Cellular Response in Eye Drainage System May Inform Glaucoma Treatments
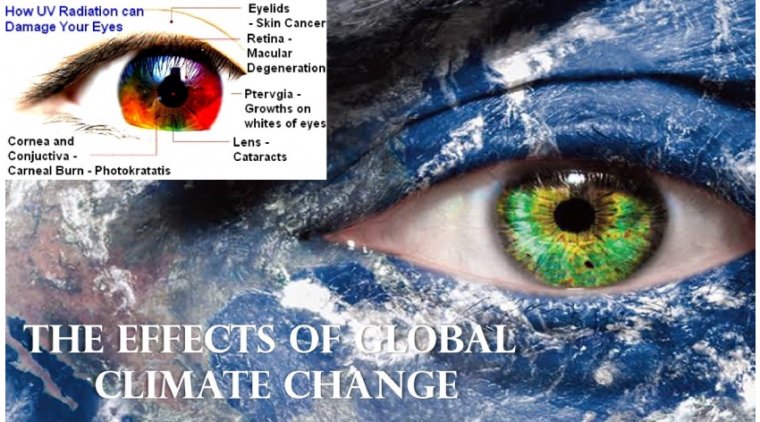
A recent study published in Matter provides new insight into how cells within the eye's drainage system respond to physical forces, potentially unlocking new pathways for the treatment of glaucoma, a leading cause of irreversible blindness.
Investigating the Cellular Mechanics Behind Elevated Intraocular Pressure
The research was led by Alireza Karimi, Ph.D., assistant professor of ophthalmology and biomedical engineering at the Oregon Health & Science University (OHSU) School of Medicine and Casey Eye Institute. The study examined the behavior of cells in the trabecular meshwork (TM), the tissue responsible for fluid drainage in the eye and a key regulator of intraocular pressure (IOP).
Elevated IOP is the primary risk factor for glaucoma, a disease projected to affect over 112 million people worldwide by 2040. While the connection between fluid drainage and glaucoma progression is well recognized, the underlying biological mechanisms remain poorly understood.
Key Findings: ECM Stiffness Influences TM Cell Behavior
Using advanced experimental and computational techniques, the researchers focused on how extracellular matrix (ECM) stiffness influences the mechanical response of TM cells in both healthy and glaucomatous eyes. The ECM provides structural support to cells and plays an active role in modulating fluid outflow resistance.
The study revealed a distinct difference in how healthy and glaucomatous TM cells respond to ECM stiffness:
• In healthy eyes, increased ECM stiffness led to stronger contractile forces by TM cells.
• In glaucomatous eyes, TM cells exerted greater forces in response to softer ECM—an inverse response pattern compared to healthy cells.
This aberrant behavior suggests that high-flow regions in glaucomatous eyes contain less stiff cells than those in normal eyes. The finding was corroborated using atomic force microscopy, reinforcing the idea that changes in cell-ECM dynamics contribute to impaired fluid drainage and elevated IOP in glaucoma.
Technological Innovation: Real-Time 3D Force Measurement
One of the major innovations of the study was the use of a novel experimental-computational technique that allowed researchers to monitor 3D contractile forces in real time without detaching the cells from the ECM. Traditional techniques often disrupt natural cell behavior by separating the cells from their surrounding matrix.
By maintaining the native cell-ECM interface, the research team achieved a more accurate and dynamic model of cellular responses over time. This approach also offers applicability beyond ophthalmology, with potential relevance to fields such as cancer research, where ECM stiffness plays a similar role in cell behavior.
Implications for Glaucoma Drug Development
According to Karimi, these findings offer a valuable framework for identifying targeted drug therapies that could better modulate TM cell behavior and reduce IOP. He noted that current glaucoma treatments—primarily eye drops—require frequent administration, often resulting in poor adherence and suboptimal outcomes.
"We now have a framework to study targeted therapies for more effective and easier-to-administer treatments," Karimi stated. "Our next study will focus on specific drug interventions that leverage this new understanding."
Reference:
Matrix Stiffness Regulates Traction Forces, Cytoskeletal Dynamics, and Collagen Reorganization in High-Flow Trabecular Meshwork Cells in Glaucoma, Matter (2025). DOI: 10.1016/j.matt.2025.102094.
(1).jpg)