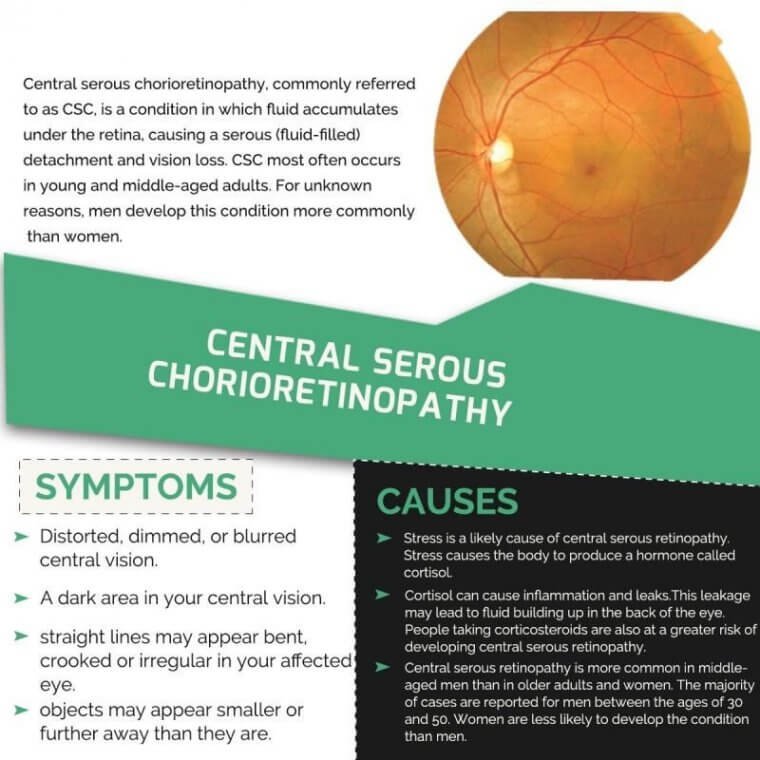
Updates On Central Serous Chorioretinopathy
Central serous chorioretinopathy, commonly referred to as CSC, is a condition in which fluid accumulates under the retina, causing a serous (fluid-filled) detachment and vision loss.
CSC most often occurs in young and middle-aged adults. For unknown reasons, men develop this condition more commonly than women. Vision loss is usually temporary but sometimes can become chronic or recur.
Central serous chorioretinopathy (CSC) is a common retina disease and has a relative high recurrence rate, etiology, and pathogenesis of which remains largely ambiguous.
The effects on the retina are usually self-limited, although some people are left with permanent vision loss due to progressive and irreversible photoreceptor damage or retinal pigment epithelium atrophy.
There have been a number of interventions used in CSC, including, but not limited to, laser treatment, photodynamic therapy (PDT), intravitreal injection of anti-vascular endothelial growth factor agents, and subthreshold lasers.
It is not clear whether there is a clinically important benefit to treating acute CSC, which often resolves spontaneously as part of its natural history. Of the interventions studied to date, PDT and micropulse laser treatment appear the most promising.
Symptoms
Blurry central vision, which often occurs in one eye, is the most common symptom that patients experience; however, careful examination often reveals some involvement in the other eye as well.
Depending on the location and amount of sub-retinal fluid, CSC can show no symptoms, especially if the affected areas fall outside of the macula—the part of the retina used to distinguish fine detail for activities like reading and recognizing faces.
Causes
The causes of CSC are not fully understood. It is thought that any systemic exposure to a corticosteroid drug can bring about or worsen CSC. Corticosteroids are found in allergy nose sprays and anti-inflammatory skin creams available over the counter, and are often prescribed to treat a variety of medical conditions.
An association has also been made between CSC and patients with emotional distress and/or “type A” personalities. It is possible that the body produces natural corticosteroids in times of stress that may trigger CSC in an individual prone to this condition.
An annual incidence of 9.9 in 100,000 in men and 1.7 in 100,000 in women was noted in the Olmstead County, Minnesota population study.
Although the underlying pathophysiology is not completely understood, it is hypothesized to be due to leakage of fluid from highly permeable choroidal vessels through the dysfunctional RPE to the subretinal layer.
There have been several advances in the area of imaging, particularly choroidal imaging, which has further enhanced the understanding of CSCR.
Advancement in multimodal imaging has been exploited, and a newer classification for CSCR has been proposed by the Central Serous Chorioretinopathy International Group.
Concurrently, clinical trials have reported results of oral medication in CSCR, and newer treatment options are being explored.
New Classifications
There is no universally adopted classification system for CSCR. However, it is important to explore the classification schemes in the literature. The goal of any clinical classification system is to predict the course of disease.
Some classification schemes have used disease duration, timing of subretinal fluid (SRF) resolution, grade of activity, spectrum of phenotypes, recurrence, and existence of a causative factor.
Conventional classification for CSCR as acute or chronic has significant discrepancies in real life. In a multicenter study, Singh et al showed a significantly poor agreement (Fleiss kappa=.218) among 6 retina experts for CSCR classification.
