What Is Strabismus? A Comprehensive Guide for All
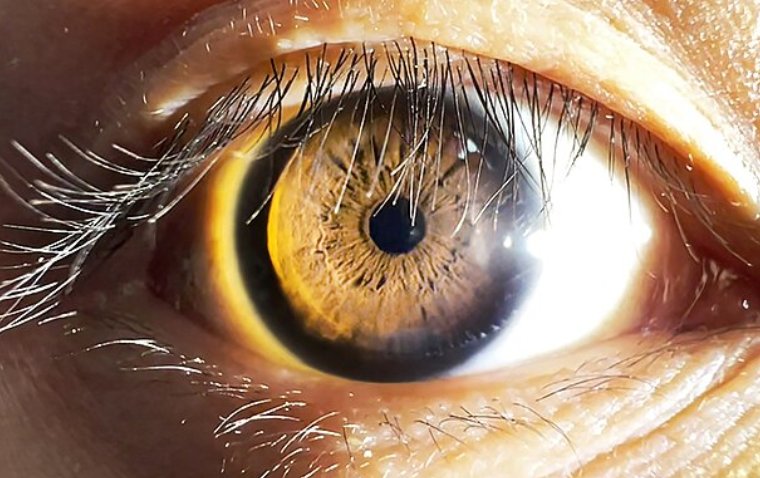
Strabismus, also known as crossed or turned eyes, is a condition where the eyes don't line up correctly. Imagine your eyes as two mischievous partners in crime, each one plotting to look in a different direction. The result? A visual mismatch that can make everyday tasks a bit more challenging.
Strabismus occurs when the eyes are unable to maintain proper alignment due to dysfunction in the ocular muscles. This misalignment can result in double vision, impaired depth perception, and, if left untreated, may cause amblyopia or vision loss in the affected eye.
Strabismus is a relatively common eye condition, affecting approximately 4% of the U.S. population. This equates to millions of individuals experiencing strabismus, highlighting the importance of early detection and treatment to prevent potential long-term vision complications.
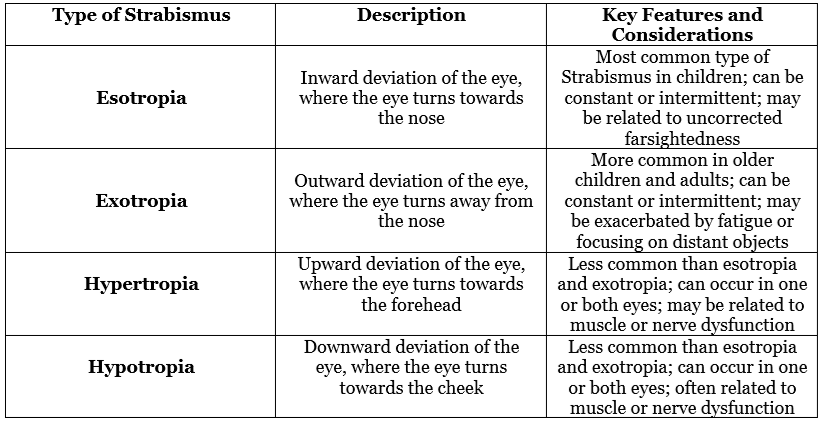
Types of Strabismus
Strabismus manifests itself in various ways, resulting in different types of misalignments. Understanding the specific type of strabismus can help tailor an effective treatment plan and address the root cause of the misalignment. In this section, we will delve into the distinct types of Strabismus, including esotropia, exotropia, hypertropia, and hypotropia, and explore their unique features and considerations.
What Causes Strabismus?
The development of strabismus can be attributed to a multitude of factors, ranging from neurological and anatomical abnormalities to congenital and acquired influences. By identifying the underlying cause of strabismus, healthcare professionals can formulate targeted treatment strategies to manage the condition effectively. In this section, we will examine the various causes of Strabismus, including neurological factors, anatomical factors, congenital factors, and acquired factors, and discuss how they contribute to this prevalent eye condition.
