Medical Breakthrough: World’s First Whole-eye and Partial Face Transplant
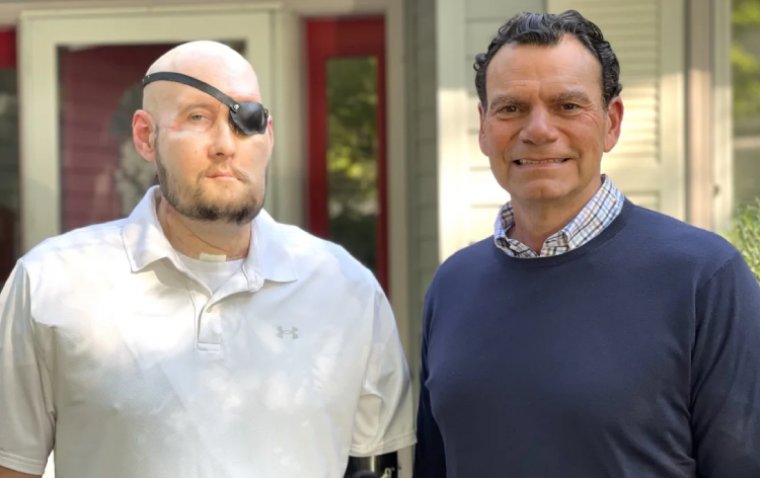
In a groundbreaking medical feat, a surgical team comprising more than 140 clinicians, including surgeons, nurses, and various healthcare professionals from New York University (NYU) Langone Health, has successfully conducted the world's first whole-eye and partial face transplantation on a 46-year-old man. The patient, identified as Aaron James, is a military veteran from Hot Springs, Arkansas, who survived a high-voltage electrical accident at work in June 2021.
The catastrophic incident, involving 7,200 volts of electricity, resulted in the loss of Mr. James's dominant left arm above the elbow, his entire nose and lips, front teeth, left cheek area, and chin down to the bone, along with the destruction of the left eye.
In a 21-hour procedure carried out in May 2023, the surgical team achieved a medical milestone by successfully transplanting the entire left eye and part of the face from a donor to Mr. James. This marks the first instance of a human whole-eye transplant combined with a partial facial transplant.
Dr. Eduardo Rodriguez, MD, DDS, the Helen L. Kimmel Professor of Reconstructive Plastic Surgery, Chair of the Hansjörg Wyss Department of Plastic Surgery, and director of the Face Transplant Program at NYU Langone, highlighted the remarkable success of the surgery. The facial transplant has exhibited no signs of rejection, a phenomenon that typically occurs in the early months post-procedure.
Furthermore, the transplanted eye is doing exceptionally well, boasting a healthy blood supply to the retina and stable intraocular pressure. Currently protected by the closed left lid to prevent exposure damage, the eye is under the expert care of Dr. Vaidehi S. Dedania, MD, a retina specialist in the Department of Ophthalmology at NYU Langone. This groundbreaking surgery not only offers hope to patients with severe facial injuries but also underscores the collaborative and innovative efforts of the medical community in advancing the frontiers of reconstructive surgery.
The clinicians are currently uncertain about the potential restoration of vision; however, a press release states that the transplanted left eye has displayed remarkable signs of health, including direct blood flow to the retina, since the procedure. While the future functionality of the eye remains unknown, the medical team believes that this groundbreaking procedure introduces new possibilities for advancements in vision therapies and related medical fields. Functional magnetic resonance imaging has revealed light stimulation in the retina during testing.
When Mr. James commenced treatment at a Texas medical center following the accident, Rodriguez and his team recommended cutting the optic nerve as close to the eyeball as possible before removing the left eye. This decision aimed to preserve as much nerve length as possible, maximizing reconstructive options and holding the hope for a potential transplant in the future. This choice sparked discussions about the unprecedented possibility of including an eye with the face in the transplantation, a concept never previously attempted.
“The mere fact that we’ve accomplished the first successful whole-eye transplant with a face is a tremendous feat many have long thought was not possible. We’ve made one major step forward and have paved the way for the next chapter to restore vision,” Rodriguez stated.
A Samer Al-Homsi, MD MBA, executive director of the Transplantation and Cellular Therapy Center, and professor in the Department of Medicine at NYU Langone added: “This is the first attempt at injecting adult stem cells into a human optic nerve during a transplant in the hopes of enhancing nerve regeneration. We chose to use CD34 positive stem cells that harbor the potential to replace damaged cells and neuroprotective properties. We have now demonstrated that the procedure is safe and potentially efficacious, but we need time to determine if this step plays a role in enhancing the chance of sight restoration, and if there’s anything further that can be done in the future to optimize the procedure.”
*Stay in the loop and make sure not to miss real-time breaking news about ophthalmology. Join our community by subscribing to OBN newsletter now.
(1).jpg)