Researchers Identify Molecular Link Between HPV and Thyroid Eye Disease
Researchers from the University of Miami Miller School of Medicine have identified molecular evidence linking human papillomavirus (HPV) to thyroid eye disease (TED). The study suggests that molecular mimicry involving HPV capsid proteins and autoimmune targets such as insulin-like growth factor-1 receptor (IGF-1R) and thyroid-stimulating hormone receptor (TSHR) may influence disease development. Elevated antibody levels against HPV were observed in participants with TED, indicating a potential immunological connection.
Thyroid Eye Disease: Complex Autoimmune Features and Triggers
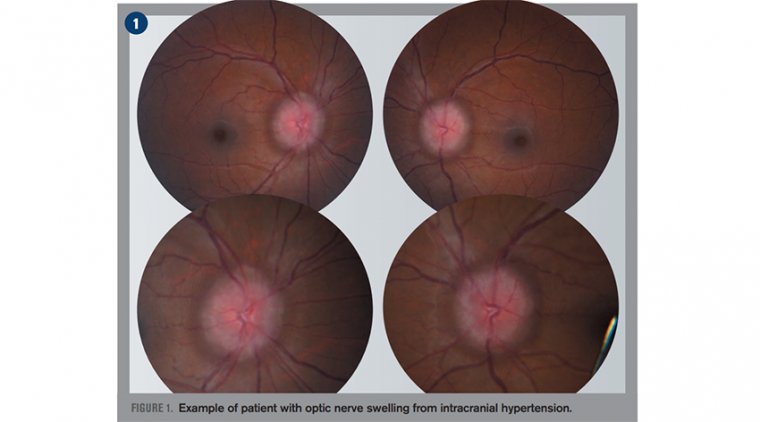
TED is characterized by complex autoimmune mechanisms with unclear triggers. Managing the varied clinical manifestations of TED remains challenging, with symptoms including proptosis, diplopia, pain, dryness, and redness. Severe cases can lead to vision loss in 2% to 5% of patients. TED affects approximately 25% to 50% of individuals with Graves disease and 3% to 5% of those with Hashimoto thyroiditis. Additionally, TED occurs in individuals with euthyroidism and hypothyroidism, suggesting that mechanisms beyond thyroid dysfunction are involved.
Autoantibodies that upregulate IGF-1R and TSHR have been primarily implicated in TED. However, TED cases without thyroid dysfunction prompted hypotheses involving molecular mimicry by pathogens. Reports of TED following COVID-19 infection further supported the theory that infectious agents could trigger autoimmune responses.
Study Overview: Exploring Viral Involvement in TED Pathogenesis
In a study titled "Human Papillomavirus and Thyroid Eye Disease," published in JAMA Ophthalmology, researchers conducted an experimental investigation into the potential role of viral infections in TED development.
Orbital adipose tissue samples were collected from 11 patients with TED undergoing orbital decompression surgery and 11 control patients undergoing blepharoplasty. The study cohort had a mean age of 58.6 years (range: 37.4–74.4 years), with female patients comprising 86.4% of the group.
Molecular Homology Analysis and Antibody Testing
Researchers utilized the Basic Local Alignment Search Tool (BLAST) from the National Center for Biotechnology Information (NCBI) to perform protein homology analysis, comparing IGF-1R and TSHR sequences against viral proteomes. Enzyme-linked immunosorbent assays (ELISAs) measured HPV18 L1 immunoglobulin G (IgG) levels from the collected orbital adipose tissue samples. Optical density (OD) readings from the ELISAs were used to estimate antibody binding levels.
Protein homology analysis revealed that IGF-1R and TSHR shared homologous sequences with major capsid proteins from several viral families, including Papillomaviridae, Paramyxoviridae, Herpesviridae, Enteroviruses, Polyomaviridae, and Rhabdoviridae. Two conserved motifs, FGXV and IXEXT+NP, were identified across all HPV serotypes and in both IGF-1R and TSHR sequences.
Elevated HPV Antibody Levels in TED Patients
Analysis of ELISA results showed:
• Control group: Mean normalized OD = 0.94
• Chronic TED group: Mean normalized OD ≈ 2.31
• Acute active TED group: Mean normalized OD ≈ 4.09
Both TED groups demonstrated significantly higher normalized OD levels compared with controls, with the acute active TED group displaying the highest antibody levels.
No correlations were found between HPV18 L1 IgG levels and thyroid-stimulating hormone (TSH), free thyroxine (FT4), or thyroid-stimulating immunoglobulin (TSI) levels. Furthermore, treatments such as radioactive iodine, thyroidectomy, or therapy with teprotumumab did not affect antibody levels.
Conclusion: Viral Mimicry as a Potential Contributor to TED
Researchers concluded that viral molecular mimicry between HPV and key autoimmune targets (IGF-1R and TSHR) could contribute to TED development. Elevated antibodies against HPV18 L1 capsid protein in patients with TED suggest a potential immunological mechanism influencing disease pathogenesis.
The identification of viral mimicry offers new opportunities for preventive strategies and therapeutic approaches. Although the cohort size was small and causation was not established, recognizing viral exposure as a contributing factor could shape future diagnostic and treatment research for TED.
Reference:
Ishita Garg et al, Human Papillomavirus and Thyroid Eye Disease, JAMA Ophthalmology (2025). DOI: 10.1001/jamaophthalmol.2025.0847
(1).jpg)