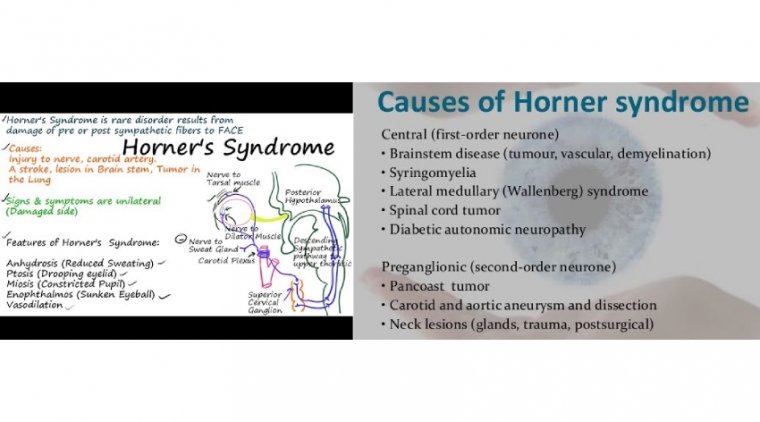
1. Neurological factors:
● Problems with eye muscle control and coordination can contribute to the development of Strabismus. This may result from issues in the brain's communication with the ocular muscles or from an imbalance in the muscles themselves. Conditions such as brain injury, stroke, or cerebral palsy can cause neurological Strabismus.
2. Anatomical factors:
● Abnormalities in the eye muscles or nerves can lead to Strabismus. For instance, some individuals may have an underdeveloped or absent muscle, while others may have nerve damage or dysfunction that disrupts the proper function of the ocular muscles. These anatomical factors can be congenital or acquired due to injury or disease.
3. Congenital factors:
● Strabismus may be present at birth, resulting from genetic factors, prenatal influences, or birth complications. In some cases, newborns may have a temporary misalignment of the eyes that resolves spontaneously within the first few months of life. However, if the Strabismus persists, early intervention is crucial to prevent long-term vision problems.
4. Acquired factors:
● Strabismus can also develop later in life due to various causes, including eye injuries, diseases that affect the eye muscles or nerves (such as thyroid eye disease or myasthenia gravis), and complications from eye surgery. Additionally, certain medications or substances that affect the nervous system can contribute to the development of Strabismus in some individuals.
Symptoms and Diagnosis of Strabismus
Strabismus can present a variety of symptoms, which can differ in severity and presentation depending on the specific type and underlying cause. Here are some of the most common symptoms associated with Strabismus:
1. Eye misalignment: One of the most noticeable symptoms of Strabismus is the visible misalignment of the eyes. This misalignment can be constant or intermittent and may be more noticeable when the individual is tired or focusing on close or distant objects.
2. Double vision (diplopia): Strabismus can cause the individual to see two images of a single object, resulting in double vision. The brain may adapt to this by ignoring the image from the misaligned eye, leading to reduced visual acuity in the affected eye.
3. Impaired depth perception: Strabismus can disrupt the eyes' ability to work together to perceive depth, making it difficult for the individual to gauge distances accurately or participate in activities that require accurate depth perception, such as sports or driving.
4. Squinting or closing one eye: To compensate for the misalignment and avoid double vision, the individual may squint or close one eye, especially in bright light or when attempting to focus on an object.
5. Eye strain or fatigue: Strabismus can lead to eye strain and fatigue, as the affected eye constantly struggles to maintain proper alignment.
6. Head tilting or turning: The individual may tilt or turn their head to a specific angle to achieve single vision and minimize the effects of the misalignment.
To diagnose strabismus, a comprehensive eye examination is necessary. An ophthalmologist or optometrist will evaluate the patient's medical history, perform a visual acuity test, and assess the eye alignment and eye movements. Special tests, such as the cover test, may be used to determine the presence and severity of strabismus. In some cases, the eye care professional may recommend additional testing to identify the underlying cause of the Strabismus, such as imaging studies or neurological evaluations.
