mast cell stabilizers:
Used for: Treating allergic keratoconjunctivitis by targeting the allergic response.
How they work: Antihistamines block histamine receptors, reducing itching and redness, while mast cell stabilizers prevent the release of histamine and other inflammatory mediators.
Examples: Antihistamine eye drops (e.g., olopatadine, azelastine) or mast cell stabilizer eye drops (e.g., nedocromil, lodoxamide).
Potential side effects: Eye irritation, burning, or stinging. In rare cases, an allergic reaction to the medication may occur.
To conclude...
This article has highlighted the importance of understanding and recognizing the signs and symptoms of keratoconjunctivitis, a common eye condition that affects the cornea and conjunctiva. As we have explored its various types, causes, symptoms, and treatment options, it is crucial to emphasize that seeking medical attention when experiencing symptoms is vital for prompt diagnosis and effective management of the condition.
Keratoconjunctivitis can significantly impact an individual's quality of life, but with proper care and timely intervention, its symptoms can be controlled and complications prevented. By being proactive and vigilant about eye health, we can ensure that our vision remains clear and comfortable, enabling us to fully appreciate the world around us. So, don't hesitate to consult an eye care professional if you suspect you or a loved one may be suffering from keratoconjunctivitis – your eyes deserve the best care possible.
FAQ
If left untreated, severe cases of keratoconjunctivitis can lead to scarring and other permanent damage to the cornea and conjunctiva. It is important to seek prompt medical attention if you experience any symptoms of Keratoconjunctivitis.
(1).jpg)
.PNG)