Battling Reimbursement Challenges: The Largest Problem Faced by Ophthalmologists Today
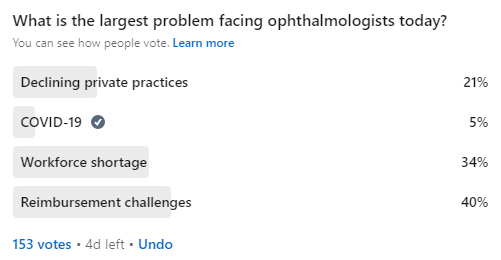
We recently conducted a survey on LinkedIn to ask ophthalmologists about the largest problem they face in their field. A total of 153 people participated in the poll, and the results revealed some interesting insights.
The top issue identified by 40% of respondents was reimbursement challenges. Reimbursement challenges can include issues such as denied claims, reduced payments, and administrative burdens, all of which can negatively impact a practice's bottom line. This can make it difficult for ophthalmologists to continue providing high-quality care, invest in new technology, or even stay in business. To address this issue, ophthalmologists could advocate for changes in reimbursement policies, explore alternative payment models, or invest in technology that streamlines the reimbursement process.
Reimbursement problems are a growing concern in medical specialties, including ophthalmology, as healthcare payers continue to cut costs. It's crucial for practitioners to stay updated on changes in insurance policies and to optimize their practice management systems to minimize claim denials. Using tools like automated billing software and third-party claim management services could improve reimbursement rates and ease the administrative burden.
Workforce Shortages: A Growing Concern for Ophthalmology Practices
The second-largest problem identified by 34% of respondents was workforce shortage. This can be a significant issue for ophthalmologists as it can lead to longer wait times for patients and a higher workload for practitioners. It can also make it difficult for practitioners to provide the same level of care they would like to offer their patients. To solve this problem, it could be important to encourage more medical students to pursue a career in ophthalmology, provide support for continuing education and professional development, and work to improve work-life balance for practitioners.
The workforce shortage in healthcare has become a major issue, especially in specialties like ophthalmology where specialized training is required. Recruitment efforts need to focus on incentivizing students to enter this field by offering scholarships, mentorship programs, and improved work conditions. Furthermore, adopting telemedicine or artificial intelligence for routine diagnostics can help ease the burden on ophthalmologists by managing some of the less critical tasks, improving efficiency, and reducing burnout.
The Decline of Private Ophthalmology Practices
Declining private practices was another concern identified by 21% of survey respondents. The ongoing trend of consolidation in the healthcare industry, along with changes in reimbursement policies, can make it difficult for independent ophthalmologists to compete with larger organizations. This can lead to a loss of autonomy, increased pressure to see more patients, and reduced ability to provide personalized care. To address this issue, private practitioners may need to explore new business models, such as forming networks or partnerships, investing in technology, or offering specialized services.
Private ophthalmology practices face increasing competition from hospital-owned groups and large medical networks, which have more resources and access to better reimbursement rates. Independent practitioners can still thrive by adopting niche services, such as offering specialized eye care procedures, forming collaborative networks with other independent practices, or even joining Accountable Care Organizations (ACOs). These strategies can help private ophthalmologists maintain their autonomy while staying competitive in a rapidly changing healthcare environment.
COVID-19’s Impact on Ophthalmology: Adapting to the New Normal
Finally, 5% of respondents identified Covid-19 as a problem. While it may not be the largest problem, the pandemic has had a significant impact on the field of ophthalmology, with many practitioners facing reduced patient volume, canceled elective procedures, and financial difficulties. The pandemic has brought about many challenges for ophthalmologists, including reduced patient volume, increased costs, and safety concerns. To address these issues, ophthalmologists may need to adapt to new ways of working, such as using telemedicine, implementing safety protocols, or finding ways to increase patient volume.
The COVID-19 pandemic forced many ophthalmology practices to adapt rapidly. The sudden drop in patient visits, especially for elective surgeries like cataract operations, led to significant financial losses. However, some practices have thrived by embracing telehealth for routine consultations, educating patients about the safety of in-person visits with strict protocols, and offering flexible scheduling for procedures. These changes are likely to shape the future of ophthalmology practices beyond the pandemic.
Addressing Reimbursement Challenges, Workforce Shortages, and Other Key Issues in Ophthalmology
These results offer a glimpse into the challenges facing ophthalmologists today. They highlight the need for ongoing efforts to address reimbursement challenges, workforce shortages, and the decline of private practices in the field of ophthalmology. By working together and finding ways to solve these problems, we can help ensure that ophthalmologists can continue to provide the highest quality of care to their patients.
Collaboration among ophthalmology professionals, policymakers, and healthcare payers will be essential in overcoming these challenges. Advocacy for better reimbursement models, workforce development initiatives, and innovative practice models will not only improve the sustainability of ophthalmology practices but also ensure continued access to high-quality eye care for patients across the globe.
(1).jpg)