Research Reveals Hidden Visual Deficits and Neural Pathway Alterations in Mild TBI Patients
A groundbreaking study led by Vanderbilt University Medical Center has unveiled subtle changes in the visual pathways of individuals with chronic mild traumatic brain injury (TBI). These findings highlight structural and functional deficits, even when standard eye examinations reveal no abnormalities.
The Prevalence of Visual Deficits in Mild TBI
Mild TBI accounts for approximately 3 million cases annually in the United States. Despite being classified as "mild," its impact on visual health is significant:
• Up to 85% of TBI patients report visual disturbances, such as:
- Light sensitivity
- Blurred vision
- Difficulty reading
• Persistent symptoms, including memory issues, irritability, and slowed cognitive processing, frequently affect the quality of life.
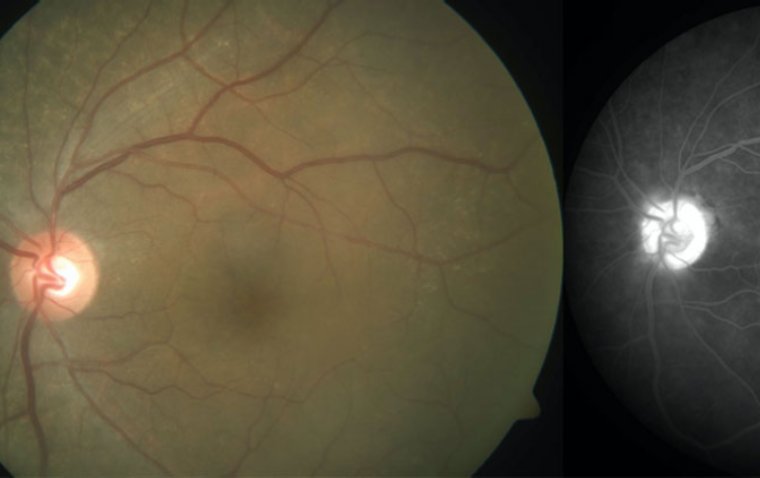
Standard clinical evaluations, like fundus examinations, often fail to detect these issues, leaving many patients without a clear diagnosis.
Key Findings from the Case-Control Study
The study, titled "Primary Visual Pathway Changes in Individuals With Chronic Mild Traumatic Brain Injury" and published in JAMA Ophthalmology, revealed that:
• 78% of mild TBI participants exhibited visual deficits when subjected to comprehensive testing.
• 70% of participants showed changes in the optic radiations and occipital lobe regions, identified through machine-learning analyses, even when self-reported visual symptoms were absent.
Study Design and Testing Methods
Researchers compared 28 individuals with mild TBI to 28 controls without brain injury using a wide range of diagnostic tools:
• Visual and Oculomotor Tests: Oculomotor function, visual field performance, and contrast sensitivity.
• Neurophysiological Assessments: Visual evoked potentials (VEPs).
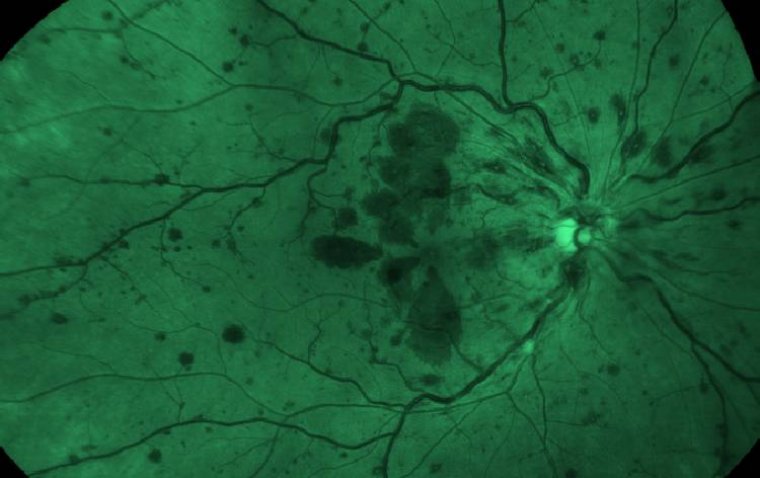
• Retinal Imaging: Retinal structure analysis via optical coherence tomography (OCT).
• Brain Imaging: MRI diffusion imaging and tractography to study microstructural and macrostructural changes.
Notable Structural and Functional Deficits
The study identified specific changes in mild TBI patients:
• Oculomotor Function Deficits:
- Reduced prism convergence breakpoints and recovery points.
• Contrast Sensitivity: Decreased in many participants.
• VEPs: Increased binocular summation index.
• Retinal Changes:
- Reduced peripapillary retinal nerve fiber layer thickness.
- Enlarged optic nerve/sheath size.
• Cortical Changes:
- Volume alterations in the occipital regions of the brain.
Implications of the Findings
The study underscores the need for comprehensive diagnostic assessments for visual dysfunction in mild TBI patients. While changes in the visual pathway were present in varying degrees across participants, many were independent of self-reported symptoms, suggesting that:
• Visual deficits in mild TBI are often hidden during routine eye exams.
• Advanced testing methods, including imaging and functional assessments, are essential for detecting these subtle alterations.
These findings highlight the importance of early diagnosis and tailored interventions to manage visual impairments and improve the quality of life for individuals with mild TBI.
This research paves the way for enhanced understanding and clinical care for TBI-related visual dysfunction, emphasizing the importance of a multidisciplinary approach to diagnosis and treatment.
Resources:
Marselle A. Rasdall et al, Primary Visual Pathway Changes in Individuals With Chronic Mild Traumatic Brain Injury, JAMA Ophthalmology (2024). DOI: 10.1001/jamaophthalmol.2024.5076
Madeleine K. Nowak et al, Visual Deficits in Patients With Mild Traumatic Brain Injury, JAMA Ophthalmology (2024). DOI: 10.1001/jamaophthalmol.2024.5121
(1).jpg)