Human iPSC-Based Study Identifies Key Defects and Potential Therapies for AMD and Related Macular Dystrophies
A recent study led by Sonal Dalvi, PhD, has identified the key defect responsible for the development of age-related macular degeneration (AMD) and associated macular dystrophies (MDs) such as Sorsby’s fundus dystrophy, Doyne honeycomb macular dystrophy, and autosomal dominant radial drusen. The findings, published by a team from the University of Rochester, shed light on the role of matrix metalloproteinase 2 (MMP2) secreted by retinal pigment epithelium (RPE) cells in promoting drusen formation, a hallmark of these conditions.
Key Findings of the Study
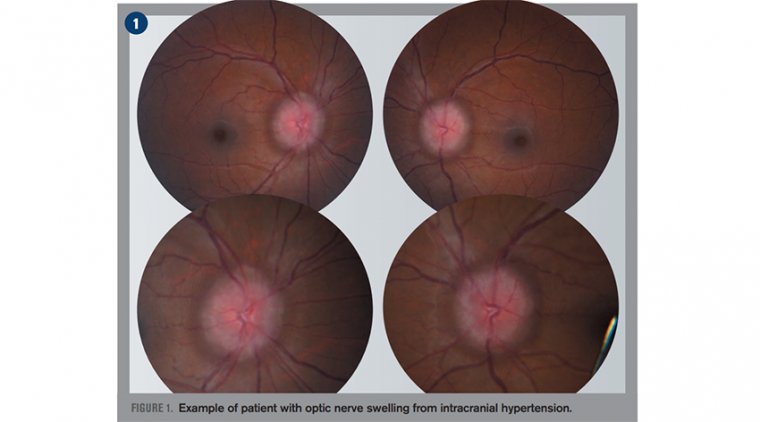
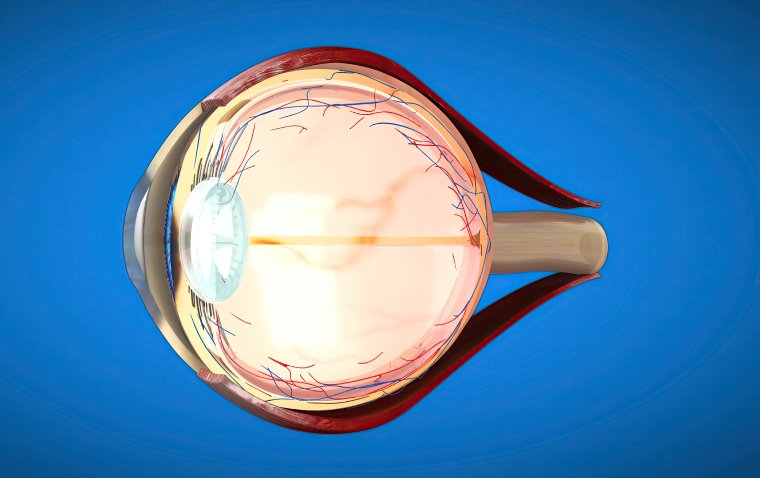
Dalvi and her colleagues demonstrated that reduced activity of MMP2 secreted from the RPE contributes to drusen formation in AMD and MDs. These conditions manifest primarily in the RPE-choriocapillaris complex of the eye, where Bruch’s membrane plays a critical role in disease development. Bruch’s membrane, which lies under the RPE, undergoes turnover regulated by proteases like MMPs, particularly MMP2, MMP3, and MMP9.
Mechanism of Disease Development
Using human induced pluripotent stem cell (iPSC)-derived RPE from patients with AMD and three MDs, the researchers found that reduced MMP2 activity leads to several pathological changes:
•Formation of drusen (yellow deposits under the retina)
•Impaired RPE barrier integrity
•RPE atrophy
•Induction of sterile inflammation and disrupted lipid homeostasis
The research points to a mechanism involving damage-associated molecular patterns (DAMP) that activate the receptor for advanced glycation end-products (RAGE), which in turn increases secretory phospholipase 2-IIA (sPLA2-IIA) levels.
Therapeutic Potential
The study also explored potential therapies targeting the MMP2-DAMP-RAGE-sPLA2-IIA axis. Dalvi’s team showed that drusen accumulation could be mitigated using a combination of treatments, including:
•RPE-specific MMP2 supplementation
•RAGE-antagonistic peptides
•Small molecule inhibitors of sPLA2-IIA
These treatments, tested in iPSC-derived RPE models of AMD and macular dystrophies, hold promise for slowing disease progression in patients.
Key Takeaways
•Shared Mechanistic Defect: Both AMD and MDs share a common defect involving reduced MMP2 activity.
•Cellular Pathology: The reduction in MMP2 triggers cellular events that drive maculopathy.
•Therapeutic Targets: Pharmacologic interventions aimed at the MMP2-DAMP-RAGE-sPLA2-IIA pathway show promise in addressing AMD and related MDs.
This study provides crucial insights into the molecular mechanisms of AMD and MDs, opening the door to more targeted treatment options for these blinding diseases.
(1).jpg)