Landmark Research Proposes Ranibizumab Over Laser for ROP Treatment
A study led by a University at Buffalo researcher has the potential to revolutionize the treatment of retinopathy of prematurity (ROP), a condition that can lead to blindness in low birthweight premature infants if left untreated.
Published in eClinicalMedicine, the study addresses a longstanding question about the safest and most effective treatment for ROP. The international randomized clinical trial, named RAINBOW, compared the efficacy and safety of ranibizumab with the traditional laser therapy for very low birthweight infants suffering from ROP.
Laser Therapy vs. Anti-VEGF
For decades, laser therapy has been the standard treatment for ROP. This procedure involves burning the peripheral retina to halt the growth of abnormal blood vessels. However, it is physically demanding for both the clinician and the infant, often taking at least 60 minutes per eye and potentially requiring general anesthesia or heavy sedation. Children who undergo laser therapy may develop nearsightedness and lose peripheral vision as they grow older.
In 2011, the BEAT-ROP study published in the New England Journal of Medicine introduced anti-vascular endothelial growth factor (anti-VEGF) agents as a possible alternative. These agents, which can be administered via intravitreal injection at the bedside with topical anesthesia, showed promise in treating ROP by suppressing excessive VEGF levels.
"That paper caused a sensation," recalls Dr. James D. Reynolds, the senior author of the new study and the Jerald and Ester Bovino Professor and Chair of the Department of Ophthalmology at the Jacobs School of Medicine and Biomedical Sciences at UB. He also penned the editorial that accompanied the NEJM publication in 2011.
The BEAT-ROP study found that bevacizumab, an anti-VEGF agent, was as effective as laser therapy. However, safety concerns emerged due to the potential for these molecules to enter the bloodstream and harm the developing brain. This controversy kept laser therapy as the gold standard until now.
Introducing Ranibizumab: A Proven Safe Agent
"Our study using ranibizumab should end this safety controversy," asserts Reynolds. "Ranibizumab is a smaller molecule with a much shorter serum half-life than bevacizumab and does not lower plasma VEGF. Intravitreal ranibizumab (IVR) is at least as effective as laser therapy, may even be superior, and is systemically safe. Ranibizumab is now the proven safe agent."
The RAINBOW trial involved 201 children, with 156 followed for five years. This was the first study to assess visual acuity— the ability to distinguish objects and shapes at a distance— after anti-VEGF treatment. The findings indicated that visual acuity in five-year-old children treated with ranibizumab was at least as good as in those who received laser therapy.
No adverse effects were observed in visual function or a range of non-ocular outcomes, including neurodevelopment, gross motor function, growth, blood pressure, or respiratory function.
Future Research
Reynolds continues to advance research in this field, currently focusing on the impact of imaging on treatment timing for ROP. This ongoing research aims to further refine and optimize treatment protocols for this vulnerable population.
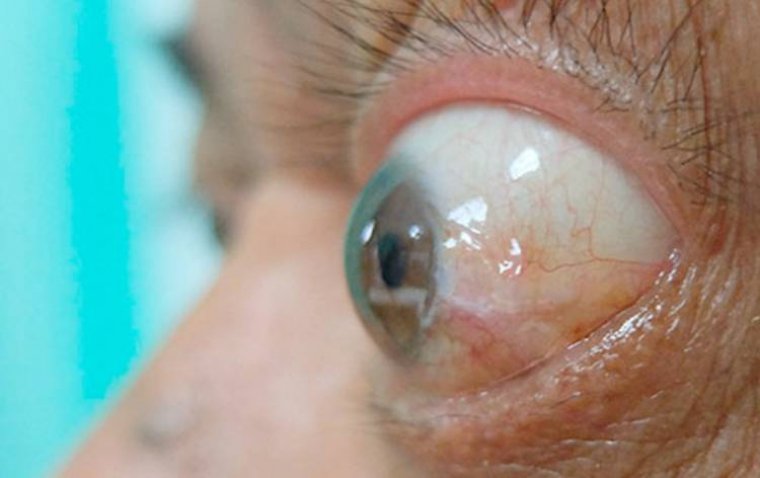
Understanding Retinopathy of Prematurity
Retinopathy of prematurity (ROP) is a potentially blinding eye disorder that primarily affects premature infants with low birthweight. It is characterized by abnormal blood vessel development in the retina, the light-sensitive layer at the back of the eye. Normally, retinal blood vessels develop gradually and reach maturity around the time of a full-term birth. However, in premature infants, this process can be disrupted, leading to the growth of abnormal, fragile vessels that can leak or cause scarring. If left untreated, ROP can progress to retinal detachment and permanent blindness. The condition necessitates early screening and timely intervention to preserve vision, typically involving laser therapy or anti-vascular endothelial growth factor (anti-VEGF) treatments.
Reference
Neil Marlow et al, Ranibizumab versus laser therapy for the treatment of very low birthweight infants with retinopathy of prematurity (RAINBOW): five-year outcomes of a randomised trial, eClinicalMedicine (2024). DOI: 10.1016/j.eclinm.2024.102567
(1).jpg)