Treatment Options for Strabismus
Complications and Prognosis
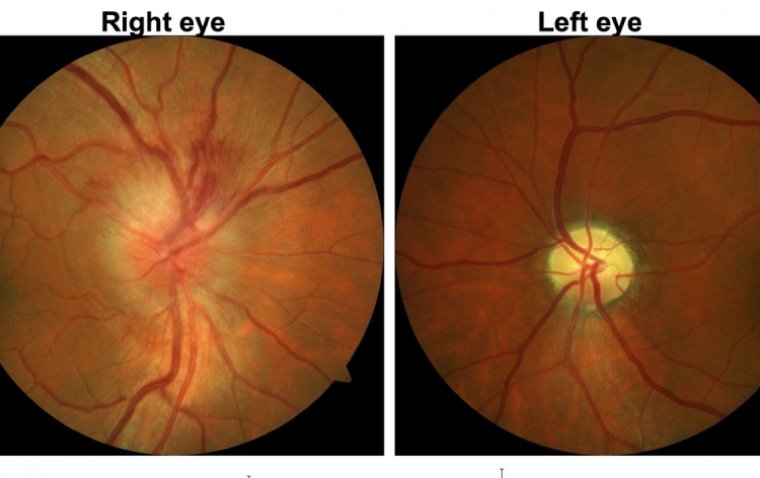
Strabismus can lead to various complications if left untreated or not managed appropriately. Here are some potential complications associated with the condition:
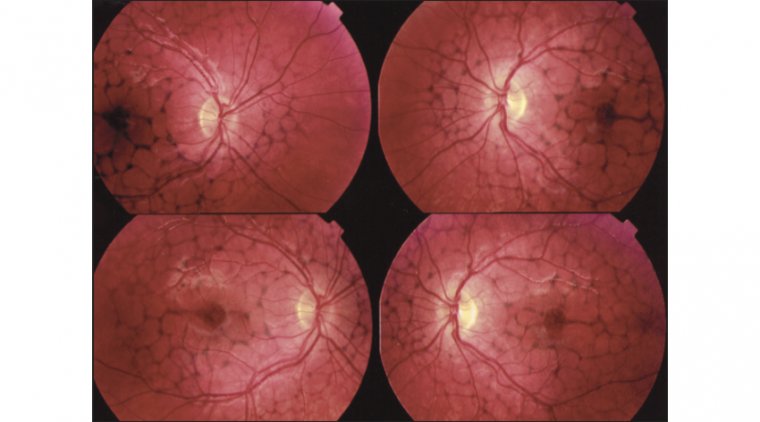
1. Amblyopia (lazy eye): In cases of strabismus, the brain may ignore the image from the misaligned eye to avoid double vision. This suppression can result in amblyopia, where the affected eye experiences reduced visual acuity due to underuse.
2. Social and psychological effects: The visible eye misalignment in strabismus can affect an individual's self-esteem and confidence, leading to social anxiety, isolation, or depression.
3. Impaired visual function: Strabismus can disrupt essential visual functions, such as depth perception and binocular vision, affecting an individual's ability to perform daily tasks, sports, or drive safely.
4. Persistent double vision: If not adequately addressed, strabismus may lead to persistent double vision, making it challenging to focus on objects and perform daily tasks.
The prognosis for strabismus largely depends on the type, cause, and severity of the condition, as well as the patient's adherence to the prescribed treatment plan. In most cases, early diagnosis and intervention significantly improve the chances of successful treatment and long-term outcomes.
Conclusion
In the world of ocular alignment, strabismus is a bit like a pair of dancers that can't quite sync their steps, causing them to zig when they should zag. But don't let the misaligned waltz of the eyes throw you off balance! With early diagnosis, intervention, and a comprehensive treatment plan, you can help your eyes find their groove again and tango in unison.
Remember, it's essential to keep an "eye" on your vision, and if you or your loved ones notice any signs of Strabismus, don't hesitate to consult a qualified eye care professional. After all, when it comes to our eyes, it's always better to be "strabismart" than sorry. So, let's set the stage for better vision and dance our way towards a clearer, more coordinated future.
(1).jpg)