Retinitis Pigmentosa Mouse Models Accurately Reflect Pathobiology of Human RP59
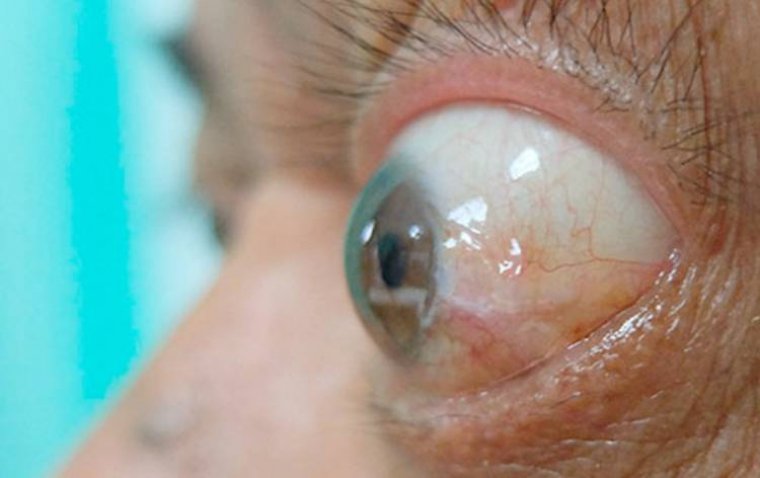
Retinitis pigmentosa (RP) is a group of inherited retinal degenerative diseases caused by mutations in nearly 100 different genes. These mutations progressively impair vision, often leading to blindness over the course of years or decades.
One subtype, known as RP59, is linked to mutations in the DHDDS gene, which encodes an enzyme involved in the protein glycosylation pathway. RP59 is inherited in a recessive manner, meaning that disease develops only when both copies of the DHDDS gene carry pathogenic mutations.
Mouse Models Developed to Study RP59 Mechanism
To better understand RP59 and explore potential therapeutic avenues, Steven Pittler, PhD, and colleagues at the University of Alabama at Birmingham (UAB) have developed genetically engineered mouse models carrying DHDDS mutations analogous to those found in humans with RP59.
Initial Mouse Model: K42E/K42E
The first model, reported in 2020 and 2023, featured a K42E/K42E mutation. This mutation substitutes lysine (K) at amino acid position 42 with glutamic acid (E) in both copies of the DHDDS gene. This mutation corresponds to one of the known human variants associated with RP59.
New Models: T206A/K42E and T206A/T206A
The latest study, published in Disease Models & Mechanisms, introduces two additional models:
• T206A/K42E (heterozygous)
• T206A/T206A (homozygous)
In these models, threonine (T) at position 206 is replaced with alanine (A). Notably, the T206A/K42E variant has been reported in human RP59 patients, while the T206A/T206A combination has not been observed clinically.
At 12 months of age, both new models showed retinal structure and function changes similar to those seen in the earlier K42E/K42E model.
Key Findings and Implications
According to Pittler, professor in the UAB Department of Optometry and Vision Science, these results strengthen the understanding of RP59 pathobiology and its underlying mechanism.
“Because T206A/K42E is one of the prevalent variants reported in RP59 patients, these findings will bring us closer to understanding the mechanism underlying this disease,” said Pittler.
The study suggests that both K42E and T206A alleles are pathogenic, likely through a shared biological mechanism. The authors propose that RP59 pathology involves:
• Defective synaptic transmission from photoreceptors to bipolar cells
• Degeneration of bipolar and amacrine cells
Retinal Layer Findings and Electrophysiological Evidence
In all three mouse models (K42E/K42E, T206A/K42E, and T206A/T206A), researchers observed:
• Thinning of the inner nuclear layer
• Reduced densities of bipolar and amacrine cells
Electroretinography (ERG) was used to evaluate retinal function. This technique measures electrical responses in retinal neurons following a flash of light:
• The a-wave, originating from photoreceptors in the outer retina, showed minimal reduction
• The b-wave, reflecting the activity of inner retinal cells like bipolar cells, showed a notable reduction
These findings reinforce the hypothesis that the primary functional disruption in RP59 lies in the inner retina, downstream from the initial photoreceptor response.
Conclusion
This research demonstrates that DHDDS mutations modeled in mice, including both common and novel allelic variants, produce retinal phenotypes closely mirroring human RP59. The results offer valuable insights into disease mechanisms and could guide future efforts in therapeutic development for this rare but severe form of inherited retinal degeneration.
Reference:
Mai N. Nguyen et al, Dhdds T206A and Dhdds K42E knock-in mouse models of retinitis pigmentosa, type 59 are phenotypically similar, Disease Models & Mechanisms (2025). DOI: 10.1242/dmm.052243
(1).jpg)