Study Suggests New Treatment Approach for Wet AMD
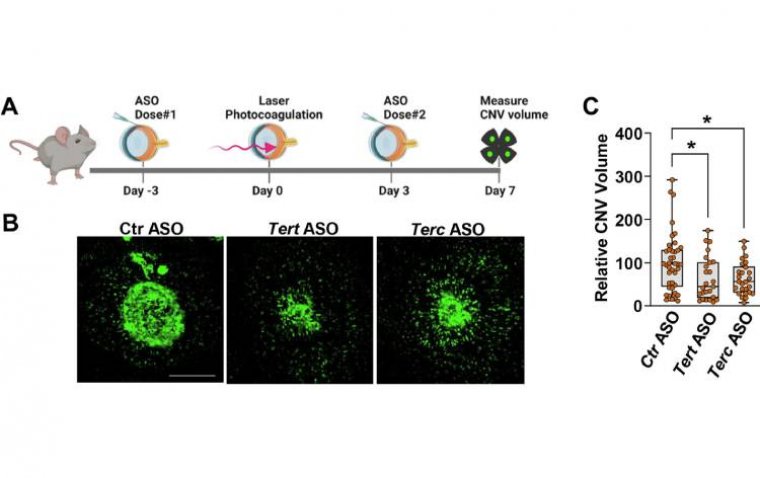
A recent study conducted on mice has provided promising insights into a potential alternative treatment for the "wet" version of age-related macular degeneration (AMD). Researchers identified an enzyme, telomerase, which plays a critical role in the abnormal blood vessel growth that characterizes wet AMD, leading to blurred central vision.
Experimental Drug Targets Telomerase, Suppresses Blood Vessel Invasion
Published in the journal Biochimica et Biophysica Acta (BBA)—Molecular Basis of Disease, the study demonstrated that targeting telomerase with an experimental drug effectively suppressed the invasive growth of new blood vessels in the retina of mice. This finding is significant as current treatment options for wet AMD primarily involve injections that inhibit the activity of vascular endothelial growth factor (VEGF), which stimulates the formation of abnormal blood vessels.
Combining Therapeutic Approaches
Dr. Nagaraj Kerur, senior study author and associate professor of ophthalmology and visual sciences at The Ohio State University College of Medicine, highlighted the limitations of existing treatments: "Anti-VEGF treatment has shortcomings—after two years, about half of people stop responding. And patients can develop scarring under the retina. There is a need for better understanding of the mechanisms behind this problem, which, to me, means newer targets need to be tested."
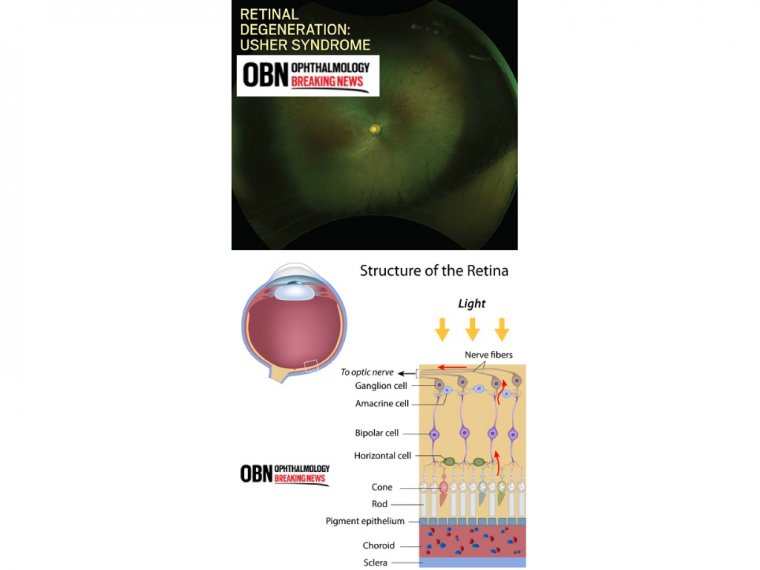
Dry AMD vs. Wet AMD: Two Distinct Pathologies
Dry AMD, which constitutes about 80% of all AMD cases, involves the thinning of the macula and buildup of proteins that lead to cell death and central vision impairment. In contrast, wet AMD, or neovascular AMD, is characterized by the abnormal growth of new blood vessels in the retina, which can leak and cause inflammation, further deteriorating vision.
The study's findings indicated that telomerase inhibition could potentially offer a new therapeutic approach. Researchers observed that mice lacking telomerase genes exhibited significantly reduced abnormal blood vessel growth following induced laser injury compared to control mice.
Moreover, experiments with an experimental compound that inhibits telomerase activity showed promising results. The drug effectively reduced telomerase activity in healthy mice and, when injected into mice with symptoms resembling wet AMD, significantly curtailed the invasion of abnormal blood vessels into the retina.
Future Directions
Dr. Kerur emphasized the study's implications for future treatments: "Telomerase inhibition by itself can also be pursued independently, and that is the plan." He noted that combining telomerase inhibition with current anti-VEGF treatments at lower doses yielded the most effective therapeutic outcomes in the study's experiments.
The researchers concluded that further investigation into telomerase inhibition as a standalone therapy and in combination with existing treatments could lead to improved outcomes for patients with wet AMD.
Reference
Aman Kumar et al, Therapeutic targeting of telomerase ameliorates experimental choroidal neovascularization, Biochimica et Biophysica Acta (BBA)—Molecular Basis of Disease (2024). DOI: 10.1016/j.bbadis.2024.167156
(1).jpg)