Charles Bonnet Syndrome (CBS) & Children
Charles Bonnet syndrome (CBS) is characterized by the presence of complex visual hallucinations in psychologically healthy but visually impaired people. It has been well described in the adult population but has been less well characterized in children.
Charles Bonnet syndrome causes a person whose vision has started to deteriorate to see things that aren’t real (hallucinations). The hallucinations may be simple patterns, or detailed images of events, people, or places.
They’re only visual and don’t involve hearing things or any other sensations. It’s important to be aware that hallucinations associated with Charles Bonnet syndrome are caused by failing eyesight. They’re not caused by a mental health problem or dementia.
Charles Bonnet syndrome (CBS) is seen in individuals who are experiencing sight loss, with no psychiatric or cognitive basis. It was first described by Swiss philosopher Charles Bonnet in 1760, whose father was troubled by these symptoms after losing his sight. Δ
Since then it has been mostly associated with the elderly, reflecting the mean age at which common underlying conditions, such as age-related macular degeneration, diabetic retinopathy, and glaucoma occur.
It has an estimated prevalence of 11–15% of adults accompanying any form of visual impairment. However, CBS can affect individuals of any age including children, and so having an awareness will improve the detection and management of symptoms.
Case Series
In a recent publication in the British Journal of Ophthalmology, it has been identified the largest series of 13 pediatric and young adult patients from electronic patient records over 9 years presenting to Moorfields Eye Hospital NHS Foundation Trust in London.
Nearly 70% were male and the median age of onset was 11 (range 9–19) years old. Most patients had significantly reduced vision, with best-corrected visual acuity in the better eye being 0.81 LogMAR.
It may be possible to identify the at-risk cohort, as over 60% of patients were diagnosed with an inherited retinal disease. The most prevalent cause was Stargardt disease, which is the commonest childhood macular dystrophy. Others included Usher syndrome, Batten disease, and Leber congenital amaurosis.
The remaining cases were affected with congenital eye disorders, including microphthalmia and ocular coloboma, or optic nerve pathologies, such as bilateral optic atrophy secondary to spontaneous intracranial hemorrhage and a hereditary optic neuropathy. Δ
There was no clear correlation between visual dysfunction (e.g., loss of central vision versus peripheral visual field loss) and CBS, hence there should be no visual acuity or functionality threshold before physicians enquire about CBS symptoms.
In the published case series, clinicians-in-training were the most frequent reporting healthcare professional, followed by optometrists, then consultant-grade.
Children presenting with these developmental eye disorders are likely to be managed in tertiary referral centers within specialist services, and so we need to raise professional awareness amongst ophthalmologists and allied health care professionals, including orthoptists and optometrists (especially those specializing in low vision services) of the importance of informing families about CBS as well as encourage them to enquire about symptoms.
Management and Cause
The visual hallucinations may not necessarily manifest in the initial stages of the disease but could trigger during the active sight loss phase.
Hence, forewarning patients and families with information on CBS and hallucinatory experiences, including strategies for symptom management and sources of emotional support, may reduce the psychological impact if they do develop symptoms.
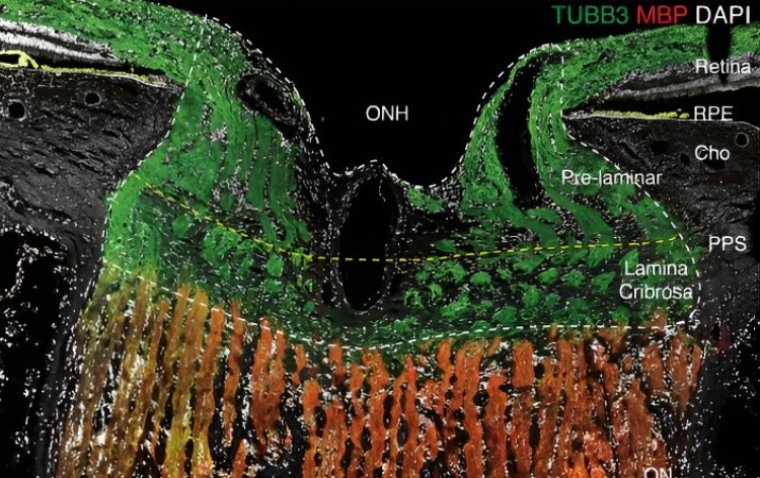
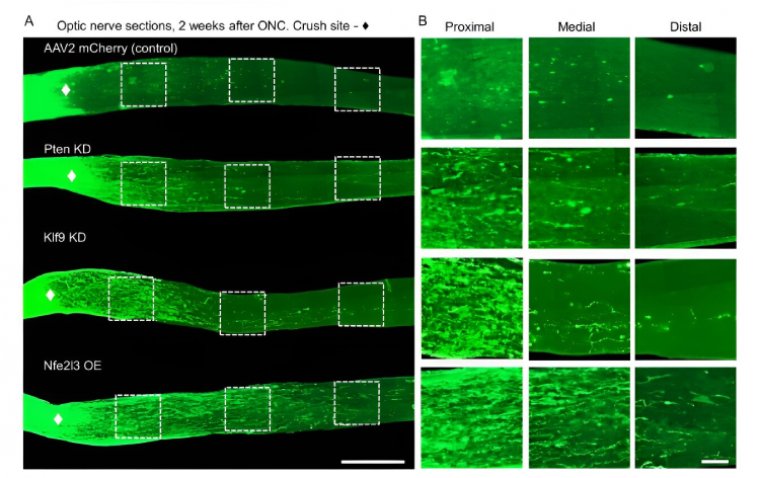
The cause of these visual hallucinations is still unknown; current thinking suggests that reduced visual input due to systemic or retinal dysfunction results in spontaneous hyperexcitability and disinhibition of the visual cortex, resulting in these experiences.
The spectrum of visual hallucinations ranges from simple geometric patterns and landscape scenes to more complex images with small figures or people, objects, and distorted faces.
The majority of children reported simple hallucinations, but two had more complex hallucinations and in a significant proportion it affected their personal lives including education, diet, and sleep.
It has previously been suggested that children believe their hallucinations to be real, hence they are more susceptible to maladaptive responses such as fear and distress.
This contrasts with adults, who do not always feel troubled by their hallucinations, since most individuals are aware that the images they are seeing are not real. Further research on the psychological impact of CBS in pediatric and adolescent patients is warranted.
The clinical management of CBS involves the implementation of simple yet effective psychological coping strategies, including brain shunting exercises such as frequent blinking or rapid eye movements, attempting to touch or brush away hallucinations, moving to brightly lit areas, and increasing social interactions. Δ Δ
Families should be linked to local family support services and any patient can access support groups such as Esme’s Umbrella (www.charlesbonnetsyndrome.uk).
Future Directions
We know there is consistent under-reporting of symptoms and difficulty with case ascertainment; this is arguably a shortcoming of current pediatric ophthalmology services.
The whole multidisciplinary team must raise awareness of CBS with children, and actively ask patients or families about symptoms.
We are now conducting a prospective study to try to ascertain the prevalence of CBS in the pediatric population across the UK with the support of the British and Irish Orthoptic Society and the Thomas Pocklington Trust.
Further research into CBS is required in order to gain a deeper understanding of the cause and how best to manage symptoms. Natural history studies into the longevity of visual hallucinations, especially in childhood, will also help when advising parents of the future prognoses of their children.
(1).jpg)