Thus, there is a need for a new classification system. In pursuit of a more standardized classification system, the Central Serous Chorioretinopathy International Group proposed a diagnostic criteria and classification system for idiopathic CSCR based on consensus among major experts.
They described major and minor criteria based on findings of serous retinal detachment (SRD) and RPE alterations detected through multimodal imaging techniques. According to the classification, a patient must meet both major criteria and 1 minor criterion for the diagnosis of CSCR.
The major criteria are (1) presence or evidence of prior SRD documented on optical coherence tomography (OCT) involving the posterior pole unrelated to another disease process and (2) at least 1 area of RPE alteration on fundus autofluorescence (FAF), spectral-domain OCT, or infrared imaging.
The minor criteria include mid-phase hyperfluorescent placoid areas on indocyanine angiography (ICGA), one or more focal leaks on fundus fluorescein angiography, or subfoveal choroidal thickness (SFCT) of 400 µm or greater (consider age and axial length).
The Central Serous Chorioretinopathy International Group classified CSCR into 2 major subtypes: simple and complex. Atypical variants types, such as bullous CSCR variant, RPE tear, and CSCR associated with other retinal diseases, were placed into the atypical category.
The group used a 2-disc area (DA) diameter of RPE atrophy as the threshold to classify CSCR as simple or complex (≤2 DA=simple, >2 DA=complex). Both groups (simple and complex) were further divided into primary (first known episode of SRF), recurrent (presence of SRF with history or signs of resolved episode) and resolved (absence of SRF on OCT).
According to the classification system, when SRF has been present for >6 months, it is described as persistent. Other modifiers include outer retinal atrophy (outer nuclear layer thinning and or external limiting membrane disruption and or ellipsoid zone attenuation), intraretinal fluid with or without macular neovascularization (MNV), and foveal involvement.
New Imaging Techniques and Findings
Multimodal imaging techniques have been the key for the diagnosis and assessment of patients with CSCR. Recently, OCT angiography (OCTA) allows the detection of areas of choroidal nonperfusion. In normal eyes, there are consistent OCTA signals at the level of the choriocapillaris.
There have been reported abnormal vascular signals at the choriocapillaris in eyes with CSCR. Shinojima et al showed abnormal signals at the level of choriocapillaris in 58 eyes with CSCR and 51 contralateral eyes using OCTA.
All patients with CSCR showed abnormal signals at the choriocapillaris, whereas 61% of contralateral eyes showed abnormal signals. They described the abnormal vascular signal patterns at the choriocapillaris level in CSCR eyes on OCTA as type 1, with central high-flow signal surrounded by an inner-low flow signal and an outer high-flow signal (18 eyes); type 2, with central low-flow signal surrounded by a high-flow signal (6 eyes); and type 3, with mosaic flow signal pattern (34 eyes).
They defined the “mosaic pattern” as random high-flow and low-flow portions corresponding to neither type 1 nor type 2 on OCTA images. The study noted RPE detachment/irregularities and ellipsoid zone (EZ) irregularities on OCTA in patients with abnormal vascular signals.
The role of OCTA is already established in identifying choroidal neovascular (CNV) membranes associated with CSCR, and OCTA has a 45.8% to 58.0% greater chance of detecting CNV than conventional dye-based angiography.
Previously, ICGA studies were limited to the posterior pole without peripheral imaging of the vortex veins. Widefield ICGA (WF ICGA) and ultrawidefield ICGA (UWF ICGA) has expanded the ability to extensively image up to 200 degrees with ICGA technique.
A recent hypothesis states that CSCR eyes have reduced peripheral outflow through the vortex veins. Jung et al used UWF ICGA to quantitatively demonstrate asymmetric choroidal outflow in CSCR and pachychoroid pigment epitheliopathy (PPE).
The increased brightness levels along the inferior quadrants in mid-phase ICGA showed the venous outflow congestion in CSCR/PPE.
Adaptive optics scanning laser ophthalmoscopy (AOSLO) has been used to show intraretinal hyperreflective dots (HRDs) in CSCR. The exact cellular origins of HRDs are unknown. They are thought to be debris from inflammatory responses incited by CSCR.
Hanumunthadu et al showed increased choroidal HRDs on OCT in patients with acute CSCR compared to chronic disease. In patients with acute disease, HRDs were positively correlated with age and SFCT.
In chronic disease, HRDs were positively correlated with central macular thickness and neurosensory detachment height. However, in all patient populations, they noted a negative correlation between HRDs, age, and SFCT.
Adaptive-optics ICGA has recently been employed to visualize choriocapillaris and outer retina at the cellular level. This modality may be able to provide additional details of the choriocapillaris layer.
Newer Insights on Pathophysiology
As stated above, WF-ICGA and UWF-ICGA have expanded visualization and analysis of vortex veins in defining their patterns and coverage from the central retina to the periphery. Choroidal vasculature is divided into 4 quadrants as a result of horizontal and vertical watershed zones.
Each quadrant is served by an average of 4 to 5 (range of 3 to 8) vortex veins. Recent literature has shown asymmetric dilation of vortex vein and outflow congestion in the pachychoroid spectrum of diseases.
The anastomosis of the vortex veins is hypothesized to be caused by the congestive mechanism within the choroid. Matsumoto et al, in a retrospective case series, suggested that congestion of the vortex veins might contribute to the development of anastomosis between the superior and inferior vortex veins during the course of disease progression.
In their quantitative measure of vortex veins in the posterior pole in eyes with pachychoroid, CSCR eyes had significantly larger mean diameter of vortex veins compared to polypoidal choroidal vasculopathy.
Anastomosis between superior and inferior vortex veins was observed in more than 90% of eyes with each pachychoroid spectrum disease. Overall, this venous overload theory may explain the pathophysiology for pachychoroid disease spectrum.
New Treatments
Acute CSCR presents with decreased vision, metamorphopsias, and central scotomas. Spontaneous resolution of SRF occurs in 80% of patients, especially with discontinuance (and continued avoidance) of topical, inhaled, intranasal, intraarticular, or intravenous steroids.
However, some patients can have recurrence or progression of these acute symptoms to a chronic form usually after 3 months to 6 months. Currently, most retina specialists use photodynamic therapy (PDT) with verteporfin (Visudyne; Bausch + Lomb) as well as pharmacologic therapy.
In a pivotal nonrandomized multicenter study, complete resorption of SRF occurred in 100% of 82 CSCR patients treated with full-fluence PDT with an average 12-month follow-up; reactivation occurred in only 2% of patients.
To avoid possible adverse events, half-fluence PDT has shown to be beneficial and was found to be equivalent to full-fluence PDT treatment for CSCR.
Furthermore, the multicenter PLACE trial showed that half-dose PDT was superior to subthreshold micropulse laser treatment of CSCR.
There is a current shift toward the preference of pharmacologic treatment for the management of CSCR.
The recent VICI trial was a randomized, double-blind, placebocontrolled trial of 114 patients at 22 hospitals in United Kingdom that concluded that eplerenone was not superior to placebo for improving best corrected visual acuity (BCVA) in patients with chronic CSCR after 12 months of treatment (placebo BCVA 79.5±4.5, eplerenone 80.4±4.6, adjusted mean difference of 1.73 letters; 95% CI 1.12-4.47; P=.24).
The study concluded that ophthalmologists who currently prescribe eplerenone for CSCR should discontinue the practice.
Since the VICI trial, several articles have been published that support the use of eplerenone for the management of CSCR, contradicting the recommendations of the VICI trial. In a letter to the authors, both Sacconi et al24 and StanescuSegall et al25 stated the recommendation against eplerenone was too strong due to the presence of several reports of increased efficacy of eplerenone in treating CSCR.
Fraenkel et al, in a retrospective study, assessed the morphologic and functional outcome of 30 patients with chronic CSCR treated with oral eplerenone. All patients had improved BCVA from 0.2±0.2 to 0.09±0.15 at 3 months (P=.01).
Another retrospective study by Petkovsek et al confirmed the anatomic improvement of patients with chronic CSCR within the first year of eplerenone study. Although these studies showed improvement in BCVA and anatomic markers, these studies had a small sample size and were nonrandomized in nature.
Apart from eplerenone, there has been contradicting evidence of the efficacy of numerous medical therapies in the management of CSCR. Among them are nonsteroidal antiinflammatory drugs (NSAIDs), oral propranolol, and topical carbonic anhydrase inhibitors like dorzolamide.
In a recent retrospective study by Bahadorani et al, patients diagnosed with new-onset CSCR on NSAIDs showed a faster rate of SRF reduction compared to control patients who were observed without any treatment.
In the 14 eyes treated with topical bromfenac or nepafenac, there was a significant reduction in central macular thickness (-192 µm in treated eyes and -43.5 µm in control eyes; In a randomized prospective study of 120 patients with CSCR, Chen et al showed the efficacy (95% success rate) of oral propranolol over placebo in treating patients with CSCR over a 4-month period.
Patients on oral propranolol showed complete remission in 1.9 months, whereas those receiving placebo achieved remission in 3.5 months. The recurrence rate was 5.3% in the propranolol group and 25.5% in the placebo group.
In another prospective nonrandomized study, 18 patients with chronic CSCR treated with the topical carbonic anhydrase inhibitor dorzolamide showed significant improvement in central macular thickness compared to 15 observed control patients (-145.6 µm, 95% CI -170.5 to -120.7 in the treatment group; -45.1 µm, 95% CI -65.3 to -25.1 in the control group) within the 3-month study period.
At 3 months, 77.8% patients in the treatment group and 40.0% in the control group achieved complete resolution of SRF (P=.04).
There have been numerous recent advances in the classification, diagnosis, and management of CSCR. The Central Serous Chorioretinopathy International Group classification system was created to standardize the descriptors used by ophthalmologists across the globe and helps to establish standard treatment guidelines.
The advent of newer venous congestion theory using WF imaging has added further to the understanding of this disease spectrum.
However, controversy remains around medical management of CSCR. Photodynamic therapy continues to be the mainstay treatment, although ophthalmologists have found success with numerous therapies, such as eplerenone, topical dorzolamide, NSAIDs, and oral propranolol.
(1).jpg)